Abstract
Background: We reported that mutations in ASXL1, EZH2, IDH1/2 and SRSF2 are negative prognostic variables for survival in primary myelofibrosis (PMF). Patients harboring any one of these mutations comprise IPSS and DIPSS-plus independent high molecular risk (HMR) category. Conversely, prognostic variables in secondary myelofibrosis (sMF), including post-polycythemia vera (PPV) and post-essential thrombocythemia (PET) MF are not defined.
Aims: The aim was to evaluate the correlations of HMR mutational status with hematologic characteristics and clinical presentation, and the role for outcome predition, in PPV- and PET-MF.
Methods: PPV- and PET-MF were diagnosed by IWG-MRT criteria; all pts provided informed consent. Previously published methods were used to screen mutations involving JAK2,MPL, CALR, EZH2, ASXL1, IDH1/2 and SRSF2. The prognostic value of the molecular variables with regard to OS was estimated by the Kaplan-Meier method and Cox regression.
Results: A series of 200 sMF pts from 3 Italian centres was collected: 108 were PPV-MF (54%), 92 PET-MF (46%). PPV-MF cohort: Median age was 65y. Median follow up from PPV-MF diagnosis 4.7y (0.2-25.9y) and median time from PV to PPV-MF 10y (1.08-30.7y). Death occurred in 34 pts (31.8%), 7 pts (6.5%) developed leukemia. Median OS from PPV-MF diagnosis was 9.5y (7.1-11.9y). Frequency of mutations was: JAK2V617F 100% (median allele burden 77%, range 23-100), ASXL1 17.8%, EZH2 3.7%, IDH 5.6%, SRSF2 1%; 29 patients (26.9%) were classified as HMR cases. Hematologic characteristics: median leucocytes 13.0x109/L, hemoglobin 13.3g/dL, platelets 328x109/L, blasts ≥1% 23.4%. Constitutional symptoms in 45.8%, splenomegaly 94.1% (43.3% >10cm from LCM), pruritus 49%; median percentage of BM cellularity was 90% (25-100%) and grade 3 fibrosis in 16.8%. Overall 73 patients were evaluable for karyotype and abnormalities were detected in 42.5%. We did not find significant correlations between individual mutations or HMR category and hematologic and clinical characteristics. PET-MF cohort: Median age was 63.6y. Median follow up from the PET diagnosis 3.3y (0.2-14.5y), median time from ET to PET-MF 11.8y (0.9-30.6y). Death occurred in 30 pts (32.6%), 11 pts (12.0%) developed leukemia. Median OS from PET-MF diagnosis was 9.2y (4.9-13.6y). Frequency of mutations was: JAK2V617F 48.9% (median allele burden 49%, range 0-100), CALR 40.2%, MPL 4.3% and triple negativity (TN) 6.5%; ASXL1 29.3%, EZH2 6.5%, IDH 1.1%, SRSF2 3.3%; 33 pts (35.9%) were HMR. Hematologic characteristics: median leucokytes 8.0x109/L, hemoglobin 10.9 g/dL, platelets 375x109/L, blasts ≥1% 26.4%. Constitutional symptoms 35.4% of pts, splenomegaly 82% (18.2% >10cm from LCM), pruritus i31%; median percentage of BM cellularity was 70% (15-90%) and grade 3 fibrosis was found in 31.7%. Overall 56 patients were evaluable for karyotype and abnormalities were detected in 25.0%. By correlating hematologic and clinical characteristics with unique mutations and HMR category, we found that HMR mutated pts presented greater leukocytosis (P=0.04) and higher JAK2V617F allele burden (P=0.017) than pts in the low-molecular risk –LMR- category (ie, wild-type for ASXL1, EZH2, SRSF2, IDH1/2).
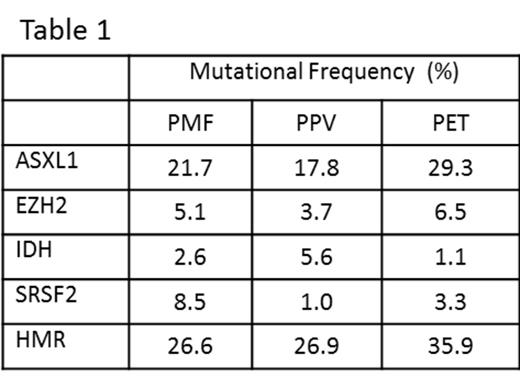
Comparison of PPV-MF and PET-MF: a comparison of hematologic and clinical characteristics according to the diagnosis sMF disclosed that PPV-MF pts presented more frequently splenomegaly (P=0.008; for >10cm from LCM P<0.001), pruritus (P=0.009), abnormal karyotype (P=0.009), increased leukocytes (P<0.001), higher hemoglobin (P<0.001) and BM cellularity (P<0.001) compared with PET-MF. Conversely, PET-MF pts presented higher incidence of grade 3 of BM fibrosis (P=0.04). The median JAK2 allele burden (P<0.001) was higher in PPV-MF pts, while PET-MF pts showed more frequent mutations of ASXL1 (29.3% vs 17.8%; P=0.03).
Univariate analysis disclosed significant correlations between shortened survival and mutated ASXL1 (P=0.02, HR 2.2 95% CI, 1.02-4.8) or EZH2 (P=0.05, HR 5.0 95% CI, 1.0-40.7) in PPV-MF. A HMR category was associated with reduced survival in PPV-MF: median survival 6.1y versus 9.5yr LMR (HR 1.07, 95%CI 1.0-4.4; P=0.04). In PET-MF survival was 4.8y in HMR versus 10.9y in LMR (HR1.6, 95%CI 0.8-3.4; P=0.2).
Conclusion: We conclude that a HMR status is associated with shorter survival in sMF, but the overal impact is narrower than in primary MF, even though the rate of mutations is similar (Table1).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.