Key Points
Phagocytosis of IgG-opsonized blood cells by human macrophages is inhibited by intravenous immunoglobulins.
This inhibition is independent of IgG-Fc sialylation but improves with IgG preparations that bind FcγRs more avidly.
Abstract
In immune thrombocytopenia and warm autoimmune hemolytic anemia, circulating immunoglobulin G (IgG)-opsonized blood cells are cleared from the circulation by macrophages. Administration of intravenous immunoglobulin (IVIg) can prevent uptake, but the exact working mechanism is not known. The prevailing theory from murine studies, which states that Fc-sialylated IgG alters the balance between activating and inhibitory Fc-gamma receptors (FcγRs) by inducing upregulation of the inhibitory FcγRIIb on effector macrophages, is currently debated. We studied phagocytosis of IgG-opsonized blood cells in a human system, assessing the effect of IVIg and blocking anti-FcγR F(ab′)2 fragments on uptake by monocyte-derived macrophages (both M1 and M2 macrophages). Phagocytosis was remarkably sensitive to administration of IVIg, but unexpectedly, recombinant Fc-sialylated IgG or sialic acid-enriched IVIg were equally active as unsialylated IgG fractions in mediating this inhibition, independent of FcγRIIb expression. Instead, IVIg inhibited phagocytosis by direct blockade of FcγRs. IgG fractions enriched for IgG dimers with enhanced avidity for FcγRs showed increased inhibition compared with monomeric IgG fractions. Together, our data demonstrate that inhibition of IgG-mediated phagocytosis in human macrophages by IVIg is dependent on the capacity to directly bind FcγRs but is independent of FcγRIIb or sialylation of the Fc fragment in the human setting.
Introduction
Human immunoglobulin G (IgG) antibodies directed against blood cells can cause destruction of these cells, leading to anemia or thrombocytopenia. This occurs, for instance, in warm antibody autoimmune hemolytic anemia (wAIHA) or immune thrombocytopenia (ITP), in which IgG auto-antibodies against erythrocytes or thrombocytes, respectively, are formed. These IgG-opsonized blood cells are cleared by macrophages in the spleen and liver, which recognize and destroy IgG-opsonized cells by Fc-gamma receptors (FcγRs).1 Human FcγRs are divided into high-affinity receptors (FcγRI [CD64], which has a high affinity for its ligand2 ) and low-affinity receptors (the different isoforms of FcγRs II [CD32] and III [CD16], which have a lower affinity for IgG and bind monomeric IgG less efficiently than FcγRI, but do bind to dimeric and multimeric IgG).2,3 Five of these human FcγRs potentially play a role in the phagocytosis of IgG-opsonized blood cells by macrophages. The classical activating FcγRs (FcγRI, FcγRIIa, and FcγRIIIa) are all independently capable of inducing phagocytosis by monocyte-derived macrophages when crosslinked,4 but the relative contributions of each of these receptors to phagocytosis of IgG-opsonized particles by different types of macrophages are not well known. FcγRIIc, an activating receptor that is expressed only in a minority of individuals, may also play a role, and its presence has been shown to contribute to ITP susceptibility.5 In contrast, FcγRIIb, the only inhibitory FcγR, has been reported to inhibit the prophagocytic signals.6
Therapeutic strategies for the treatment of ITP and wAIHA include the administration of intravenous immunoglobulin (IVIg).7-9 IVIg is a first-line treatment of ITP in situations in which a rapid increase in the number of platelets is warranted.8 Although many different modes of action for the immune-modulating effect of IVIg have been proposed, the exact mechanism by which IVIg immediately alleviates the clearance of IgG-opsonized blood cells is still debated. The therapeutic effects of IVIg are somewhat surprising, considering that its main component, IgG, is normally present in plasma at high concentrations. Possibly, a specific fraction of the IgG present in IVIg preparations is responsible for the therapeutic effect. Because high doses of 1 to 2 g/kg of IVIg are needed to induce a good therapeutic response, more-targeted therapies may potentially be developed. It is known that the effect of IVIg lies within the Fc fragments of the IgG, because purified Fc fragments alone were an effective treatment of ITP,10 whereas IVIg preparations depleted of Fc fragments were not effective.11 Direct blockade of the FcγRs by the Fc fragments of IgG molecules is one of the possible explanations,1,12 and IgG dimers and IgG multimers (present at low concentrations in IVIg) have been implicated as an active fraction13,14 because of their capacity to more efficiently bind and block low-affinity FcγRs. Several murine studies have indeed suggested IgG dimers to be the most effective part of IVIg in ameliorating ITP,13-16 although a recent report showed that they are not absolutely required, as purely monomeric fractions were also able to ameliorate murine ITP.17
During the last decade, however, the focus of research on immune modulation by IVIg has shifted to the role of the inhibitory FcγRIIb and glycosylation of IgG molecules at the Fc tail. Upregulation of FcγRIIb on splenic macrophages was implicated as the working mechanism of IVIg in a mouse model of ITP.18 Since then, several reports have suggested that the minor IgG fraction with sialic acid-containing N-linked glycans at Asn297 in the Fc region is important for this immune-modulating effect of IVIg.19-21 This has led to a model for IVIg activity in ITP in which sialylated IgG binds to specific ICAM-3 grabbing nonintegrin-related 1 or its human homolog dendritic cell-specific intercellular adhesion molecule-3-grabbing nonintegrin on macrophages, leading to increased expression of the inhibitory FcγRIIb on effector macrophages.22-24 However, sialylation did not affect efficacy of IVIg in 2 other reports using mouse models of ITP.25-27 Taken together, the studies in mouse models are inconclusive with regard to the working mechanism of specific fractions of IVIg.
In addition to these inconsistent results in murine models, human FcγRs are very different from those in mice. Therefore, we set out to directly compare the different components of IVIg in a fully human in vitro system. Using monocyte-derived macrophages, we studied the effect on the phagocytosis of human erythrocytes that were opsonized with a human polyclonal anti-RhD serum. The study revealed that IVIg had a direct blocking effect on phagocytosis, which was even stronger in the presence of dimeric and multimeric IgG preparations, whereas sialic acid-enriched fractions of IVIg or recombinant Asn297-α2,6sialic acid-containing IgG did not show increased effects. Saturation of FcγRI and FcγRIIa were sufficient to explain the inhibitory effects of IVIg, whereas no inhibitory role could be ascribed to FcγRIIb in human macrophages.
Materials and methods
Human samples
Heparinized blood samples were obtained from healthy volunteers. The study was approved by the Medical Ethics Committee of the Academic Medical Center and was performed in accordance with the Declaration of Helsinki.
