To the editor:
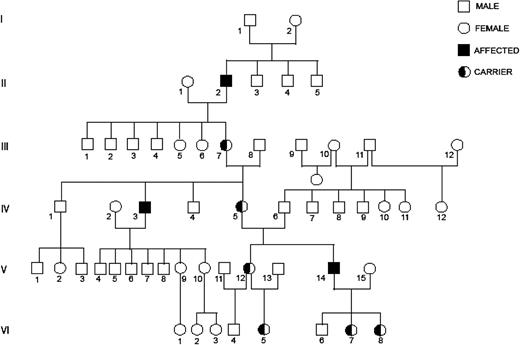
In 1975, Ratnoff and Lewis described a family with an X-linked, moderately severe, inherited bleeding disorder and named it Heckathorn disease after the 34-year-old index patient (patient V-14, Figure 1).1 The patient and his maternal uncle (IV-3), also a bleeder, underwent extensive investigations and were found to have factor VIII deficiency. The functional antihemophilic factor (AHF) level varied from 0.10 to 0.75 U/mL over a 6-year period in patient V-14 and from 0.10 and 1.20 U/mL over a 3-month period in patient IV-3. Four women (IV-5, V-12, VI-5, and VI-8) were identified as obligate carriers. The authors concluded that Heckathorn disease represents a separate form of AHF deficiency and its chief distinguishing feature was the fluctuation of AHF in affected men. They believed that, in time, other families with Heckathorn disease would be identified.
The index patient’s daughter (patient VI-8), who was born in 1964 and had no children, was seen in August 2013 for clearance prior to her spinal surgery. She bruised easily but did not bleed excessively. Her physical examination was unremarkable. A complete blood count, prothrombin time, partial thromboplastin time, factor VIII activity (which was 80% and 121% on 2 occasions), von Willebrand factor studies, and platelet aggregation were normal. Factor VIII gene sequencing showed 1 mild pathogenic mutation (1 copy) with nucleotide change c.908C>A. The amino acid alteration was p. ALA303GLU (traditional nomenclature: ALA284GLU). This finding established her as a carrier of hemophilia A.
Factor VIII is a single-chain peptide with multiple domains known as A1-A2-B-A3-C1-C2.2-4 During clot formation, cleavage of factor VIII increases its procoagulant activity followed by first-order decay in the procoagulant activity and generation of a heterodimer consisting of the A1 and A2 subunits. The A2 subunit dissociates from the A1/A3-C1-C2 in a pH-dependent manner resulting in loss of procoagulant activity.5 Normally, ARG531 lies at the interface of the A1 and A2 subunits. Mutations that directly contact ARG531 (ALA284GLU, ALA284PRO) or are adjacent to it (SER289LEU) are associated with lower clotting activity, especially in assays that use incubation, as is done in 2-stage assays. The A2 subunit can also dissociate spontaneously.5,6
There are 3 hemophilia mutations involving the ARG531 or adjacent region that show increased dissociation of A2 subunit. These are ALA284GLU, ALA284PRO, and SER289LEU. In vitro studies of these missense mutations show a twofold lower activity when the factor VIII assay is done with incubation. When cleaved by thrombin, A2 dissociation is threefold faster for SER289LEU and ALA284GLU.6
Fluctuations in factor VIII levels seen by Ratnoff and Lewis may have resulted from their methods, which involved incubation of plasma7,8 and measurement of AHF activity at 2 different institutions at different times. Also, factor VIII levels are influenced by age, glucose, and insulin levels, fibrinogen level, pregnancy, surgery, hemolytic anemia, and hyperthyroidism.9
In summary, we have shown that Heckathorn disease is hemophilia A due to a missense mutation resulting in nucleotide change c.908C>A and amino acid alteration p. ALA303GLU (traditional nomenclature: ALA284GLU).
Authorship
Contribution: S.N. and A.K. designed the study. All authors interpreted the data and wrote and revised the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Sucha Nand, Loyola University Medical Center, 2160 South First Ave, Maywood, IL 60153; e-mail: snand@lumc.edu.