As part of a year-long celebration in honor of Blood's 70th anniversary, we are publishing a series of editorials written by past Editors-in-Chief of the journal. The authors reflect on their experience at Blood in light of the journal's publication history. Each of these special pieces will highlight and discuss the impact of one or more original research articles that had a significant influence on the field or that mark a pioneering scientific development in hematology that appeared in the journal during the author's term as Editor-in-Chief.
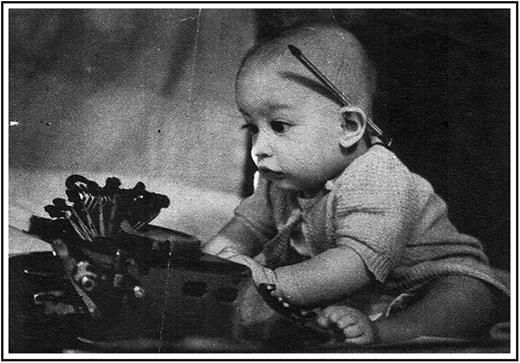
I had the great privilege and good fortune of serving as Editor-in-Chief of Blood from 2003 to 2007, a period of important advancements in the field of hematology and of new challenges and opportunities for this and other biomedical journals. I was trained to be an editor at an early age during an era of mechanical typewriters and carbon paper, and just before the birth of this journal (Figure 1). The success of Blood from 2003 to 2007 was made possible largely through the efforts of a group of talented and collegial Associate Editors, an Editorial Board committed to participating in rigorous peer review, dedicated publication professionals in Blood’s central office in Washington, DC, and an arm’s length but supportive relationship between the American Society of Hematology and the editorial apparatus of the journal. During this 5-year period, manuscript submissions to Blood increased from ∼3000 per year to >5000 per year, with the acceptance rate remaining relatively constant at ∼25%.
The early training of a Blood editor, circa 1944. This untouched photograph was taken by Arthur Shattil.
The early training of a Blood editor, circa 1944. This untouched photograph was taken by Arthur Shattil.
There were many important, even breakthrough, hematology research papers published in Blood between 2003 and 2007. I can recall several in particular that broadened my knowledge of the field and that have stood the test of time and influenced subsequent basic and clinical research and patient care. Examples from my top 10 list include (in no particular order of importance):
Demonstration of improved outcome for children with acute lymphoblastic leukemia in the Total Therapy Study XIIIB.1
Demonstration of significant clinical and cytogenetic responses to dasatinib2 or nilotinib3 in Bcr-Abl-positive chronic myelogenous leukemia, including after the development of treatment resistance to imatinib. These drugs were also shown be effective, albeit to a lesser extent, in some cases of accelerated phase4 or blast crisis5 chronic myelogenous leukemia.
Clarification of the pathobiological and clinical significance of mutations in Jak26-9 in patients with polycythemia vera, essential thrombocythemia, or myelofibrosis. Additional reports illustrated the diagnostic and clinical significance of mutations in MPL in individuals with Jak2 (V627F)–negative essential thrombocythemia,10 or in VHL in Chuvash congenital polycythemia.11,12
Identification by fluorescence in situ hybridization of deletion of the CHIC2 locus as a surrogate for the FIP1L1-PDGFRA fusion protein in systemic mastocytosis associated with eosinophilia, a predictor of response to imatinib in this disorder.13 Other individuals with systemic mastocytosis may exhibit a KIT(D816V) mutation in their bone marrow mast cells and CD34-positive hematopoietic progenitor cells,14 portending a lack of response to imatinib.
Clarification of the Blackfan-Diamond15-17 and Shwachman-Diamond18 inherited bone marrow failure syndromes as disorders of ribosome expression or function.
Continuation of efforts to reduce morbidity and mortality in individuals suffering from sickle cell anemia.19-22
Investigations into the role of hepcidin and other genes in normal iron metabolism and in disease states, including hereditary hemochromatosis and the anemia of chronic disease.23-34
Further demonstration of the therapeutic efficacy of eculizumab in paroxysmal nocturnal hemoglobinuria.35,36
Studies into the epidemiology and potential etiologies of transfusion-associated lung injury (TRALI),37 eventually leading to a change in transfusion practices that have reduced the incidence of this serious complication following blood transfusion.
Demonstration in mice that recombinant proteins such as factor VIII and urokinase-type plasminogen activator can be expressed in megakaryocytes and platelets, providing proof of principle that platelets may serve as a potential delivery system for therapeutic proteins in disorders of hemostasis or thrombosis.38,39 This work preceded by several years the generation of induced pluripotent stem cells from human somatic cells, a feat that has accelerated current efforts aimed at producing genetically modified megakaryocytes and platelets for therapeutic purposes.
What about new opportunities for Blood during my tenure as Editor-in-Chief? A series called Translational Reviews in Hematology and another called Blood Work were introduced in the journal during this period of time. The purpose of Translational Reviews was to shine light on subject areas in which basic research was informing diagnostic and therapeutic advances in nonmalignant and malignant blood disorders. The purpose of Blood Work was to bring to each issue of the journal a photomicrograph containing an interesting, pedagogical, or unusual peripheral blood smear or bone marrow. The latter series was initiated in response to concern that hematology trainees were in danger of becoming less and less exposed to the diagnostic power of the blood smear in an era of information overload and of ill-fated attempts at multitasking.40 It is gratifying to see that this series is still going strong, and it may become increasingly important as blood smear production and analysis are taken over by robots that never took a hematology fellowship. I am no Luddite, but in my view, no digital image can match the beauty and utility of a well-made peripheral blood smear examined directly under the light microscope.
Blood faced several challenges between 2003 and 2007. First, the improper use of digital images was becoming a palpable problem in scientific publishing.41 In response, we introduced a system into the editorial process to examine all such images in accepted manuscripts to educate authors on acceptable practices and to better detect inappropriate image manipulation, be it willful or unintentional.42 Guidelines for image preparation remain an important feature of Blood’s current Author Guide.
Second, in the early years of this century, publishers of biomedical journals sponsored by learned societies such as the American Society of Hematology became increasingly concerned with the growth of the open access movement, which was perceived as threatening the business models of journals like Blood. Our stance was to welcome further efforts to open access,43 but in ways that preserved the key peer-review function of the journal and its scientific rigor and financial viability. So far, so good, although models of scientific publishing continue to be a moving target.
Third, while serving as Editor-in-Chief, I frequently railed against the widespread and, to my mind, inappropriate use of journal impact factors in assessing the quality of individual published manuscripts and their authors. This remains a major problem. As recently articulated by the San Francisco Declaration on Research Assessment (http://www.ascb.org/dora/), there need to be better ways to evaluate research by academic institutions, funding agencies, and scientists themselves than journal-based impact factors. It may take a while to turn this ship around, and metrics that better assess the quality of a piece of work, its reproducibility, and its eventual impact are needed. Although I no longer speak for Blood, top journals like it should do their part and end the tyranny of the impact factor.
The Nobel laureate George Richards Minot wrote in the foreword to the first issue of Blood in 1946: “The best clinical investigator must be an able clinician, have wide interests, and understand human beings. He must possess an active, creative imagination and scientific curiosity, but the center of his activity must be the patient. Much knowledge and progressive interest has developed concerning the blood and its disorders … so that now one may feel that a medical journal in English devoted to this subject is appropriate.”44 Minot’s prescience is no better illustrated than in the current pages of Blood. It was an honor to have played a small part in the journal’s history. Happy birthday, Blood!
Acknowledgments
I thank Drs Jim Griffin and Ken Kaushansky for asking me to serve as an Associate Editor of Blood prior to my service as Editor-in-Chief. This service could not have been performed without the dedication and expertise of my Associate Editors, the editorial and production staff of the journal, and wise input from the Publications Committee of the American Society of Hematology.