Culture of monocyte-derived macrophages
Monocytes were isolated from peripheral blood mononuclear cells with a CD14 MACS isolation kit (Miltenyi Biotec). Cells were cultured in 6-well (1 × 106 cells/well) or 24-well (0.2 × 106 cells/well) plates in complete Iscove modified Dulbecco medium (Gibco) containing 10% fetal calf serum (Bodinco, Alkmaar, The Netherlands) and antibiotics, stimulated with either 50 ng/mL macrophage colony-stimulating factor (M-CSF; eBioscience) or 10 ng/mL granulocyte-macrophage colony-stimulating factor (GM-CSF; Peprotech) for 9 days.
Phagocytosis assay
Erythrocytes of donors positive for the RhD blood group were isolated and stained with cell tracker carboxyfluorescein diacetate succinimidyl ester (CFSE; Life technologies) for 30 minutes, and were subsequently opsonized with clinical-grade human anti-RhD antibody (RheDQuin, Sanquin, The Netherlands) at 1.56 IE/mL for 30 minutes, after which excess anti-RhD antibody was washed away or was left unopsonized.
Erythrocytes were added to macrophages in the 24-well plates in which they were cultured at a ratio of 10 erythrocytes to 1 macrophage, and were incubated at 37°C for 20 minutes (M-CSF macrophages) or 2 hours (GM-CSF macrophages). Phagocytosis was stopped by transferring cells to ice, and erythrocytes that were not phagocytosed were lysed twice, using an isotonic ammonium chloride lysis buffer at 4°C for 5 minutes. Lysis buffer was washed away with phosphate-buffered saline (PBS). Microscopy pictures were taken with an EVOS microscope (Life Technologies), and macrophages were subsequently detached from the surface of culture plates by vigorous pipetting after a 15-minute incubation with a PBS buffer containing 125 mM lidocaine (Sigma Aldrich) and 10 mM EDTA (Merck). Ingestion of CFSE-positive erythrocytes by macrophages was quantified by flow cytometry on a FACS CANTO II (BD Biosciences). IgG-mediated phagocytosis was calculated as percentage positive macrophages minus the percentage positive macrophages of the unopsonized control.
Specific monoclonal antibodies (MoAbs) or their fragments to block phagocytosis were incubated with the macrophages for 5 minutes before the addition of erythrocytes, all at 10 μg/mL; intact anti-CD64 clone 10.1 (BioLegend), F(ab′)2 fragment anti-CD64 clone 10.1 (Ancell), F(ab′)2 fragment anti-CD32 clone 7.3 (Ancell), Fab fragment anti-CD32b clone 2B6 (a generous gift from Macrogenics), F(ab′)2 fragment anti-CD16 clone 3G8 (Ancell) and F(ab′)2 fragment of mouse IgG1 isotype control (Ancell). Different IVIg preparations were also added 5 minutes before the start of phagocytosis, unless indicated otherwise. Data from blocking of phagocytosis are shown normalized to unblocked IgG-mediated phagocytosis. Experiments with less than 5% IgG-mediated phagocytosis (only 6/138 experiments) were excluded from analysis in blocking studies.
Preparation of monomeric and dimeric IgG
Normal IVIg was Nanogam 50 mg/mL (Sanquin, The Netherlands). Nanogam was fractionated into different-size components in the following way: 2 mL Nanogam (containing 50 mg/mL polyclonal IgG) was fractionated with LC-SEC (AKTA system, GE Healthcare, Sweden), using Superdex200 column 16/60 and PBS at pH 7.4 as elution buffer. The fraction corresponding to dimeric IgG was pooled from several runs.
Dimeric idiotype-anti-idiotype immune complexes were generated starting from equimolar amounts of a human IgG1 monoclonal anti-adalimumab antibody 2.6 (described previously28 ) and adalimumab (human IgG1; AbbVie). The composition of each preparation was analyzed by injecting 50 μL of 30 mg/mL (Nanogam), 3 mg/mL (dimer-enriched IVIg), or 100 μg/mL (adalimumab/anti-adalimumab complexes) into LC_SEC using superdex200 column 10/30, with PBS at pH 7.4 as an elution buffer.
IgG preparations with altered levels of galactosylation and sialylation
Fractions of IVIg enriched or depleted for sialic acid by Sambucus nigra agglutinin (SNA) were prepared as described previously.25 Neuraminidase treatment of IVIg was performed essentially as described previously19,26 (see the supplemental Methods available on the Blood Web site for details). Recombinant IgG was enriched for sialic acid-Fc by cotransfection of HEK-293F Freestyle cells with human IgG1 anti-2,4,6-trinitrophenol and galactosyl- and sialyltransferases, as described in detail in the supplemental Methods.
Flow cytometry, mass spectrometry, genotyping, and quantitative mRNA analysis
Flow cytometry for surface expression on monocyte-derived macrophages, mass spectrometry for IgG-Fc glycosylation, genotyping of healthy individuals for FCGR genetic variation, and quantitative messenger RNA analysis of IVIg-stimulated macrophages were performed as described in the supplemental Methods.
Statistical analysis
Statistical analysis was performed using GraphPad Prism 6.02. For comparison of expression levels and the level of IgG-mediated phagocytosis, a Kruskal-Wallis test or Mann-Whitney test was used. For comparison of blocking studies, analysis of variance (ANOVA) was used. When this revealed a P value lower than 0.05 (Bonferroni corrected per figure, uncorrected P values are shown), subsequent testing was performed with unpaired t-tests.
Results
FcγRI, FcγRIIa, FcγRIIb, and FcγRIII are expressed on M-CSF and GM-CSF cultured macrophages
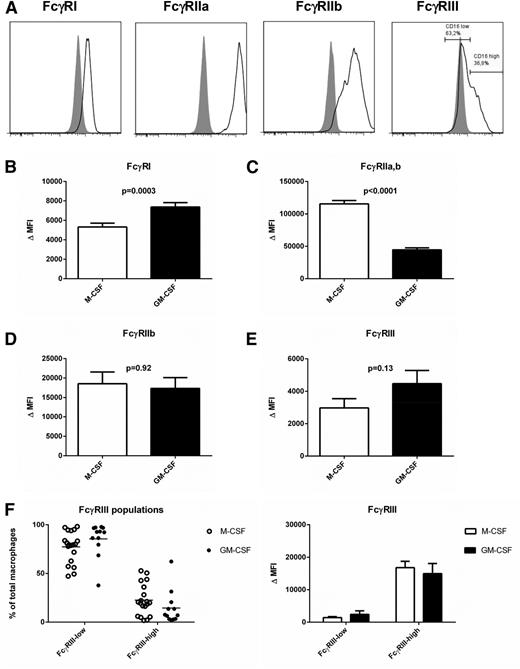
Culturing of peripheral blood monocytes with M-CSF is known to induce differentiation toward a general anti-inflammatory (M2) macrophage phenotype, whereas GM-CSF induces macrophages with a pro-inflammatory (M1) phenotype29 (supplemental Figure 1). When analyzing the expression pattern of the different FcγRs after differentiation with these stimulants for 9 days, we detected FcγRI, FcγRIIa, FcγRIIb, and FcγRIII on the cell surface (Figure 1A-E). Staining with MoAb AT10, recognizing FcγRIIa but also FcγRIIb and FcγRIIc, resulted in the highest fluorescence intensities, especially in the M-CSF macrophages (Figure 1C). To evaluate expression of FcγRIIb, we stained with MoAb 2B6, which actually binds the identical extracellular domains of both FcγRIIb and FcγRIIc.30 To ensure specificity for FcγRIIb, we excluded individuals carrying the open reading frame allele of FCGR2C from this analysis. FcγRIIb expression was indistinguishable for M-CSF and GM-CSF macrophages (Figure 1D), indicating that the observed increased FcγRII expression originated from FcγRIIa. Whereas FcγRI and FcγRII isoforms were always present on the whole population of macrophages, FcγRIIIa showed a bimodal distribution (Figure 1A), with very low or absent expression on the majority of cells, but higher expression on a subset of the macrophages (Figure 1F). A time course of the expression levels during differentiation into macrophages revealed that FcγRI was re-expressed on the macrophages, after an initial decrease, compared with levels on monocytes, whereas expression levels of the other FcγRs steadily increased (supplemental Figure 2).
