Abstract
Introduction: Sepsis is a severe systemic inflammatory response to infection that manifests with widespread inflammation as well as endothelial and coagulation dysfunction that may lead to hypotension, organ failure, shock, and death. Disseminated intravascular coagulation (DIC) is a complication of sepsis involving systemic activation of the fibrinolytic and coagulation pathways that can lead to multi-organ dysfunction, thrombosis, and bleeding, with a two-fold increase in mortality. Elevated levels of nucleosomes released from apoptotic cells have been detected in the blood of severe sepsis patients. Procalcitonin (PCT), a propeptide of calcitonin, is a marker of inflammation of infectious origins. Both nucleosomes and PCT are associated with the inflammatory and infectious processes that play a key role in the pathogenesis of sepsis and DIC. No single biomarker or laboratory test can effectively diagnose DIC; accordingly, the International Society on Thrombosis and Hemostasis (ISTH) has developed a diagnostic algorithm based on clinical parameters that uses platelet count, prothrombin time (PT), fibrin related marker (D-dimer) and fibrinogen levels to calculate a DIC score. This study lays the groundwork for the development of a diagnostic algorithm using several markers of inflammation and infection and DIC score as parameters in assessing severity of sepsis-associated coagulopathy (SAC) in a clinical setting.
Materials and Methods: De-identified serial plasma samples from patients diagnosed with sepsis-associated coagulopathy (n=137) were obtained from the University of Utah under an IRB approved protocol. The citrated plasma samples were collected from adult patients in the ICU upon admission and ICU days 4 and 8 In addition, plasma samples from healthy volunteers (n=50) were purchased from George King Biomedical (Overland, KS). Platelet count, prothrombin time, International normalized ratio (INR), D-dimer and fibrinogen levels were used to assign International Society of Thrombosis and Hemostasis (ISTH) DIC scores. Plasma samples were analyzed for procalcitonin (PCT) (Abcam, Cambridge, MA) and extracellular nucleosomes (Roche Diagnostics, Indianapolis, IN)) using a commercially available ELISA methods. In addition, markers of inflammation including interleukin 6 (IL-6), interleukin 8 (IL-8), interleukin 10 (IL-10) and tumor necrosis factor α (TNF α) were measure using the Biochip Array from Randox (Crumlin, County Antrim, UK).
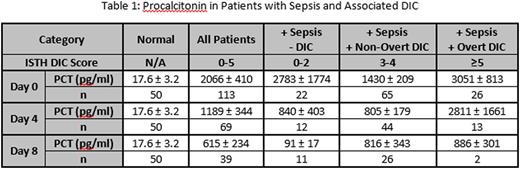
Results: DIC scores were calculated using the ISTH criteria and categorized into sepsis without DIC, non-overt DIC, and overt DIC. The levels of PCT were elevated in all three groups compared to normal (p<0.05). In addition, the patients with overt DIC had a higher level of PCT on day 0 and 4, compared to patients with non-overt DIC or sepsis alone. On day 8, the overt and non-overt DIC patients had similar levels of PCT. PCT data is shown in Table 1 (mean ± SEM). Nucleosome levels were also measured and compared between groups. Similarly, markers of inflammation, including IL-6, IL-8, IL-10 and TNF α were higher in the overt DIC group compared to the other groups on day 0 and day 4. By day 8, most of the patients initially diagnosed with overt DIC had transitioned into the non-overt group or died prior to the blood draw. The PCT levels correlated with nucleosomes, IL-6, IL-8, IL-10 and TNF α levels (p<0.05, Spearman r>0.20).
Conclusions: This study demonstrates the diagnostic and prognostic value of profiling several biomarkers of inflammation and infection in patients with sepsis-associated DIC to assess the severity of illness. Elevated levels of PCT, IL-6, IL-8, IL-10 and TNF-α were observed in most patients with sepsis and DIC. Additionally, the levels of these markers show significant positive correlations to each other and to DIC score. Currently, no single biomarker can be used to confirm the diagnosis of DIC in patients with sepsis. This study provides an initial framework in developing a multiparametric profile of biomarkers in DIC for diagnostic and prognostic purposes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.