Abstract
Introduction
Hepatic veno-occlusive disease, also called sinusoidal obstruction syndrome (VOD/SOS), is an unpredictable, potentially life-threatening complication of conditioning for hematopoietic stem cell transplant (HSCT). Reported mean incidence of VOD/SOS following HSCT is an estimated 13.7% (range 0%-62.3%). VOD/SOS with multi-organ dysfunction (MOD) may be associated with >80% mortality. Endothelial cell (EC) damage, triggered by cytotoxic chemotherapeutic conditioning regimens and a prothrombotic-hypofibrinolytic state, is a critical factor in the pathophysiology of VOD/SOS. In the United States, defibrotide is approved for treating hepatic VOD/SOS with renal or pulmonary dysfunction post-HSCT, and in the European Union, defibrotide is approved to treat severe hepatic VOD/SOS post-HSCT. Prior to its approval, defibrotide had been available in the United States through an expanded-access program. Here, Day +100 post-HSCT survival and safety are analyzed for the 2 largest primary-disease subgroups in that study: acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL).
Methods
Patients in the expanded-access program had VOD/SOS diagnosed by Baltimore criteria (bilirubin ≥2 mg/dL and ≥2 of: hepatomegaly, ascites, ≥5% weight gain), modified Seattle criteria (≥2 of: total bilirubin >2 mg/dL, hepatomegaly, or ascites and/or ≥5% weight gain [in this study]), or biopsy, and this study included patients with or without MOD (defined by renal and/or pulmonary dysfunction). Defibrotide 25 mg/kg/day was given in 4 divided doses for a recommended ≥21 days.
Results
A total of 867 patients were enrolled in the safety population of the expanded-access program through April 18, 2015, including 476 patients with MOD. The primary diseases affecting 5% or more of the safety population at baseline were AML, 25.7% (222/867); ALL, 23.4% (202/867); neuroblastoma, 8.5% (73/867); and myelodysplastic syndrome, 5.7% (27/867).
Data were available for 756 post-HSCT patients who received ≥1 dose of defibrotide. Of those patients, 207 (27.4%) patients had AML and 152 (20.1%) patients had ALL as their primary disease. Of the AML patients, 49.8% (103/207) were male, and 50.2% (104/207) were female; median age at HSCT was 23 years (range: 0.5, 74.0 years); and all had allogeneic HSCT. Among the ALL patients, 62.5% (95/152) were male, and 37.5% (57/152) were female; median age at HSCT was 16 years (range: 0.3, 68.0 years); and all had allogeneic HSCT.
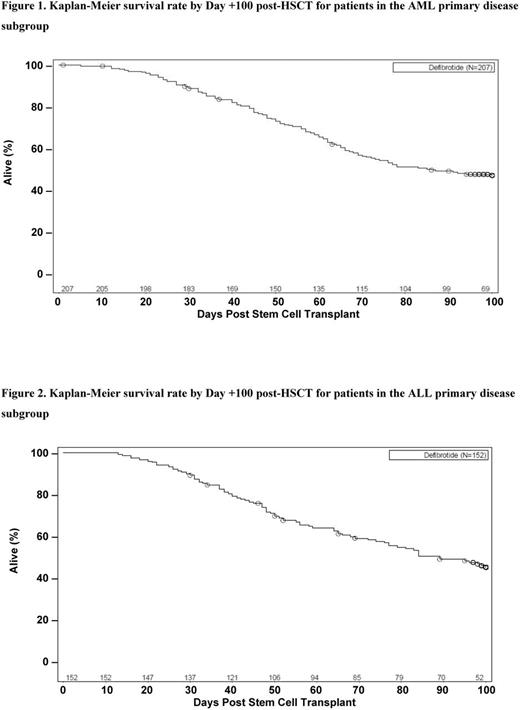
At Day +100 post-HSCT, observed survival was 45.4% (94/207) among AML patients and 42.8% (65/152) among ALL patients; 50.7% (105/207) and 52.0% (79/152), respectively, had died; and status was not available (ie, no HSCT date recorded, did not have sufficient follow-up, or their data were not available) for 3.9% (8/207) and 5.3% (8/152), respectively. For AML patients, Kaplan-Meier estimated survival rate was 47.8% (95% confidence interval [CI], 40.7%-54.5%; Figure 1); among ALL patients, Kaplan-Meier estimated survival rate was 46.0% (95% CI, 37.7%-53.9%; Figure 2).
Adverse events (AEs) occurred in 76.8% (159/207) of AML patients and 64.5% (98/152) of ALL patients, with serious AEs in 57.5% (119/207) and 52.6% (80/152), respectively. Treatment-related AEs, as assessed by investigators, occurred in 21.7% (45/207) of AML patients and 17.1% (26/152) of ALL patients (>2% in either group [all <4%]: pulmonary hemorrhage, epistaxis, gastrointestinal hemorrhage, hypotension). Treatment-related AEs leading to discontinuation developed in 14.5% (30/207) of AML patients and 8.6% (13/152) of ALL patients (>2% in either group [all <3%]: pulmonary hemorrhage, gastrointestinal hemorrhage); treatment-related deaths occurred in 3.4% (7/207) of AML patients and 2.6% (4/152) of ALL patients, respectively, with none occurring in >1 patient in either subgroup.
Conclusions
The Day +100 survival rates and safety profile for the AML and ALL subgroups in the expanded-access program were consistent with prior defibrotide studies and analyses of the overall HSCT population in this study. Kaplan-Meier estimates of survival at Day +100 were similar between the AML (47.8%) and ALL (46.0%) subgroups. Taken together, these subgroup results affirm the overall efficacy and safety profile of defibrotide in post-HSCT patients with VOD/SOS and underlying acute leukemia.
Support: Jazz Pharmaceuticals.
Richardson:Jazz Pharmaceuticals: Consultancy, Membership on an entity's Board of Directors or advisory committees. Kernan:The National Cancer Institute of the National Institutes of Health: Research Funding; Gentium: Research Funding. Grupp:Jazz Pharmaceuticals: Consultancy; Novartis: Consultancy, Research Funding; Pfizer: Consultancy. Antin:Gentium SpA/Jazz Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees. Liang:Jazz Pharmaceuticals, Inc.: Employment, Other: stock options exercisable for, and other stock awards of, ordinary shares of Jazz Pharmaceuticals plc. Hume:Jazz Pharmaceuticals, Inc.: Employment, Other: stock options exercisable for, and other stock awards of, ordinary shares of Jazz Pharmaceuticals plc. Tappe:Jazz Pharmaceuticals, Inc.: Employment, Other: stock options exercisable for, and other stock awards of, ordinary shares of Jazz Pharmaceuticals plc. Soiffer:Kiadis: Membership on an entity's Board of Directors or advisory committees; Jazz Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; Juno: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal