Abstract
Introduction: Sickle cell anemia (SCA) presents a chronic inflammatory condition associated with vaso-occlusive painful episodes and intravascular hemolysis. For the innate response, a family of cellular receptors called Toll-like receptors (TLRs) has multiples functions, which may lead to several different pathways that can modulate the SCA pathogenesis. For example, TLR expression is not restricted to leukocytes, but has been reported in multiple cell types, including endothelial cells, implying that the role of the TLR pathway may not be limited to immune response. TLRs are thought to play important role in the maintenance of the inflammatory status observed in these patients. We aim to evaluate the role that lysed red blood cells (RBC) from SCA patients play in TLR2, TLR4, TLR5 and TLR9 gene expression in peripheral blood mononuclear cells (PBMC) in presence or absence of hydroxyurea (HU).
Methods: Ten SCA patients in steady-state (age 10.3 ± 4.6 years) and 7 healthy volunteers (age 14.5 ± 5.2 years) were recruited at the Fundação de Hematologia e Hemoterapia da Bahia (HEMOBA). PBMC were isolated from one healthy donor for cell cultures challenged by lysed RBC of SCA patients (SS-RBC) and RBC of healthy volunteers (AA-RBC), in presence or absence of HU. TLRs gene expressions were performed by qPCR. Serum biochemical analysis was evaluated using commercially available biochemical kits. This study was approved by the Research Ethics Committee of the Oswaldo Cruz Foundation, and was developed in accordance with the Declaration of Helsinki of 1975 and its revisions. All subjects or their legal guardians agreed to collect the biological sample after read and sign the informed consent.
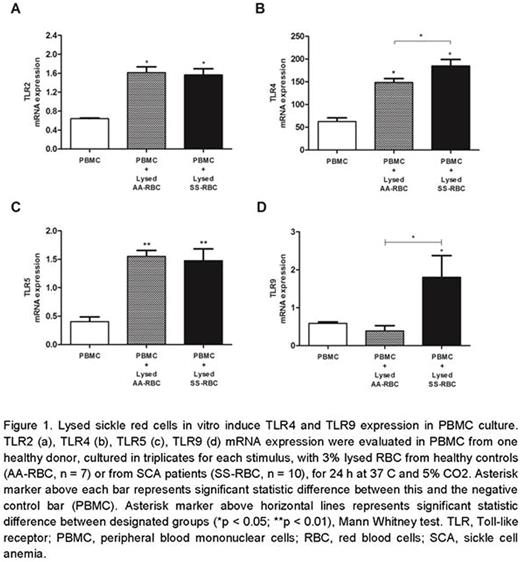
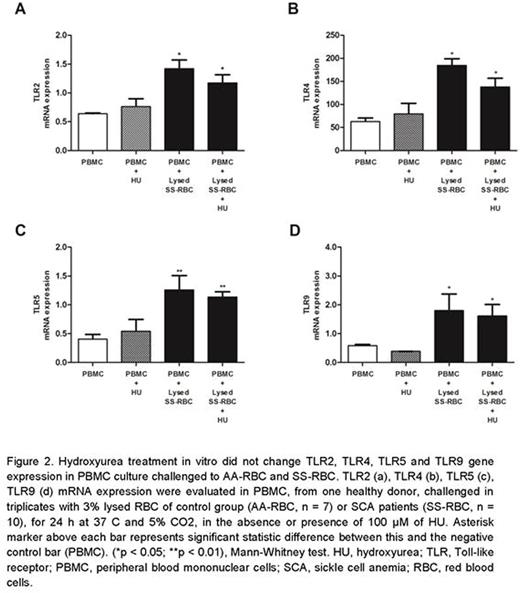
Results: We observed that TLR4 (185.0 ± 37.51, p=0.0167) and TLR9 (1.80 ± 1.51, p=0.0394) were higher expressed in PBMC culture challenged by lysed SS-RBC than by lysed AA-RBC (148.5 ± 21.43, p=0.0238; 0.38 ± 0.29, p=0.3429 respectively), whereas PBMC challenged by lysed SS-RBC had TLR2 (1.56 ± 0.34, p=0.0167) and TLR5 (1.48 ± 0.50, p=0.0043) gene expression similar to lysed AA-RBC (1.61 ± 0.30, p=0.0238; 1.55 ± 0.23, p=0.0079 respectively). Surprisingly, HU treatment did not modulate TLR expression. It is known that hemolytic byproducts such as heme and hemoglobin are able to bind TLR4 and TLR9.
Conclusion: Despite the global relevance of SCA, mechanisms that contribute to the disease severity and heterogeneity are poorly understood, even though that is the same underlying genetic mechanism. In an attempt to contribute to the field, our data reinforce the hypothesis that lysed RBCs, especially lysed SS-RBCs, act as danger signals, stimulating TLR expression and contributing to inflammation. This study highlighted that HU does not prevent TLR-dependent inflammation, pointing out the need to develop new drugs that act with different mechanisms of action of those observed for HU.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.