Abstract

Introduction: Allogeneic hematopoietic stem cell transplantation (Allo-HCT) is the only curative treatment for myelodysplastic syndrome (MDS). The portion of patients referred for transplant and the proportion who are subsequently transplanted is unknown.
Aim: Tostudy the frequency of allo-HCT in pts with MDS and identify factors associated with transplant referral and barriers to transplant.
Methods: Pts were included if they were under the age of 75 and seen at our center by a leukemia physician between 2008-2015 and within 6 months of MDS diagnosis. Pts were eligible for allo-HCT if they did not have major organ dysfunction, i.e. left ventricular ejection fraction <40%, Creatinine >2mg/dL, FEV1 <1L, DLCO <50%, metastatic solid organ malignancy within 5 years of MDS diagnosis and had KPS <60. Allo-HCT was indicated in pts with therapy related MDS (tMDS), MDS with excess blasts (RAEB-1 or 2), IPSS int-2 or High risk and in cases of life threatening cytopenia (ANC <0.5x109/L, Plt<30x109/L, Hb <7gm/dL). Pts not meeting any of these criteria at diagnosis but who developed >5% marrow blasts during follow-up were eligible for allo-HCT from date of disease progression.
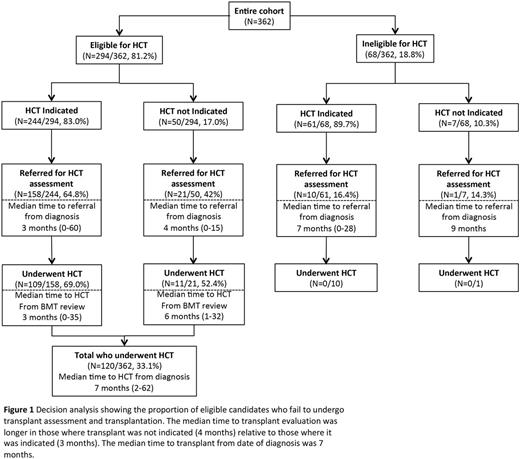
Results: This was a single center study.362 pts were identified with a median follow-up of 14 months. 294 (81.2%) were eligible for allo-HCT and in this group transplant was indicatedin 244 (83%). Of these 158 (65%) were referred for transplant evaluation and 109 (69%) of those underwent allo-HCT (figure 1).
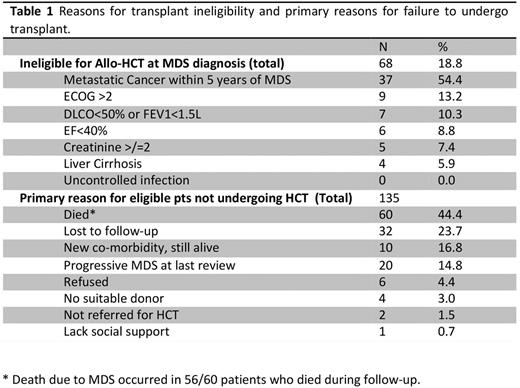
Reasons for transplant ineligibility at diagnosis and reasons for eligible patients not undergoing transplant are listed in table 1. Metastatic solid organ malignancy within 5 years of MDS diagnosis accounted for most cases of transplant ineligibility (54%), and death due to MDS and progression of disease at last follow-up (60%) were the major reasons for eligible patients not undergoing transplant. Lack of a suitable donor was rarely the primary reason for not proceeding with transplant (3%).
Factors associated with a lower likelihood of referral for transplant evaluation were primarily patient related including age over 65 (p=0.001), presence of 3 or more co-morbidities (p=0.003) and RAEB-1 or 2 (p=0.009) at diagnosis. Earlier referral was associated with high-risk disease including tMDS (p=0.006); excess blasts (p=0.001); high-risk IPSS (p=0.001) or IPSS-R (p=0.001) while patient factors including age (p=0.421), gender (p=0.258), KPS (p=0.143) and number of comorbidities (p=0.247) were not associated with time to referral. Pts diagnosis between 2014 and 2015 were referred earlier then in prior years (p<0.001).
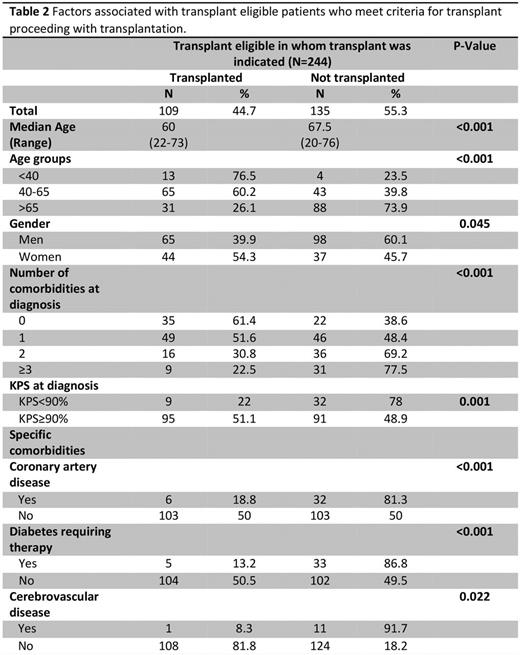
Among eligible pts in whom transplant was indicated, patient factorswere associated with a higher likelihood of undergoing transplant (table 2) including younger age, female gender, KPS over 90 and having fewer co-morbidities. Specific comorbidities associated with a reduced likelihood of undergoing transplant included coronary or cerebrovascular disease or diabetes. MDS disease features including IPSS (p=0.390), blast percentage at diagnosis (p=0.061), progression to RAEB (p=0.992) or AML (p=0.776) and earlier referral for transplant evaluation (p=0.068) were not associated with a greater likelihood of undergoing transplant. 11 pts were transplanted despite not meeting our transplant indications. These pts had a longer median time to transplant from the time of BMT assessment and underwent allo-HCT most likely due to progressive cytopenia (Figure 1)
Conclusion: Allo-HCT is underutilized in MDS patients with only 64% of eligible patients referred for evaluation and 69% of those referred undergoing transplant. Death due to MDS and disease progression were the major barriers to transplantation. The decision to refer a patient for transplant evaluation was influenced by the physician's assessment of the patient's functional eligibility (age, KPS, number of comorbidities) while the urgency of referral was influenced by disease risk. Development of reduced toxicity conditioning protocols, improved GVHD prophylaxis, extended donor options and optimization of supportive care mean older pts with higher co-morbidity scores should be referred for transplant assessment and those with low risk disease should be referred early so that donor options can be identified and a plan for transplant can be prepared prior to disease progression.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract