Key Points
Lowest numbers of ex vivo–selected CD8+ memory T cells can reconstitute pathogen-specific immunity in immunocompromised hosts.
Abstract
Patients undergoing allogeneic hematopoietic stem cell transplantation (allo-HSCT) are threatened by potentially lethal viral manifestations like cytomegalovirus (CMV) reactivation. Because the success of today’s virostatic treatment is limited by side effects and resistance development, adoptive transfer of virus-specific memory T cells derived from the stem cell donor has been proposed as an alternative therapeutic strategy. In this context, dose minimization of adoptively transferred T cells might be warranted for the avoidance of graft-versus-host disease (GVHD), in particular in prophylactic settings after T-cell–depleting allo-HSCT protocols. To establish a lower limit for successful adoptive T-cell therapy, we conducted low-dose CD8+ T-cell transfers in the well-established murine Listeria monocytogenes (L.m.) infection model. Major histocompatibility complex-Streptamer–enriched antigen-specific CD62Lhi but not CD62Llo CD8+ memory T cells proliferated, differentiated, and protected against L.m. infections after prophylactic application. Even progenies derived from a single CD62LhiL.m.-specific CD8+ T cell could be protective against bacterial challenge. In analogy, low-dose transfers of Streptamer-enriched human CMV-specific CD8+ T cells into allo-HSCT recipients led to strong pathogen-specific T-cell expansion in a compassionate-use setting. In summary, low-dose adoptive T-cell transfer (ACT) could be a promising strategy, particularly for prophylactic treatment of infectious complications after allo-HSCT.
Introduction
After allogeneic hematopoietic stem cell transplantation (allo-HSCT), severe impairment of the patient’s T-cell compartment due to lymphocyte-depleting conditioning regimens regularly leads to reactivation of highly prevalent endogenous herpes viruses like Epstein-Barr virus, herpes simplex virus, varicella zoster virus, or cytomegalovirus (CMV). In particular, CMV can contribute substantially to direct and indirect infection-related complications in allo-HSCT patients if donor-derived virus-specific T cells cannot timely control virus replication.1,2 Prophylactic or preemptive virostatic treatment with ganciclovir or foscarnet is known to be effective but exhibits substantial side effects.3 Therefore, adoptive transfer of donor-derived virus-specific T cells has been proposed as an alternative treatment option in order to restore antiviral immunity and bridge the first months of high susceptibility after allo-HSCT.
Pilot studies in the early 1990s have convincingly illustrated the efficacy of this approach,4-7 which has further been adapted to target a wide range of infectious and noninfectious complications.8,9 Yet, the introduction of antiviral adoptive T-cell transfer into routine treatment after allo-HSCT has so far been discouraged by costly and time-consuming Good Manufacturing Practices–conform in vitro expansions.10
More recently, direct ex vivo isolation (<24h) of virus-specific T cells using conventional11 or minimally manipulating reversible major histocompatibility complex (MHC) multimers12,13 as well as short-time–stimulated cytokine-secreting T cells14-16 has been successfully tested in clinical pilot studies.
However, yield of these primary virus-specific T cells can be limited by cell isolation efficiency from small antigen-specific donor T-cell populations. In addition, the content of contaminating, potentially graft-versus-host disease (GVHD)-triggering CD3+ T cells restricts the total number of adoptively transferred T cells.17 In particular, for the envisioned prophylactic strategies or the recently proposed use of partially HLA-matched third-party donors,18-20 the use of small-sized clinical T-cell products might become indispensable to keep the risk of GVHD as low as possible.
Because the minimal number of ex vivo–isolated cells for successful T-cell therapy is unknown, we decided to test the potential of minimal numbers of ex vivo–isolated antigen-specific T cells in a well-established murine infection model with the intracellular bacterium Listeria monocytogenes (L.m.). After systemic application in mice, L.m. uses cellular niches to survive initially in the spleen.21,22 Although infection is primarily confined by innate defense mechanisms, clearance of L.m. depends on the mobilization of adaptive immunity, illustrated by chronic L.m. infection in severe combined immunodeficiency (SCID) mice.23 The established (eventually) lifelong T-cell immunity is mainly mediated by antigen-experienced CD8+ memory T cells, and contribution of different memory subsets to protective T-cell responses has been controversially discussed during the last decade. However, in the context of adoptive T-cell transfer, data are accumulating that less differentiated memory subsets (eg, CD62Lhi cells) might comprehend all necessary qualities for in vivo efficacy, in particular if implemented for prophylactic use: long-term survival, extensive proliferative capacity, and differentiation potential into effector and effector memory cells that finally convey cytotoxic control.24-27
In addition, we could recently show that single naive L.m.-epitope–specific CD8+ T cells can differentiate into diverse effector and memory T-cell subsets.28,29 Here, we used a comparable single-cell transfer protocol to evaluate the protective capacity of minimal numbers of naive L.m.-epitope–specific CD8+ T cells after in vivo challenge and in addition extended these analyses to CD62Lhi and CD62Llo CD8+ memory T cells. The lowest numbers of CD62Lhi memory T cells developed into diversified progenies conferring protection against L.m. challenge, identifying this subpopulation as the most potent for effective adoptive immunotherapy. Finally, the reconstitution capacity of human low-dose T-cell transfers was demonstrated by the expansion of Streptamer-enriched CMV-specific CD8+ T cells in 2 compassionate-use allo-HSCT patients.
Methods
Mice and L.m. infection
CD45.2+ C57BL/6 wild-type (B6 wt) mice were obtained from H. Winkelmann (Borchen, Germany). CD45.1+ congenic C57BL/6 (CD45.1), CD45.2+ RAG1-deficient (RAG−/−) mice and CD45.1+ Kb-ovalbumin (Ova257–264) peptide–specific T-cell receptor (TCR) C57BL/6 transgenic mice (CD45.1-OT-I) were derived from in-house breeding. Experimental conditions of adoptive transfer and L.m. infection experiments are provided in the supplemental Methods (available at the Blood Web site)
Isolation of ova-specific donor T cells
Naive CD45.1-OT-I T cells, antigen-experienced CD45.1+ OT-I memory T cells, or polyclonal Ova257-264-peptide–specific CD45.1+ memory T cells were used for adoptive cell transfer. See supplemental Methods for details.
Cell sorting and adoptive transfer of T cells
The adoptive cell transfer of 1 to 1000 antigen-specific CD8+ T cells has been previously described29 and is described in detail in the supplemental Methods.
MVA-Ova immunization and L.m.-Ova challenge in recipient mice
Recipient mice were prime-boost immunized by IV injection with 2 subsequent doses (1 × 108 colony-forming units [CFUs]) of a replication-deficient modified vaccinia virus type Ankara recombinantly expressing ova under control of the viral P7.5 promoter (MVA-Ova).30 Expansion and differentiation of T-cell progenies were followed by fluorescence-activated cell sorter (FACS) staining of blood and ex vivo tissue samples as previously described,31 and protective capacity of donor-derived T-cell responses was tested in adoptively transferred T-cell–deficient RAG−/− recipient mice by L.m.-Ova infection. See supplemental Methods for further details.
Patients
Two patients were treated with allo-HSCT for SCID syndrome and B-cell acute lymphoblastic leukemia (B-ALL), respectively. Patients suffered before and/or after stem cell transplantation from a therapy-resistant CMV viremia.
Isolation of human CMV-specific donor lymphocytes
Tracking of donor-derived CMV HLA-A0201/pp65–specific CD8+ T cells
CDR3 sequencing of ex vivo–isolated transferred T cells allowed identification of donor-derived T cells as previously described.13 See supplemental Methods for details.
Approval for the transplantation and the compassionate use treatment was obtained from the Medical Ethical Board of the University Medical Center Utrecht and the Medical Faculty Ethics Committee of Heinrich-Heine University Düsseldorf, respectively. Informed consent was provided according to the Declaration of Helsinki.
Results
Low-dose transfer of naive ova-peptide–specific T cells confers protection against L.m.-Ova challenge
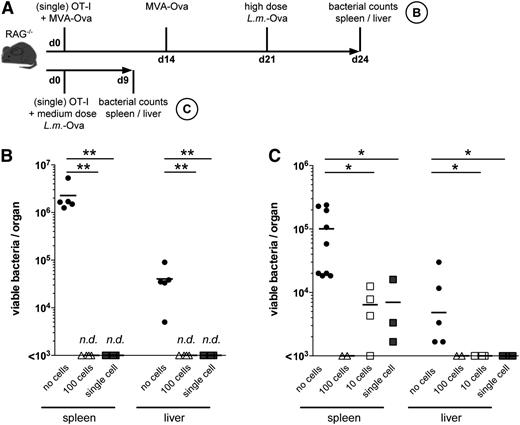
In murine L.m.-Ova infection, single adoptively transferred ovalbumin-peptide–specific CD8+ T cells can give rise to highly diversified T-cell populations. Those progenies can consist of both effector and memory T cells and resemble herein concomitantly developing endogenous T-cell responses in B6 wt hosts.28,29 However, whether developing T cells from such lowest-cell-dose transfers will also be sufficient to protect against full-scale infection has not yet been determined. To address this question in regard to its clinical relevance, we used T- and B-cell–devoid RAG−/− recipient mice,32 in which any functional antibacterial T-cell response could be unambiguously attributed to the progeny of adoptively transferred T cells. L.m.-infected T- and B-cell–deficient mice are not able to eradicate the pathogen, and chronic infection develops.23 In order to study the expansion potential as well as the protective capacity of low-dose adoptive T-cell transfers in immunocompromised hosts, we used MVA-Ova for prime-boost vaccination prior to challenge with L.m.-Ova. RAG−/− mice received a first MVA-Ova dose briefly after adoptive T-cell transfer followed by a boost vaccination 14 days later (Figure 1A). Expansion of transferred CD45.1+ CD8+ T cells was subsequently followed in peripheral blood. In accordance with our previously published data,28,29 transfer of 100 CD45.1+ OT-1 T cells was found to be successful in all recipient mice, and single-cell transfers still resulted in detectable antigen-specific T-cell populations in peripheral blood of 15% to 20% of recipients (data not shown).28,29 After challenge with an otherwise-lethal dose of L.m.-Ova, all successfully single-cell–transferred mice had no detectable bacteria in liver and spleen, whereas bacterial loads were at least 100- to 1000-fold higher in recipients with no detectable T cells after single-cell transfer and vaccination (Figure 1B). Taken together, these data show that even the lowest amounts of adoptively transferred naive antigen-specific CD8+ T cells (and, in the extreme, even a single cell) can establish a functional T-cell response in RAG−/− hosts leading to complete protection against high-dose bacterial challenge.
Adoptive transfer of a single naive antigen-specific CD8+ T cell can reconstitute protective immunity toward high-dose L.m. infection. (A) Schematic outline of the experimental procedure. RAG−/− recipient mice received a single naive (CD44lo) CD45.1-OT-I CD8+ T cell by intraperitoneal application. On days 0 and 14 after T-cell transfer, prime/boost IV vaccination was performed with 1 × 108 MVA-Ova. On day 21 after T-cell transfer, mice were challenged IV with an otherwise-lethal dose of L.m.-Ova. Three days later, viable bacteria in tissue homogenates were determined by counting CFUs on brain heart infusion plates. Results are depicted in panel B. Alternatively, RAG−/− recipient mice received naive CD45.1 OT-I TCR-transgenic CD8+ T cells as before, and on the same day recipient mice were challenged IV with L.m.-Ova (infection dose 7500 bacteria). (C) Nine days later, viable bacteria were determined in spleen and liver. Mice receiving 100 CD45.1 OT-I cells served as positive control, whereas mice with undetectable CD45.1 OT-I T cells after single-cell transfer (no cells) served as a negative control (n.d., not detectable). Horizontal bars indicate means. P values were calculated by 1-way analysis of variance.
Adoptive transfer of a single naive antigen-specific CD8+ T cell can reconstitute protective immunity toward high-dose L.m. infection. (A) Schematic outline of the experimental procedure. RAG−/− recipient mice received a single naive (CD44lo) CD45.1-OT-I CD8+ T cell by intraperitoneal application. On days 0 and 14 after T-cell transfer, prime/boost IV vaccination was performed with 1 × 108 MVA-Ova. On day 21 after T-cell transfer, mice were challenged IV with an otherwise-lethal dose of L.m.-Ova. Three days later, viable bacteria in tissue homogenates were determined by counting CFUs on brain heart infusion plates. Results are depicted in panel B. Alternatively, RAG−/− recipient mice received naive CD45.1 OT-I TCR-transgenic CD8+ T cells as before, and on the same day recipient mice were challenged IV with L.m.-Ova (infection dose 7500 bacteria). (C) Nine days later, viable bacteria were determined in spleen and liver. Mice receiving 100 CD45.1 OT-I cells served as positive control, whereas mice with undetectable CD45.1 OT-I T cells after single-cell transfer (no cells) served as a negative control (n.d., not detectable). Horizontal bars indicate means. P values were calculated by 1-way analysis of variance.
Next, we tested if the lowest numbers of transferred naive antigen-specific CD8+ T cells can directly contain bacterial growth in a preemptive setting33 in RAG−/− mice without previous MVA-Ova vaccination. Mice were infected with a sublethal dose of L.m.-Ova immediately after transfer of naive CD45.1+ OT-I cells, and bacterial replication was determined by CFU counts in the spleen 9 days later (Figure 1A). As previously described for L.m.-infected SCID mice,23,34 high bacterial numbers (mean 105 CFUs; Figure 1C) were counted in spleens of RAG−/− mice in the absence of adoptively transferred L.m.-specific CD45.1+ T cells. In contrast, viable bacteria were undetectable (<103 CFUs) after transfer of 100 naive CD45.1 OT-I cells, and successful 10-cell and single-cell transfers led to a significant reduction of bacterial load in comparison with mice that had no detectable CD45.1+ progeny. This demonstrates that the lowest numbers of antigen-specific T cells can restrict bacterial growth even in the absence of previous T-cell priming or endogenous T-cell help.
The complete absence of endogenous adaptive immunity in RAG−/− mice could facilitate survival and proliferation after low-dose T-cell transfer due to increased availability of survival factors like interleukin-7 or interleukin-15.35,36 Although clinical adoptive T-cell transfer is often performed under such lymphopenic conditions, we wanted to estimate the influence of homeostatic proliferation in our experimental setting. Therefore, we compared low-dose transfer efficacy rates in RAG−/− and B6 wt mice using the MVA-Ova prime/boost scheme described above (Figure 1A). Ten-cell transfers into B6 wt mice resulted in detectable CD45.1+ T-cell expansions in 85% of all transfers (supplemental Figure 1A) and thus showed identical efficacy rates (6/7 mice) as transfers into RAG−/− hosts (supplemental Figure 1B). Although the mean absolute numbers of CD45.1+ T cells in spleens of B6 wt recipients seemed slightly lower (supplemental Figure 1C) than those in RAG−/− mice, this trend was not statistically significant (P = .180). Altogether, antigen-specific naive T cells, transferred in the lowest cell doses, survive and proliferate also in the presence of a physiological T-cell compartment in wt mice.
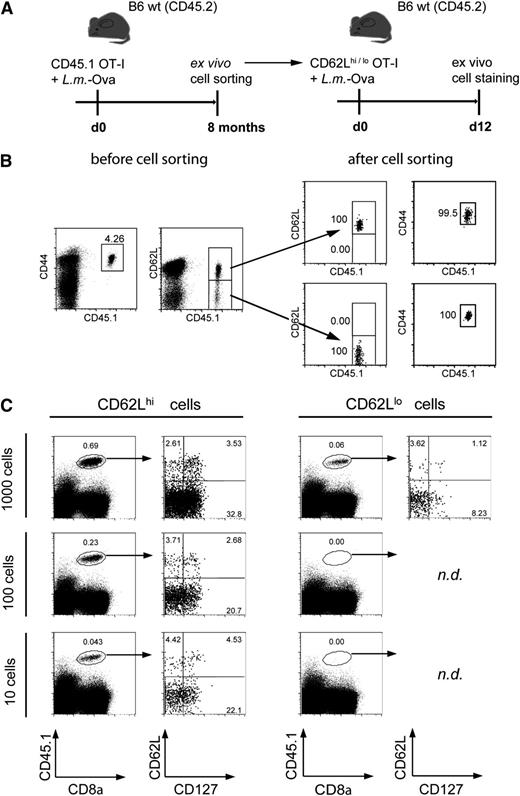
Antigen-triggered proliferation and differentiation of CD62Lhi CD8+ memory T cells after low-dose transfer
Naive antigen-specific precursor T cells are often very low in frequency and too difficult to detect or enrich from human blood by today’s methods. Therefore, the main focus for clinical adoptive transfers (at least if nonmanipulated primary T cells are used) is currently put on circulating antigen-experienced T cells. Because both CD62Lhi and CD62Llo memory T cells have been described to contribute to protection against reinfections with L.m. in mice,29,37 we examined their survival and differentiation potential after low-dose T-cell transfer (Figure 2). CD45.1+ OT-I memory cells were isolated from L.m.-Ova immune donor mice (CD45.2+) by highly pure FACS sorting of either CD62Lhi or CD62Llo antigen-experienced CD44hi memory T cells (Figure 2A-B). CD62Lhi memory T cells showed high survival rates after adoptive transfer, manifesting in successful 10-cell transfers, whereas descendants from CD62Llo memory T cells could only be detected when recipients had received higher T-cell doses. In addition, expanded populations derived from CD62Llo CD45.1 OT-I T cells exhibited lower levels of differentiation into long-lasting CD127+ memory T cells (Figure 2C). Furthermore, descendants of CD62Lhi memory T cells were detectable for more than 8 weeks after transfer, indicating long-term persistence (data not shown). In consequence, CD62Lhi memory T cells seem to be the better-suited candidates for prophylactic low-dose transfers.
Expansion of CD62Lhi antigen-experienced memory T cells after low-dose T-cell transfer. (A) B6 wt (CD45.2) recipient mice received 10 naive CD44lo CD45.1+ OT-I T cells and were subsequently infected with 5 × 103L.m.-Ova. Eight months later, CD45.1+ OT-I T cells were identified from living lymphocytes as CD44hi CD62Lhi and CD62Llo memory T-cell subsets (B, before cell sorting). Subset cells were FACS purified (B, after cell sorting) and transferred into L.m.-Ova-infected (5 × 103) B6 wt (CD45.2) recipient mice, respectively. (C) Expansion and differentiation of the transferred memory T-cell subsets were analyzed 12 days later. The frequencies of re-expanded CD45.1 OT-I memory subset T cells in the spleen after transfer of the indicated cell numbers are demonstrated, and representative differentiation patterns of expanded CD45.1+ T cells (CD127 and CD62L staining) are shown (n.d., not detectable).
Expansion of CD62Lhi antigen-experienced memory T cells after low-dose T-cell transfer. (A) B6 wt (CD45.2) recipient mice received 10 naive CD44lo CD45.1+ OT-I T cells and were subsequently infected with 5 × 103L.m.-Ova. Eight months later, CD45.1+ OT-I T cells were identified from living lymphocytes as CD44hi CD62Lhi and CD62Llo memory T-cell subsets (B, before cell sorting). Subset cells were FACS purified (B, after cell sorting) and transferred into L.m.-Ova-infected (5 × 103) B6 wt (CD45.2) recipient mice, respectively. (C) Expansion and differentiation of the transferred memory T-cell subsets were analyzed 12 days later. The frequencies of re-expanded CD45.1 OT-I memory subset T cells in the spleen after transfer of the indicated cell numbers are demonstrated, and representative differentiation patterns of expanded CD45.1+ T cells (CD127 and CD62L staining) are shown (n.d., not detectable).
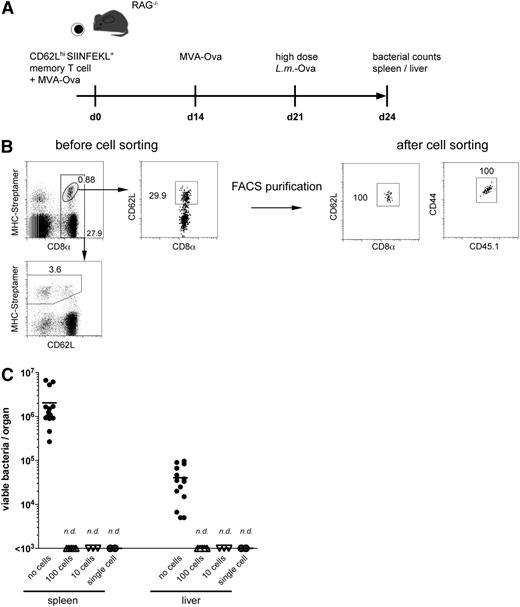
Single-cell transfer from polyclonal CD62Lhi CD8+ memory T cells can establish a protective T-cell compartment against high-dose L.m.-Ova infection
In order to mimic most realistically a potential source of CD62Lhi CD8+ memory T cells for future adoptive T-cell transfers in humans, we isolated polyclonal H2-Kb-SIINFEKL-specific CD62Lhi CD8+ memory T cells using MHC-Streptamers from resting L.m.-Ova–immune CD45.1 mice and tested their protective capacity after adoptive transfer into RAG−/− recipients (Figure 3A). FACS sorting of CD62Lhi H2-Kb-SIINFEKL+ CD45.1+ splenocytes led to the highest purity of enriched cells (Figure 3B; 100% CD62Lhi/CD8+/CD44hi cells gated on living lymphocytes). In order to prevent T-cell activation mediated by MHC-multimer binding to the cognate TCR, the remaining Streptamers were completely removed directly after FACS purification (data not shown).12
Successful single-cell transfer of CD62Lhi antigen-experienced CD8+ memory T cells. (A) Adoptive transfer protocol from H2-Kb/SIINFEKL-Streptamer–enriched polyclonal (not TCR transgenic) memory T cells. (B) MHC-Streptamer–positive CD62Lhi CD8+ memory T cells were identified in spleens of L.m.-Ova-immune CD45.1 wt mice (B, before cell sorting) and FACS purified (purities in B, after cell sorting). Streptamer reagents were removed after addition of d-biotin, and cells were immediately transferred into RAG−/− mice. Recipient mice were MVA vaccinated and L.m.-Ova challenged in analogy to Figure 1. (C) Bacterial counts in spleen and liver of mice with the indicated transferred T-cell numbers are shown (n.d., not detectable). Negative control mice had undetectable CD45.1-OT-I T cells after single-cell transfer (no cells).
Successful single-cell transfer of CD62Lhi antigen-experienced CD8+ memory T cells. (A) Adoptive transfer protocol from H2-Kb/SIINFEKL-Streptamer–enriched polyclonal (not TCR transgenic) memory T cells. (B) MHC-Streptamer–positive CD62Lhi CD8+ memory T cells were identified in spleens of L.m.-Ova-immune CD45.1 wt mice (B, before cell sorting) and FACS purified (purities in B, after cell sorting). Streptamer reagents were removed after addition of d-biotin, and cells were immediately transferred into RAG−/− mice. Recipient mice were MVA vaccinated and L.m.-Ova challenged in analogy to Figure 1. (C) Bacterial counts in spleen and liver of mice with the indicated transferred T-cell numbers are shown (n.d., not detectable). Negative control mice had undetectable CD45.1-OT-I T cells after single-cell transfer (no cells).
Similar to naive OT-I T cells, even single memory T cells derived from polyclonal Ova257-264-peptide–specific CD62Lhi CD8+ T-cell populations were able to expand vigorously after in vivo MVA-Ova restimulation and were readily detectable in peripheral blood 3 weeks after transfer (data not shown). Accordingly, a high-dose (2 × 105) L.m.-Ova challenge was completely controlled in successfully transferred RAG−/− mice manifesting in undetectable bacterial growth 3 days after infection. In spleen, this corresponded to an at least 1000-fold reduction of bacterial burden in comparison with unprotected RAG−/− control mice (Figure 3C).
Taken together, the smallest amounts of naive as well as antigen-experienced CD62Lhi memory CD8+ T cells can successfully expand and differentiate after adoptive T-cell transfer and confer protection against otherwise-lethal L.m. infections in mice.
Vigorous proliferation of primary human CMV-specific CD8+ T cells after low-dose adoptive T-cell transfer into HSCT patients
Experience from compassionate-use treatments indicates that HLA-Streptamer–enriched CMV-specific T cells can be detected after transfer into hematopoietic stem cell transplantation (HSCT) recipients, expand, and correlate with control of therapy-refractory CMV reactivation. Here, 2 children with CMV reactivations after HSCT were treated in a compassionate-use setting according to a recently established protocol.13 Both patients received very low amounts of virus-specific T cells in contrast to previous treatments, allowing the first insights into the course of low-dose T-cell transfers in human immunocompromised patients.
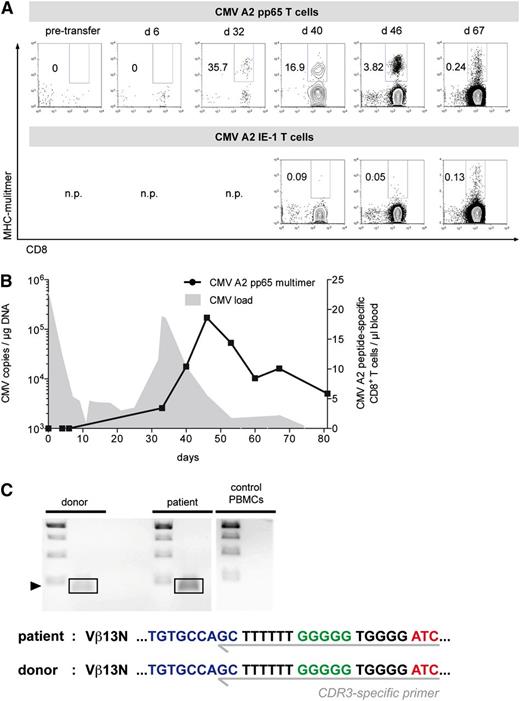
Patient 1 was an 11-month-old boy with SCID syndrome. Born and raised in the middle-eastern region, the severely immunocompromised child suffered from bacille Calmette-Guerin vaccine-induced generalized atypical mycobacteriosis and uncontrolled systemic CMV infection with ocular (retinitis) and cerebral (calcifications) manifestations. A potentially curative haploidentical HSCT with CD34-positive selected stem cells from the father was conducted under CD3-depleting antibody (OKT3) coverage. Because conventional antiviral drug therapy with ganciclovir and foscarnet did not lead to the control of tremendously high (>108 copies per µg DNA) CMV viremia, it was decided to treat the patient by adoptive T-cell transfer from the CMV-seropositive father. Fifteen days after allo-HSCT, CMV-specific A2-pp65–restricted CD8+ T cells were enriched with HLA-Streptamers, and within the same day, the patient received as few as 30 000 antigen-specific T cells (3750 cells per kg body weight) IV. On day 32 after adoptive T-cell transfer, CMV A2-pp65–restricted CD8+ T cells became detectable and expanded intensively during the following weeks (Figure 4A). Initial control of CMV blood virus load immediately after transfer was only transient and occurred well before detection of CMV-specific T cells (Figure 4B). Although not examined, this could have been potentially mediated by innate immune cells (eg, natural killer cells38,39 ). However, temporally rising virus levels decreased drastically for a second time, this time in close correlation with the expanding CMV A2-pp65–specific T-cell population. During the following weeks, CMV copy levels remained low (Figure 4B). Concomitant side effects (GVHD induction) of the expanding T cells were not observed. CMV A2-pp65-multimer–positive cells stabilized after a peak concentration of nearly 20 cells per µL on a level of around 10 cells per µL, which has been previously described as being predictive for antiviral protection.40 Phenotypic characterization of the expanding CMV A2-pp65-multimer–positive cells showed development from a less differentiated phenotype on day 32 containing CCR7+CD45RA− central memory phenotype cells (14.5%) to a mature population with a high percentage of so-called Temra cells (CCR7−CD45RA+; supplemental Figure 3C). The establishment of other endogenous CMV-specific T cells did not seem to be hindered by the CMV A2-pp65–specific CD8+ T cells, as CMV A2 IE-1-restricted CD8+ T cells became clearly detectable on day 67 (35 days after the first appearance of the presumably transfer-derived CMV A2-pp65–specific CD8+ T cells).
Expansion of CMV-specific CD8+ T cells after low-dose T-cell transfer in a SCID patient. A 10-month-old boy with SCID syndrome and generalized CMV disease (patient 1) had been reconstituted with PBSCs from the father. Fourteen days after allo-HSCT, 30 000 donor-derived CMV HLA-A0201/pp65-peptide–specific CD8+ T cells (3750 per kg body weight) were infused. Patient-derived PBMCs were analyzed at different time points before and after adoptive transfer. (A) Visualization of CMV HLA-A0201/pp65-peptide–specific T cells using MHC multimers. The frequencies among CD3+ T cells are indicated. Additionally, the kinetics of endogenously selected CMV HLA-A0201/IE-1-peptide–specific CD8+ T cells of respective time points are illustrated (n.p., not performed). (B) Comparison of CMV-specific T-cell kinetics and CMV detection. The absolute numbers of CMV HLA-A0201/pp65-peptide–specific T cells (circles) are indicated. CMV load was measured in the peripheral blood via quantitative PCR (filled gray). (C) Tracking of donor-derived CMV HLA-A0201/pp65–specific CD8+ T cells. Amplified donor and patient PCR products of an identified CDR3 region are shown (left). In control PBMCs, no product amplification was detectable. Detected PCR products (∼193 bp) were subsequently sequenced. The isolated sequences of the CDR3 region from patient and donor are shown in detail (right; blue: V segment; green: D segment; red: J segment).
Expansion of CMV-specific CD8+ T cells after low-dose T-cell transfer in a SCID patient. A 10-month-old boy with SCID syndrome and generalized CMV disease (patient 1) had been reconstituted with PBSCs from the father. Fourteen days after allo-HSCT, 30 000 donor-derived CMV HLA-A0201/pp65-peptide–specific CD8+ T cells (3750 per kg body weight) were infused. Patient-derived PBMCs were analyzed at different time points before and after adoptive transfer. (A) Visualization of CMV HLA-A0201/pp65-peptide–specific T cells using MHC multimers. The frequencies among CD3+ T cells are indicated. Additionally, the kinetics of endogenously selected CMV HLA-A0201/IE-1-peptide–specific CD8+ T cells of respective time points are illustrated (n.p., not performed). (B) Comparison of CMV-specific T-cell kinetics and CMV detection. The absolute numbers of CMV HLA-A0201/pp65-peptide–specific T cells (circles) are indicated. CMV load was measured in the peripheral blood via quantitative PCR (filled gray). (C) Tracking of donor-derived CMV HLA-A0201/pp65–specific CD8+ T cells. Amplified donor and patient PCR products of an identified CDR3 region are shown (left). In control PBMCs, no product amplification was detectable. Detected PCR products (∼193 bp) were subsequently sequenced. The isolated sequences of the CDR3 region from patient and donor are shown in detail (right; blue: V segment; green: D segment; red: J segment).
In order to provide further evidence for the adoptive T-cell transfer as the origin of the detected CMV A2-pp65 CD8 T-cell population, we extracted messenger RNA from FACS-purified CMV A2-pp65-multime–-positive donor T cells and identified in this material a specific TCR Vβ13-CDR3 region sequence. Design of a 3′ CDR3 region-specific primer then allowed screening in patient- and donor-derived PBMCs for the identified region and revealed the presence of the donor-specific CDR3 sequence in a posttransfer patient sample (Figure 4C). Resequencing of the products confirmed identity of the products from donor and recipient on the nucleotide level.
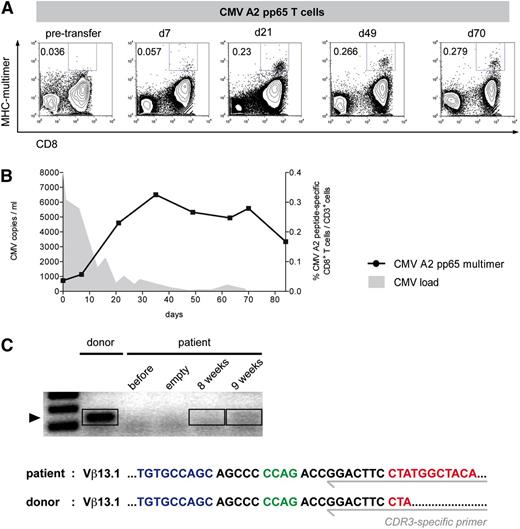
Patient 2 was a 14-year-old boy who had initially received cord blood transplantation in second remission after relapsed precursor B-ALL. Because engraftment eventually failed, a second transplantation with haploidentical PBMCs from the father became necessary but was complicated by therapy-refractory CMV reactivation and slow T-cell recovery. In consequence, the patient was treated 5 months after haploidentical HSCT with CMV-specific T cells from the CMV-seropositive father. The boy received only a total of 200,000 A2-pp65–restricted Streptamer-enriched CD8+ T cells (5130 cells per kg body weight), and again, we could observe expansion of CMV A2-pp65-multimer–positive cells after adoptive T-cell transfer (Figure 5A). Whereas antigen-specific T-cells proliferated, CMV virus load decreased to very low levels (Figure 5B).
Proliferation of CMV-specific CD8+ T cells in a patient with haploidentical HSCT after B-ALL. A 14-year-old boy with B-ALL (patient 2) and therapy-refractory CMV reactivation after haploidentical allo-HSCT was treated with Streptamer-purified CMV-specific CD8+ T cells. He received 5130 cells per kg (in total 200 000 cells) stem cell donor–derived CMV HLA-A0201/pp65-peptide–specific T cells 5 months after allo-HSCT. Patient-derived PBMCs were analyzed at different time points before and after adoptive transfer. (A) CMV HLA-A0201/pp65-peptide–specific T cells were visualized with MHC multimers, and selected time points are demonstrated. The frequencies among CD3+ T cells are indicated. (B) Comparison of CMV-specific T-cell kinetics and CMV detection. The frequency of CMV HLA-A0201/pp65-peptide–specific cells among CD3+ T cells is indicated (circles). CMV load was measured in the peripheral blood via quantitative PCR (filled gray). (C) Tracking of donor-derived CMV HLA-A0201/pp65–specific CD8+ T cells via CDR3 sequencing. Amplified donor and patient PCR products (8 and 9 weeks) of an identified CDR3 region are shown (top). Detected PCR products were subsequently sequenced. The isolated sequences of the CDR3 region from patient and donor are shown in detail (bottom; blue: V segment; green: D segment; red: J segment).
Proliferation of CMV-specific CD8+ T cells in a patient with haploidentical HSCT after B-ALL. A 14-year-old boy with B-ALL (patient 2) and therapy-refractory CMV reactivation after haploidentical allo-HSCT was treated with Streptamer-purified CMV-specific CD8+ T cells. He received 5130 cells per kg (in total 200 000 cells) stem cell donor–derived CMV HLA-A0201/pp65-peptide–specific T cells 5 months after allo-HSCT. Patient-derived PBMCs were analyzed at different time points before and after adoptive transfer. (A) CMV HLA-A0201/pp65-peptide–specific T cells were visualized with MHC multimers, and selected time points are demonstrated. The frequencies among CD3+ T cells are indicated. (B) Comparison of CMV-specific T-cell kinetics and CMV detection. The frequency of CMV HLA-A0201/pp65-peptide–specific cells among CD3+ T cells is indicated (circles). CMV load was measured in the peripheral blood via quantitative PCR (filled gray). (C) Tracking of donor-derived CMV HLA-A0201/pp65–specific CD8+ T cells via CDR3 sequencing. Amplified donor and patient PCR products (8 and 9 weeks) of an identified CDR3 region are shown (top). Detected PCR products were subsequently sequenced. The isolated sequences of the CDR3 region from patient and donor are shown in detail (bottom; blue: V segment; green: D segment; red: J segment).
Again, we could detect a donor-specific Vβ13-CDR3 polymerase chain reaction (PCR) product in FACS-sorted CMV A2-pp65–specific CD8 recipient T cells with a very faint band occurring after 8 weeks of transfer that became clearly detectable 1 week later (9 weeks posttransfer). From this PCR product, donor and recipient identity was again confirmed by sequencing.
Taken together, these 2 clinical cases demonstrate that very small numbers of adoptively transferred CMV-specific Streptamer-enriched CD8+ T cells can cause vigorous expansion and the differentiation of virus-specific T cells in immunocompromised HSCT patients.
Discussion
Although HSCT has been successfully developed through the last decades and became the standard treatment of various hematopoietic malignancies and primary immune deficiencies, it yet bears a high rate of severe, sometimes lethal complications. Most importantly, substantial risk for acute and chronic GVHD often remains the price to pay with standard transplantation protocols. Principally, depletion of T cells in hematopoietic stem cell transplants can drastically reduce the GVHD risk,41 but beneficial effects of such protocols were unfortunately found to be counteracted by delayed hematopoietic reconstitution with increased risk for relapse or opportunistic infections.42 Still, the recent shift in the indication for HSCT toward acute leukemia and/or older age with higher risk for GVHD has renewed the interest in GVHD-minimizing T-cell depletion (TCD) protocols.43 Indeed, the latest retrospective comparisons of optimized state-of-the-art TCD protocols against conventional GVHD prophylaxis using pharmacologic immunosuppressives suggest that GVHD rates can be significantly reduced without affecting survival rates of related and unrelated donor HSCT.44,45 It is tempting to speculate whether successful prevention of viral (and potentially other opportunistic) infections by adoptive T-cell transfer could help to shift the balance in favor of optimized TCD strategies, avoiding the often-limiting side effects (especially in older patients) of antiviral and also immunosuppressive agents (omissible due to the minimized GVHD risk) after transplantation. However, even though omission of pharmacologic immunosuppression in T-cell–depleted HSCT patients should augment the efficacy of transferred antiviral T cells, this clinical situation could, on the other hand, also increase the risk of GVHD induction by contaminating unrestricted CD3+ cells. Because those cells, even under the most stringent purification procedures for virus-specific T cells, cannot be completely eliminated, the applicable numbers of transferred T cells would probably be considerably restricted, particularly if antiviral T cells were applied in a prophylactic manner or isolated from partially HLA-mismatched “third-party” donors.18-20,46
In this context, our findings that the lowest doses of pathogen-specific T cells can build up fully differentiated T-cell populations in mice as well as in human HSCT patients indicate that such low-dose transfers could indeed become a successful strategy.
The murine L.m. infection model used here mimics the targeted clinical situation in various ways. First, the complete absence of endogenous T cells in RAG−/− mice revealed the actual potential of low-dose T-cell transfers in T-cell–deficient lymphopenic hosts. With proper (re-)stimulation either by the replication-deficient MVA or even direct L.m. challenge, very low numbers of transferred L.m.-specific CD8+ T cells proliferated vigorously and differentiated functionally, leaving protective immunity against L.m. challenge. Still, homeostatic proliferation, which has been well described in lymphopenic hosts,47 could have promoted T-cell survival and expansion after low-dose transfer into RAG−/− mice. However, the immediate antigen-specific stimulation after T-cell transfer makes a main influence of homeostatic proliferation on the extent of subsequent memory T-cell generation unlikely, at least in our experimental setting. Accordingly, the efficacy rates of successful transfers into “full” B6 wt mice were equal to “empty” RAG−/− hosts, although minor influences of the host environment (insignificantly higher amounts of expanded T cells in RAG−/− mice; supplemental Figure 1C) could not be excluded. Even if homeostatic effects favored T-cell expansion in T-cell-deficient hosts, this may well reflect the situation in T-cell–depleted HSCT patients. Interestingly, endogenous CD4+ T cells were not required for the development of protective CD8+ T-cell memory in RAG−/− mice, even though influences on long-term survival of the transferred T cells were not in the focus of our study and remain to be determined. Furthermore, a compensatory contribution of inflammatory stimuli during MVA-Ova stimulation or L.m.-Ova infection in the absence of CD4+ T-cell help cannot be excluded. In any case, in particular interleukin-2–producing pathogen-specific memory T cells, which have been originally properly primed in healthy donors, should be well equipped to survive and expand after clinical transfers into immunocompromised hosts.28,48
Importantly, T cells derived from murine polyclonal antigen-specific memory T-cell populations were as protective as naive TCR-transgenic CD8+ T cells, and even single memory cells could develop into fully protective diverse T-cell progenies. This demonstrates that our observations are not limited to TCR-transgenic T cells or a particular TCR. This is crucial for adoptive immunotherapies, because it implicates that human antigen-experienced antiviral T cells, which can control, for example, CMV or Epstein-Barr virus infections in healthy seropositive individuals and which can be reliably selected from blood donors, may also similarly harbor the tremendous expansion potential of their murine T-cell memory counterparts. The low-dose transfers of HLA-Streptamer–enriched CMV-specific CD8+ T cells into 2 patients, which we report here (Figures 4 and 5), indeed support this assumption.
Because the functional reconstitution of a pathogen-specific T-cell compartment will be essential for the protectivity of low-dose transfers in clinical settings, we would suggest to apply those cells as early as possible after HSCT. In prophylactic settings, polyspecific central memory T cells (TCM) could survive until pathogens start to replicate (supplemental Figure 2), functionally differentiate after antigenic stimulation, and prevent clinical manifestation. Alternatively, very early preemptive usage of low-dose transfers could be envisioned in settings where pathogen replication could be temporally contained by anti-infective medication (eg, CMV reactivation).
We also compared the transfer potential of different T memory subtypes. Intriguingly, L.m.-specific CD62Lhi memory T cells showed a clearly advantageous proliferation and differentiation profile in comparison with CD62Llo memory T cells. In humans, antigen-experienced CD62Lhi (CCR7+) T cells have been originally described as TCM, distinguishable from naive T cells by the switch from CD45RA to CD45RO expression.49 They circulate between blood and lymph nodes and show interleukin-15–dependent long-term survival with low turnover but are known to proliferate extensively after antigen re-encounter. They are mainly recruited in case of inefficient antigen clearance by local CD62Llo effector memory T cells in order to refill the waning effector and effector memory T-cell compartments.50 How TCM are generated and sustained during primary and secondary antigen challenge, respectively, is intensively discussed in the field.51 Recent data from single-cell transfer experiments in mice are in favor of the so-called progressive differentiation model, which postulates an unidirectional developmental pathway from long-lived TCM to terminally differentiated short-lived effector T cells.28 In consequence, TCM-containing antiviral T-cell populations should be the better choice for long-term protectiveness as required for prophylactic applications. This would be fully in line with recent studies postulating advantageous (and even stem cell-like) characteristics of relatively undifferentiated human CD62Lhi memory T cells for adoptive T-cell transfer.26,27,52 Whatever the optimal subset definition for potent CD62Lhi T memory cells might finally be, it will be crucial for prophylactic T-cell products to preserve them during selection, restimulation, or in vitro expansion.52 Direct transfer of minimally manipulated T cells after gentle ex vivo purification with reversible Streptamers should be very effective for that purpose, as supported by the results from lowest-cell-dose transfers in mice (Figure 3). Because circulating TCM are found only in small frequencies among human CMV-specific CD8+ T cells,53 the actual number of transferred TCM into the HSCT recipients of our study (Figures 4 and 5) must have been extremely low, indicating the potency of direct ex vivo selection of this particular T-cell subset for clinical T-cell transfer strategies. By that, our data implicate that in contrast to classical antiviral medication, T-cell therapy does not follow a linear dose-effect relation but can create protective immunity out of the lowest T-cell numbers.
In summary, minimally manipulating (ex vivo) isolation protocols of pathogen-specific T cells, which preserve presumably protective CD62Lhi memory T cells, could be the key to effective but safe prophylactic T-cell transfers in TCD allo-HSCT patients. Prophylactic and preemptive use of an entire MHC-Streptamer–enriched CMV-specific CD8+ T population in allo-HSCT patients is currently being tested in phase 1/2 and 3 trials (Eudra-CT: 2006-006146-34, #NCT01077908 and #NCT01220895). If safe and effective, the recently described ex vivo purification of memory T-cell subsets54 might become an interesting complementary tool to specifically target the donor-derived CD62Lhi memory subset for “low-dose” adoptive transfer and to extend their prophylactic use in TCD HSCT patients to further (including CD4-restricted) pathogen epitopes and entities.
The online version of this article contains a data supplement.
There is an Inside Blood commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by the SFB (Sonderforschungsbereich/Collaborative Research Centre) TR36 (TP-A10).
Authorship
Contribution: M.N., C.S., P.G., G.D., J.A., M.O., F.A., V.R.B., and M.S. performed experiments; C.S., M.N., M.O., and J.A. analyzed the data; G.G. provided MVA; M.N., C.S., and D.H.B. conceived the study and planned the murine experiments; G.U.G., F.R.S., A.B., and B.V. were responsibly involved in patient treatment; D.H.B., H.E., T.T., E.S., and L.G. performed and supervised the clinical cell selection; and M.N., D.H.B., and C.S. wrote the paper.
Conflict-of-interest disclosure: L.G. is a member of and holds shares in Stage Cell Therapeutics Ltd. D.H.B. invented the Streptamer technology and holds shares of Stage Cell Therapeutics Ltd. All other authors declare no competing financial interests.
The current affiliation for G.G. is Howard Hughes Medical Institute and Immunology Program, Memorial Sloan-Kettering Cancer Center, New York, NY.
Correspondence: Michael Neuenhahn, Institute for Medical Microbiology, Immunology and Hygiene, Technische Universität München, Trogerstrasse 30, 81675 Munich, Germany; e-mail: michael.neuenhahn@tum.de.
References
Author notes
D.H.B. and M.N. contributed equally to this study.