FcγR expression on monocyte-derived macrophages. (A) Histograms showing expression levels of different FcγRs in monocyte-derived macrophages cultured for 9 days with M-CSF. Gray shading: relevant isotype control (B-E) comparison of expression levels of FcγRI, FcγRIIa,b, FcγRIIb, and FcγRIII between M-CSF and GM-CSF macrophages. Data represent the mean of experiments with macrophages from 34 individuals, or 22 independent experiments in the case of FcγRII (including only individuals without an FCGR2C-open reading frame). Some individuals were measured twice; means of the measurements were used for these individuals. Error bars represent standard error of the mean, statistics with Mann-Whitney test. (F) Percentages of FcγRIII-low and FcγRIII-high macrophages (left, individual experiments are shown) and comparison of the expression levels of the low and high populations (right, data represent the mean and standard error of the mean of at least 12 individuals).
FcγR expression on monocyte-derived macrophages. (A) Histograms showing expression levels of different FcγRs in monocyte-derived macrophages cultured for 9 days with M-CSF. Gray shading: relevant isotype control (B-E) comparison of expression levels of FcγRI, FcγRIIa,b, FcγRIIb, and FcγRIII between M-CSF and GM-CSF macrophages. Data represent the mean of experiments with macrophages from 34 individuals, or 22 independent experiments in the case of FcγRII (including only individuals without an FCGR2C-open reading frame). Some individuals were measured twice; means of the measurements were used for these individuals. Error bars represent standard error of the mean, statistics with Mann-Whitney test. (F) Percentages of FcγRIII-low and FcγRIII-high macrophages (left, individual experiments are shown) and comparison of the expression levels of the low and high populations (right, data represent the mean and standard error of the mean of at least 12 individuals).
Macrophages phagocytose erythrocytes opsonized by human anti-RhD IgG
To assess the capacity of the macrophages to phagocytose IgG-opsonized blood cells, we used a phagocytosis assay with RhD-positive human erythrocytes opsonized with polyclonal human anti-RhD antibodies as the phagocytic target. Incubation of IgG-opsonized erythrocytes with the macrophages at 37°C led to binding and phagocytosis (Figure 2A). To distinguish binding from phagocytosis, noningested extracellular erythrocytes were lysed (Figure 2A). This efficiently lysed all noningested erythrocytes, as no erythrocytes could be detected after lysis in macrophages pretreated with cytochalasin B, which inhibits phagocytosis by interfering with actin polymerization (Figure 2B). Phagocytosis was quantified by CFSE labeling of the erythrocytes and detection of macrophages that have taken up 1 or more erythrocytes by flow cytometry (Figure 2B). A time course showed that phagocytosis was faster and more extensive in M-CSF macrophages than in GM-CSF macrophages (Figure 2C). Overnight incubation did not increase the percentage of positive macrophages in GM-CSF cultures (data not shown). Incubation times of 20 minutes (M-CSF) and 2 hours (GM-CSF) were chosen as optimal times for read-out and were used in all subsequent experiments. An overview of the range of phagocytosis at these points is given in Figure 2D. The extent of phagocytosis was not significantly correlated to FcγR expression levels (data not shown) or to single nucleotide polymorphisms in the low-affinity FcγRs (supplemental Figure 3).
Phagocytosis of anti-RhD opsonized erythrocytes by monocyte-derived macrophages. (A) RhD-positive erythrocytes opsonized with anti-RhD after phagocytosis by monocyte-derived macrophages cultured for 9 days, before (left) and after (right) lysis of erythrocytes. (B) Representative images of the quantification of phagocytosis by flow cytometry. Unopsonized or anti-RhD opsonized CFSE-labeled RhD-positive erythrocytes were incubated with macrophages in the presence or absence of cytochalasin B. Percentages indicated the percentage CFSE-positive macrophages relative to the total macrophage population. Data are representative of at least 6 (cytochalasin B) experiments. (C) Time course of phagocytosis of anti-RhD opsonized erythrocytes by M-CSF and GM-CSF macrophages. Data are representative of 3 independent experiments. Error bars represent standard error of the mean. (D) Comparison of IgG-mediated phagocytosis (corrected for unopsonized phagocytosis) for M-CSF and GM-CSF macrophages (note different points). Mean and dots represent experiments with macrophages of different individuals (n = 58 for M-CSF, n = 55 for GM-CSF). Some individuals were measured twice; the mean of the measurements is shown for these individuals. Statistics with Mann-Whitney test.
Phagocytosis of anti-RhD opsonized erythrocytes by monocyte-derived macrophages. (A) RhD-positive erythrocytes opsonized with anti-RhD after phagocytosis by monocyte-derived macrophages cultured for 9 days, before (left) and after (right) lysis of erythrocytes. (B) Representative images of the quantification of phagocytosis by flow cytometry. Unopsonized or anti-RhD opsonized CFSE-labeled RhD-positive erythrocytes were incubated with macrophages in the presence or absence of cytochalasin B. Percentages indicated the percentage CFSE-positive macrophages relative to the total macrophage population. Data are representative of at least 6 (cytochalasin B) experiments. (C) Time course of phagocytosis of anti-RhD opsonized erythrocytes by M-CSF and GM-CSF macrophages. Data are representative of 3 independent experiments. Error bars represent standard error of the mean. (D) Comparison of IgG-mediated phagocytosis (corrected for unopsonized phagocytosis) for M-CSF and GM-CSF macrophages (note different points). Mean and dots represent experiments with macrophages of different individuals (n = 58 for M-CSF, n = 55 for GM-CSF). Some individuals were measured twice; the mean of the measurements is shown for these individuals. Statistics with Mann-Whitney test.
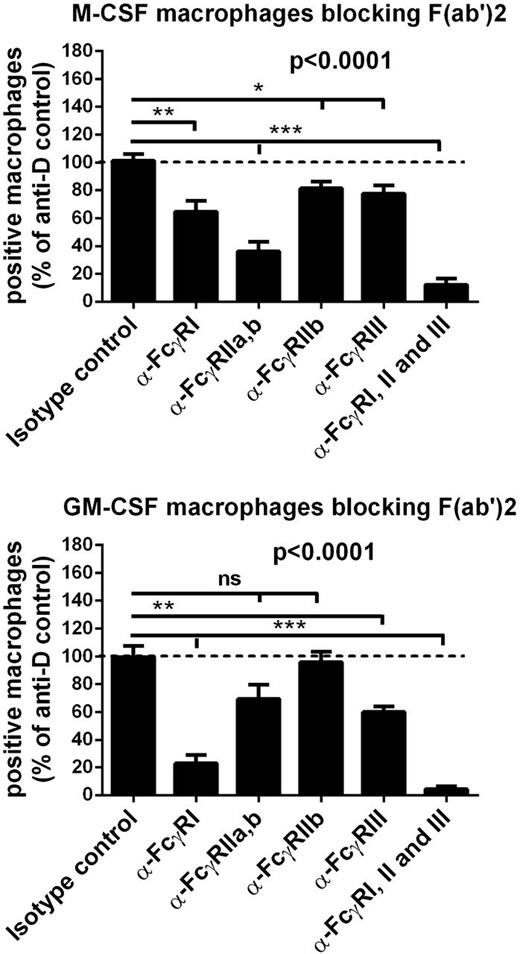
Differential role of FcγRs in M-CSF and GM-CSF macrophages
To determine the relative contribution of the different FcγRs to the phagocytosis of IgG-opsonized erythrocytes, we used FcγR-specific blocking F(ab′)2 fragments. The combination of F(ab′)2 fragments against all FcγRs induced an almost complete inhibition of phagocytosis, especially in GM-CSF macrophages (Figure 3). The blocking F(ab′)2 against FcγRII in M-CSF macrophages was strongest, whereas F(ab′)2 against FcγRI had the most effect in inhibiting phagocytosis with GM-CSF macrophages. Blocking Fab fragments of MoAb 2B6 (against FcγRIIb) and F(ab′)2 fragments (against FcγRIII) had only a minor effect in both types of macrophages. Whereas the MoAbs against FcγRII (clone 7.3), FcγRIIb (clone 2B6), and FcγRIII (clone 3G8) that we used recognize the IgG binding site of the FcγRs and block IgG binding as F(ab′)2 fragments,31-33 blocking experiments with F(ab′)2 fragments of MoAb 10.1 were more difficult to interpret because the epitope of FcγRI recognized by this antibody is not located at the IgG-binding site itself, although it is close enough to interfere with binding.34 To compare the blocking capacity of 10.1 F(ab′)2 fragments to intact 10.1, we performed a rosetting assay with FCGR1A1-transfected 293T cells (supplemental Figure 4A-C). This revealed that intact 10.1 was able to completely inhibit binding of IgG-opsonized erythrocytes to FcγRI at the concentration used in our phagocytosis assay, but F(ab′)2 fragments could not inhibit binding completely, even at high concentrations. In fact, when intact 10.1 was used in the phagocytosis assay, inhibition was much more striking in both types of macrophages (supplemental Figure 4D), and phagocytosis could be completely inhibited with a combination of intact antibodies against all 3 FcγRs. However, with the use of intact antibodies, blocking of other FcγRs through the Fc fragment (Kurlander phenomenon35 ) cannot be excluded.
M-CSF macrophages phagocytose mainly through FcγRIIa, whereas GM-CSF macrophages phagocytose mainly through FcγRI. Effect of FcγR receptor blocking F(ab′)2 (α-FcγRI, α-FcγRIIa,b, α-FcγRIII) or Fab (α-FcγRIIb) fragments on the phagocytosis of anti-RhD IgG-opsonized erythrocytes. Data are normalized against phagocytosis of unblocked macrophages. For experiments with Fab α-FcγRIIb individuals with an FCGR2C-open reading frame are excluded. Data represent means and standard error of the mean from 5 to 12 independent experiments. P values indicate results of 1-way ANOVA; subsequent unpaired t-tests were performed with results depicted as follows: *P < .05, **P < .01, ***P < .001 (Bonferroni-corrected P values).
M-CSF macrophages phagocytose mainly through FcγRIIa, whereas GM-CSF macrophages phagocytose mainly through FcγRI. Effect of FcγR receptor blocking F(ab′)2 (α-FcγRI, α-FcγRIIa,b, α-FcγRIII) or Fab (α-FcγRIIb) fragments on the phagocytosis of anti-RhD IgG-opsonized erythrocytes. Data are normalized against phagocytosis of unblocked macrophages. For experiments with Fab α-FcγRIIb individuals with an FCGR2C-open reading frame are excluded. Data represent means and standard error of the mean from 5 to 12 independent experiments. P values indicate results of 1-way ANOVA; subsequent unpaired t-tests were performed with results depicted as follows: *P < .05, **P < .01, ***P < .001 (Bonferroni-corrected P values).
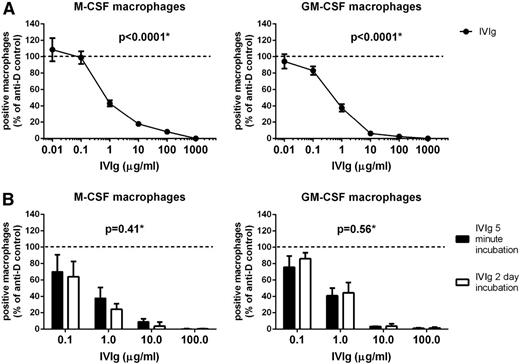
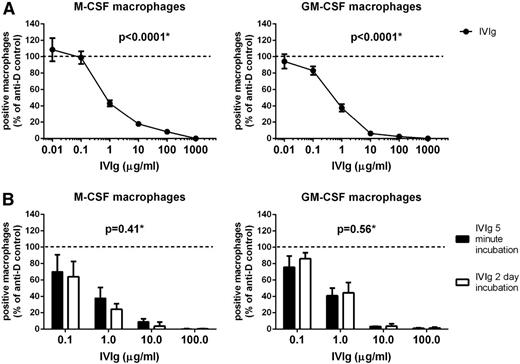
IVIg directly inhibits phagocytosis of IgG-opsonized erythrocytes
IVIg has previously been shown to be able to inhibit macrophage phagocytosis of IgG-opsonized erythrocytes in experimental setups in which macrophages were incubated for 1 hour with IVIg, after which the IVIg was washed away before the start of phagocytosis.14,36 To test whether IVIg also had the capacity to directly inhibit IgG-mediated phagocytosis in our in vitro system, we added IVIg to our macrophages just before starting the phagocytosis. IVIg inhibited phagocytosis in a dose-dependent manner, with doses as low as 1 μg/mL still showing some effect in both types of macrophages (Figure 4A). IVIg was equally effective when added 2 days before phagocytosis was initiated (Figure 4B).
IVIg directly inhibits phagocytosis of IgG-opsonized erythrocytes. (A) Dose-response curve of IVIg inhibiting the phagocytosis of anti-RhD IgG-opsonized erythrocytes by monocyte-derived macrophages cultured with M-CSF (left) and GM-CSF (right). IVIg was added 5 minutes before the start of phagocytosis. Data represent means and standard error of the mean of at least 9 experiments for each concentration. (B) Comparison of the inhibiting effect on phagocytosis when IVIg was added 2 days or 5 minutes before the incubation with erythrocytes. Means and standard error of the mean of at least 3 experiments are shown. P values in this figure were determined using 1-way (A) or 2-way (B) ANOVA.
IVIg directly inhibits phagocytosis of IgG-opsonized erythrocytes. (A) Dose-response curve of IVIg inhibiting the phagocytosis of anti-RhD IgG-opsonized erythrocytes by monocyte-derived macrophages cultured with M-CSF (left) and GM-CSF (right). IVIg was added 5 minutes before the start of phagocytosis. Data represent means and standard error of the mean of at least 9 experiments for each concentration. (B) Comparison of the inhibiting effect on phagocytosis when IVIg was added 2 days or 5 minutes before the incubation with erythrocytes. Means and standard error of the mean of at least 3 experiments are shown. P values in this figure were determined using 1-way (A) or 2-way (B) ANOVA.
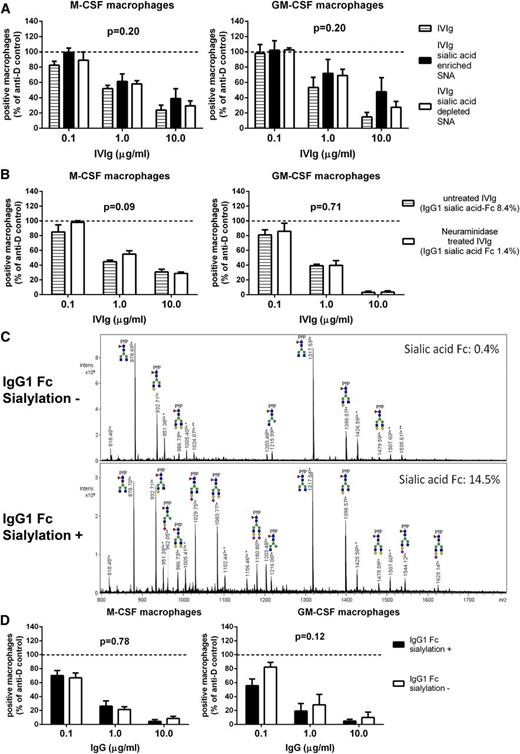
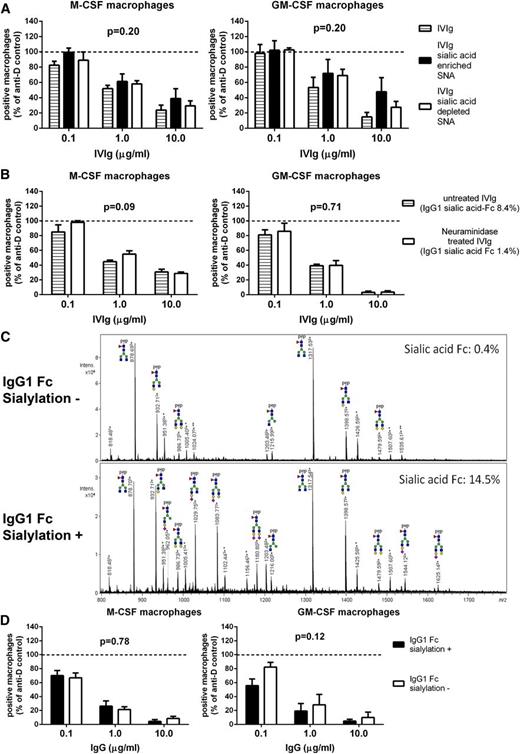
Inhibition of phagocytosis by IVIg is independent of Fc-sialylation and does not require an increase of FcγRIIb expression
The inhibitory effect of sialylated IVIg was first reported using an enrichment by Sambucus nigra agglutinin (SNA) lectin fractionation.19 When we used preparations that were enriched or depleted for sialic acid in this way, we could not detect any differences in capacity to inhibit phagocytosis (Figure 5A). However, enrichment of IVIg for sialic acid by SNA lectin fractionation only results in an enrichment of Fab-sialylated, but not Fc-sialylated, IgG.25,37 Because the presumed effects of sialylated IgG would be Fc-sialic acid-specific,21 we subsequently used neuraminidase-treated IVIg to determine whether a preparation depleted of Fc sialic acid was still capable of inhibiting phagocytosis. Despite the fact that neuraminidase removed almost 85% of the sialic acid residues at the N297-linked glycan, neuraminidase-treated IVIg was equally as effective as untreated IVIg (Figure 5B). Finally, we tried an IgG preparation that was enriched or depleted for sialic acid Fc by using a non-Fab-glycosylated recombinant anti-2,4,6-trinitrophenyl MoAb, enriched for Fc sialylation by expressing the antibody with or without galactosyltransferases and sialyltransferases. This resulted in an α2,6-sialic acid content of 14.5% in the Fc-sialylated IgG and 0.4% in non-Fc-sialylated IgG (Figure 5C). These were equally capable of inhibiting phagocytosis, showing that the inhibition of phagocytosis was completely independent of IgG-Fc sialylation status (Figure 5D).
Inhibition of phagocytosis by IVIg is not enhanced in fractions enriched for sialic acid. (A) Inhibition of phagocytosis by IVIg enriched or depleted for sialic acid by SNA fractionation. Means and standard error of the mean of at least 4 experiments for each concentration are shown. (B) Inhibition of phagocytosis by IVIg treated with neuraminidase to remove sialic acid residues compared with sham-treated IVIg. The level of sialylation of IVIg was determined by mass spectrometry as in panel C, the results of which are indicated by percentages in the figure. Means and standard error of the mean of 4 experiments for each concentration are shown. (C) Example of mass spectrometry spectra, in this case showing trypsin-generated glycopeptides of anti-trinitrophenol IgG1 produced in the absence (IgG1 Fc sialylation-negative) or presence (IgG1 Fc sialylation-positive) of galactosyl- and sialyltransferase. Percentage Fc-sialylation is indicated. A minority of the peaks appear to belong to glycopeptides with a modified peptide mass and are labeled accordingly: *mass increase of +218.1 Da, **mass increase of +436.2 = 2 × 218.1 Da. Pep, peptide; green circle, mannose; yellow circle, galactose; blue square, N-acetylglucosamine; red triangle, fucose; purple diamond, N-acetylneuraminic acid (sialic acid). (D) Inhibition of phagocytosis by recombinant human IgG1 from panel C with very low or enhanced Fc-sialylation. Means and standard error of the mean of at least 5 experiments for each concentration are shown. P values in this figure were determined using 2-way ANOVA.
Inhibition of phagocytosis by IVIg is not enhanced in fractions enriched for sialic acid. (A) Inhibition of phagocytosis by IVIg enriched or depleted for sialic acid by SNA fractionation. Means and standard error of the mean of at least 4 experiments for each concentration are shown. (B) Inhibition of phagocytosis by IVIg treated with neuraminidase to remove sialic acid residues compared with sham-treated IVIg. The level of sialylation of IVIg was determined by mass spectrometry as in panel C, the results of which are indicated by percentages in the figure. Means and standard error of the mean of 4 experiments for each concentration are shown. (C) Example of mass spectrometry spectra, in this case showing trypsin-generated glycopeptides of anti-trinitrophenol IgG1 produced in the absence (IgG1 Fc sialylation-negative) or presence (IgG1 Fc sialylation-positive) of galactosyl- and sialyltransferase. Percentage Fc-sialylation is indicated. A minority of the peaks appear to belong to glycopeptides with a modified peptide mass and are labeled accordingly: *mass increase of +218.1 Da, **mass increase of +436.2 = 2 × 218.1 Da. Pep, peptide; green circle, mannose; yellow circle, galactose; blue square, N-acetylglucosamine; red triangle, fucose; purple diamond, N-acetylneuraminic acid (sialic acid). (D) Inhibition of phagocytosis by recombinant human IgG1 from panel C with very low or enhanced Fc-sialylation. Means and standard error of the mean of at least 5 experiments for each concentration are shown. P values in this figure were determined using 2-way ANOVA.
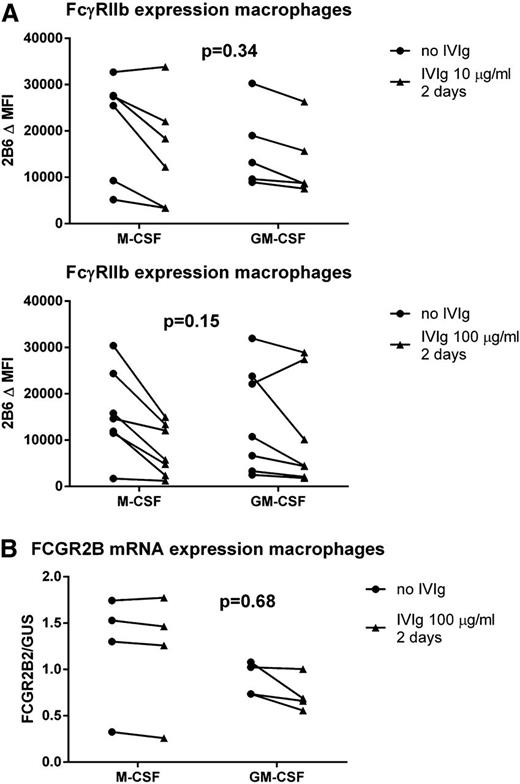
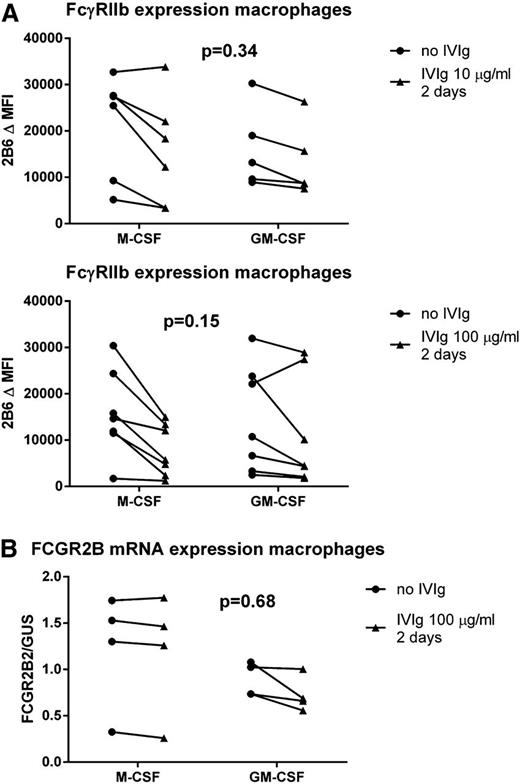
To determine whether the observed inhibitory effects were the result of an upregulation of FcγRIIb, as previously proposed,18 we determined FcγRIIb expression levels by staining macrophages preincubated with IVIg for 2 days with MoAb 2B6. This revealed no increase in expression levels of FcγRIIb in either M-CSF or GM-CSF macrophages (Figure 6A). To rule out the possibility that we could not detect an increased expression of FcγRIIb because of competition of the IgG in IVIg for the binding site of MoAb 2B6, we also measured mRNA levels of FCGR2B in macrophages incubated with IVIg. This revealed no increase in FCGR2B mRNA (Figure 6B). Together, these results indicate that IVIg could inhibit phagocytosis directly, independent of changes in expression of FcγRIIb.
Incubation of macrophages with IVIg at phagocytosis-inhibiting concentrations does not lead to an increased FcγRIIb expression. (A) Staining with MoAb 2B6, corrected for isotype control, in M-CSF or GM-CSF macrophages cultured for 9 days left either unstimulated (circles) or stimulated with 10 μg/mL (upper) or 100 μg/mL (lower) IVIg for 2 days (triangles). (B) FCGR2B2 mRNA expression compared with expression of housekeeping gene GUS, in M-CSF or GM-CSF macrophages cultured for 9 days, left either unstimulated (circles) or stimulated with 100 μg/mL IVIg for 2 days (triangles). Dots represent individual measurements, with lines linking the paired experiments with cells of the same individual. P values in this figure were determined using 2-way ANOVA.
Incubation of macrophages with IVIg at phagocytosis-inhibiting concentrations does not lead to an increased FcγRIIb expression. (A) Staining with MoAb 2B6, corrected for isotype control, in M-CSF or GM-CSF macrophages cultured for 9 days left either unstimulated (circles) or stimulated with 10 μg/mL (upper) or 100 μg/mL (lower) IVIg for 2 days (triangles). (B) FCGR2B2 mRNA expression compared with expression of housekeeping gene GUS, in M-CSF or GM-CSF macrophages cultured for 9 days, left either unstimulated (circles) or stimulated with 100 μg/mL IVIg for 2 days (triangles). Dots represent individual measurements, with lines linking the paired experiments with cells of the same individual. P values in this figure were determined using 2-way ANOVA.
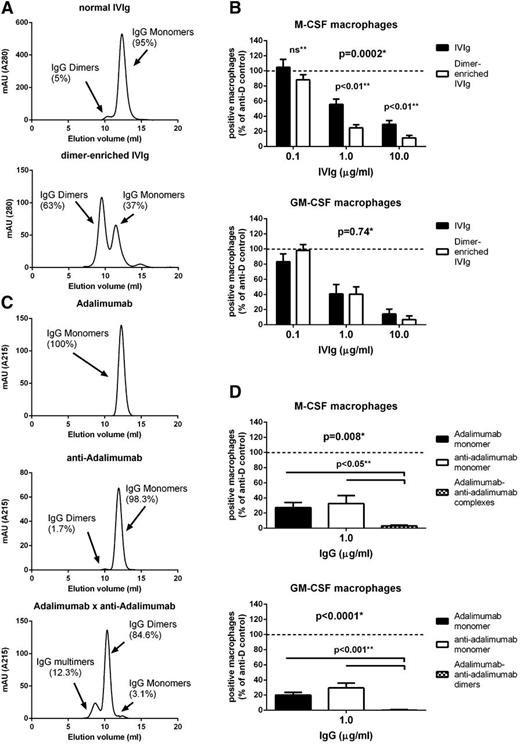
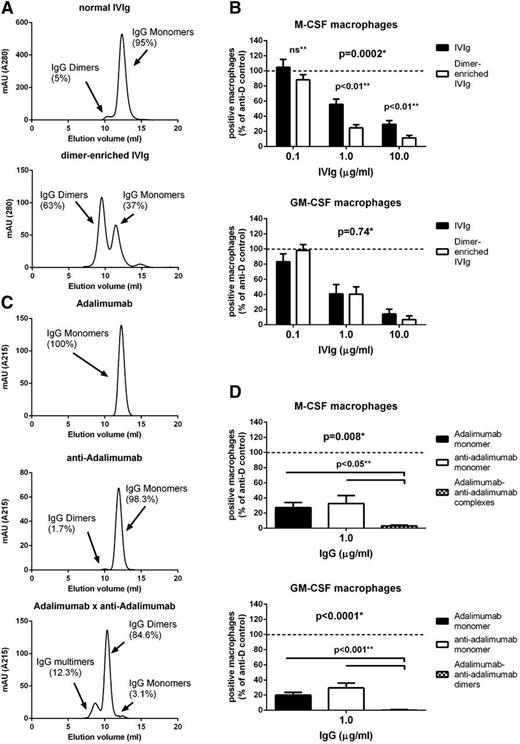
Dimeric IgG most effectively blocks phagocytosis of IgG-opsonized erythrocytes
We then tested whether preparations of IVIg rich in dimeric IgG, with a higher avidity for FcγRs, were more capable of inhibiting phagocytosis. We first prepared a fraction of IVIg enriched for IgG dimers by HPLC fractionation of IVIg, which led to an increase of dimeric IgG from ∼5% to ∼63% (Figure 7A). This fraction was even more effective than normal IVIg in inhibiting phagocytosis in the M-CSF, but not the GM-CSF macrophages (Figure 7B). Subsequently, to test IgG preparations with even higher contents of dimeric IgG, we made use of the ability of a human anti-idiotype MoAb against the TNF-blocking MoAb adalimumab to form complexes with adalimumab.28 Monoclonal fractions of these 2 antibodies consist of IgG monomers, but a combination of the 2 results in the formation of dimers, as well as some multimers (Figure 7C). When using either of the 2 monoclonal antibodies alone, phagocytosis was still inhibited to the same extent as inhibition with normal IVIg, showing that purely monomeric IgG also has an inhibiting effect on phagocytosis. However, the combination of the 2 antibodies, having formed dimers, was much more effective than either of the 2 monoclonal antibodies alone, even in the GM-CSF macrophages (Figure 7D).
IgG dimers are more potent than IgG monomers in inhibiting phagocytosis of IgG-opsonized erythrocytes. (A) High-performance liquid chromatography (HPLC) fractionation of IVIg (top) and IVIg after dimer enrichment by prior HPLC fractionation (bottom). Graphs are representative graphs of at least 4 independent experiments; percentages indicate the average amount of IgG monomers and IgG dimers. (B) Inhibition of phagocytosis by a preparation of IVIg enriched for dimeric IgG by HPLC fractionations compared with normal IVIg, for M-CSF (top) and GM-CSF (bottom). Means and standard error of the mean of at least 8 experiments for each concentration are shown. (C) Representative HPLC graphs of a recombinant human IgG1 (anti-TNF, adalimumab, top), a human monoclonal IgG1 anti-idiotype against adalimumab (anti-adalimumab, middle), and the combination of these 2 MoAbs (adalimumab × anti-adalimumab, bottom) mixed in equimolar amounts, showing the percentages of IgG monomers, dimers, and multimers. Percentages are means of 3 independent experiments. (D) Inhibition of phagocytosis by monoclonal adalimumab and monoclonal anti-adalimumab compared with the combination of these 2 MoAbs. Data represent means and standard error of the mean of at least 8 experiments. P values in this figure: *statistics by 2-way ANOVA, **statistics by Student t-test.
IgG dimers are more potent than IgG monomers in inhibiting phagocytosis of IgG-opsonized erythrocytes. (A) High-performance liquid chromatography (HPLC) fractionation of IVIg (top) and IVIg after dimer enrichment by prior HPLC fractionation (bottom). Graphs are representative graphs of at least 4 independent experiments; percentages indicate the average amount of IgG monomers and IgG dimers. (B) Inhibition of phagocytosis by a preparation of IVIg enriched for dimeric IgG by HPLC fractionations compared with normal IVIg, for M-CSF (top) and GM-CSF (bottom). Means and standard error of the mean of at least 8 experiments for each concentration are shown. (C) Representative HPLC graphs of a recombinant human IgG1 (anti-TNF, adalimumab, top), a human monoclonal IgG1 anti-idiotype against adalimumab (anti-adalimumab, middle), and the combination of these 2 MoAbs (adalimumab × anti-adalimumab, bottom) mixed in equimolar amounts, showing the percentages of IgG monomers, dimers, and multimers. Percentages are means of 3 independent experiments. (D) Inhibition of phagocytosis by monoclonal adalimumab and monoclonal anti-adalimumab compared with the combination of these 2 MoAbs. Data represent means and standard error of the mean of at least 8 experiments. P values in this figure: *statistics by 2-way ANOVA, **statistics by Student t-test.
Discussion
Our data demonstrate that the inhibiting effect of IVIg on the phagocytosis of IgG-opsonized blood cells14,36 is a very direct effect in our fully human in vitro system, as IVIg was effective after a very short incubation time of only 5 minutes. The addition of IVIg to cultured macrophages resulted in a dose-dependent inhibition of phagocytosis of IgG-opsonized erythrocytes, which could be enhanced with preparations containing more IgG dimers and multimers, but was independent of IgG-Fc and IgG-Fab sialylation. Because IgG was effective after a very short incubation, we presume that the most likely working mechanism is a direct blockade of FcγRs.
After the discovery that IVIg induces a steep increase in the circulating platelet counts in ITP,7 many theories regarding the working mechanism have been proposed, including inhibition of phagocytosis as a result of blockade of activating FcγRs. Despite the fact that many observations support this mechanism,1,12,38 the current paradigm is that IVIg induces upregulation of inhibitory FcγRIIb on effector macrophages,18,23 although this was only shown in mice. However, we did not detect any upregulation of this receptor, even after 2 days of incubation with IVIg in our macrophages, clearly showing that IVIg has very potent effects that are independent of an increased expression of FcγRIIb. Although we cannot completely rule out upregulation of FcγRIIb in response to IVIg in vivo, it was recently postulated that this receptor may not actually be required for the protective effect of IVIg in murine models in all circumstances.39 In any case, our findings do not support any role for FcγRIIb in the working mechanism of IVIg in preventing clearance of opsonized blood cells by human macrophages. Neither could we detect a direct effect of sialylation of the N-linked Fc-glycan at position 297 on the clearance of IgG-opsonized blood cells. Our findings, in conjunction with the conflicting results obtained in murine studies of ITP comparing sialic acid-enriched versus sialic acid-depleted IVIg,22,25,26 do not support a role for the sialylation of IgG-Fc in the working mechanism of IVIg preventing uptake of IgG-opsonized blood cells.
Being such a potent direct inhibitor of FcγR-mediated phagocytosis in vitro, we assume that IVIg will also be able to block this process in macrophages in vivo. The notion that FcγRs can be blocked by IgG in vivo may seem surprising, given that IgG is normally present in the circulation at ∼7 to 16 mg/mL, which would be expected to block FcγRs in vivo already under steady state conditions. Monomeric IgG has been shown to bind FcγRIIa.40 Therefore, monomeric IgG will probably form an equilibrium with low-affinity FcγRs in vivo, with a proportion of the low-affinity FcγRs bound by IgG and a proportion freely available. The administration of IVIg could shift this balance toward a higher proportion of FcγRs being occupied, leaving too little FcγRs freely available for binding to IgG-opsonized blood cells. IgG dimers and polymers in IVIg will even more efficiently block the low-affinity FcγRs, as they have a higher avidity.
We indeed found an increased effect of IgG dimers and IgG multimers in our phagocytosis studies, although the presence was not absolutely necessary, and in M1 macrophages, it could only be detected with preparations with a high IgG dimer and IgG multimer content. This differential sensitivity reflects the differences in FcγR usage between M1 and M2 macrophages. Phagocytosis by M-CSF macrophages relies greatly on the low-affinity FcγRII, which is much more effectively blocked by IgG dimers than monomers, whereas GM-CSF macrophages rely more exclusively on FcγRI, which is already fully occupied by IgG monomers alone. Our experiments with F(ab′)2 fragments indicate that FcγRI is relevant to the phagocytosis by monocyte-derived macrophages, especially when cultured with GM-CSF. The effects with the F(ab′)2 fragments will be an underrepresentation of the actual role of FcγRI, as MoAb 10.1 (nor any other available MoAb against FcγRI) does not block efficiently as a F(ab′)2 fragment. However, the effects of the intact 10.1 MoAb may, rather, be an overrepresentation of the role of FcγRI, as the Fc tail can block other adjacent FcγRs, as described by Kurlander.35
Macrophages of the spleen and liver are responsible for the clearance of IgG-opsonized blood cells in vivo, but remarkably little is known about expression levels of FcγRs on these macrophages. It has been proposed that mainly the low-affinity FcγRs are involved,1 based only on circumstantial evidence, such as association studies with genetic polymorphisms in the low-affinity FcγRs5,41 and in vivo blocking studies with specific FcγR MoAbs in limited series of patients.42,43 If it is indeed the case that these macrophages have a predominant expression of low-affinity FcγRs, we may expect the difference between dimeric and monomeric IgG to be even greater than the difference we have found in monocyte-derived macrophages.
In conclusion, the IVIg-induced inhibition of phagocytosis of IgG-opsonized blood cells by human macrophages, in contrast to the current prevailing theory,23 is not dependent on Fc sialylation or FcγRIIb upregulation. The lack of support for this theory from our data in human macrophages is in line with multiple recent studies challenging the concept of Fc sialylation and/or FcγRIIb being important for IVIg efficacy in various diseases, as studied in murine models25,26,39,44 or with human material.37,45,46 Therefore, the importance of IgG Fc sialylation and upregulation of FcγRIIb in IVIg treatment need to be reconsidered.
Instead, the capacity of IgG molecules to bind and block FcγRs seems to be more important, at least when inhibiting phagocytosis of IgG-opsonized blood cells. These findings can help improve the treatment of ITP or wAIHA with IVIg, as preparations with increased binding to low-affinity FcγRs, such as IgG dimers or recombinant engineered IgGs with an increased affinity of the Fc-tail for FcγR, may form suitable alternatives requiring a lower dosage than normal IVIg.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Mrs Ninotska I. L. Derksen and Mrs Ornella Felizolla (Sanquin) and Carolien Koeleman (Leiden University Medical Center) for assistance with the experiments.
This work was supported by a grant from the Landsteiner Foundation for Bloodtransfusion Research (LSBR 0916), and a grant of the Program on Prevention Outcomes Practices (PPOP) “Sweet IVIg: a blend of different tastes” (PPOP-12-001).
Authorship
Contribution: S.Q.N. performed experiments, analyzed data, and wrote the manuscript; G.D., I.K., F.S.v.d.B., J.G., and R.P. performed experiments and analyzed data; M.W., G.V., T.R., and T.K.v.d.B. designed experiments and interpreted and discussed data; and T.W.K. discussed data, designed the study, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Sietse Quirijn Nagelkerke, Sanquin Research, Department of Blood Cell Research, Plesmanlaan 125, 1066 CX Amsterdam, The Netherlands; e-mail: s.nagelkerke@sanquin.nl or s.q.nagelkerke@amc.nl.