Abstract
Identification of prognostic indicators to predict outcomes of hematopoietic cell transplantation (HCT) is important for selection of patients most likely to benefit from the procedure. Widely validated systems such as the HCT-Comorbidity Index (HCT-CI) and the modified EBMT risk score provide consistent prediction of outcomes, in particular non-relapse mortality (NRM) and survival. In this retrospective study we identified neutropenia prior to initiation of conditioning regimen as an additional prognostic factor in 117 adults with high risk acute myeloid leukemia (AML) who received HCT at a single institution from January 2005 to December 2015. The main endpoints of the study were day 100 non-relapse mortality and survival at 5 years.
The median age at HCT was 50 years (range 21-68); 65% had an EBMT score of ≥4. In total 107 (91%) patients had poor risk disease, with classification for poor risk including; patients undergoing HCT due to failure to achieve complete remission (CR) after induction chemotherapy, patients in 2nd CR, patients in 1st CR with adverse karyotype, patients with standard karyotype but with a FLT-3 mutation, patients with measurable residual disease (MRD) by immunophenotyping or molecular monitoring and patients with secondary AML. Conditioning was myeloablative (Cy-TBI: N=41, Bu-Cy: N=3) for patents younger than 51 years with good performance status; the intensity of conditioning was reduced for the others (N=73). Standard methotrexate and cyclosporine was used as graft versus host disease prophylaxis in recipients of sibling cells, and unrelated graft recipients also received alemtuzumab.
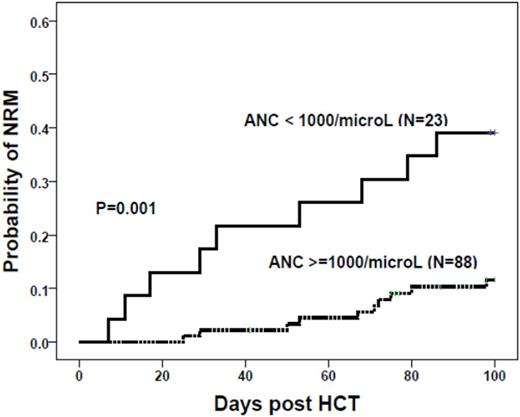
With a median follow-up of 3.1 years (range 0.3 - 10.0), day 100 NRM for the whole group was 17.3% (95% confidence interval (CI) 11 - 25) and the probability of survival at 5 years was 40.3% (95% CI 31 - 50). The effects of patient, disease and transplant factors were analysed in univariate analyses on both NRM and survival. Significant factors were then entered into multivariate analyses which yielded significant associations with improved NRM for preconditioning absolute neutrophil count (ANC) >= 1000/microL and HCT-CI < 3 (Figure) (hazard ratio (HR) 0.36; 95% CI 0.1 - 0.9 and HR 0.39; 95% CI 0.2 - 0.9 respectively). The factors associated with improved survival in multivariate analysis included preconditioning neutrophil count >= 1000/microL (HR 2.9; 95% CI 1.6 -5.4, P= 0.01), absence of any measurable disease prior to conditioning (HR 2.1; 95% CI 1.1 -4.2, P= 0.03), and less than 2 disease risk defining criteria (HR 15.8; 95% CI 2.0 -124.4, P= 0.01).
In conclusion, patients with ANC of 1000/microL and above prior to initiation of conditioning and those with HCT-CI below 3 had significantly better day 100 NRM. ANC of 1000/microL or above was also associated with better survival at 5 years together with disease specific factors, absence of measurable residual disease prior to initiation of condition and less than two adverse prognostic factors. A simple measurement such as the neutrophil count helps to predict outcome: this might reflect the presence of on-going disease but it is also possible that delaying transplant until neutrophil count recovery might impact favourably on the results. Our findings therefore advocate integration of preconditioning neutrophil count into existing risk assessment tools when considering HCT.
Milojkovic:Bristol Myers Squibb: Honoraria; Pfizer: Honoraria; Ariad: Honoraria; Novartis: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.