Abstract
Renal disease is one of the most frequent and severe complications experienced by patients with sickle cell disease; its prevalence is likely to increase as the patient population ages. We recommend regular monitoring for early signs of renal involvement and a low threshold for the use of hydroxyurea as preventative measures for end-stage renal disease. Once renal complications are detected, a careful assessment of the patient is required to rule out other causes of renal disease. Proteinuria and hypertension should be managed aggressively and the patient referred to a specialist nephrology center when progressive decline in renal function is noted. For the few patients who develop advanced chronic kidney disease, timely planning for dialysis and transplantation can significantly improve outcome, and we recommend an exchange blood transfusion policy for all patients on the transplant waiting list and for those with a functioning graft. Alongside the invasive treatment regimes, it is important to remember that renal failure in conjunction with sickle cell disease does carry a significant burden of morbidity and that focusing on symptom control has to be central to good patient care.
Introduction
Patients with sickle cell disease (SCD) are at increased risk of developing a spectrum of renal complications referred to as sickle cell nephropathy (SCN). Some manifestations of SCN are apparent from infancy, but the majority of patients do not develop symptomatic kidney disease. However, in those who progress to severe chronic kidney disease (CKD), this has an enormous impact on both morbidity and mortality.
The following cases highlight some of the particular issues encountered when managing patients with sickle-related renal complications that will be discussed in more detail.
Case 1
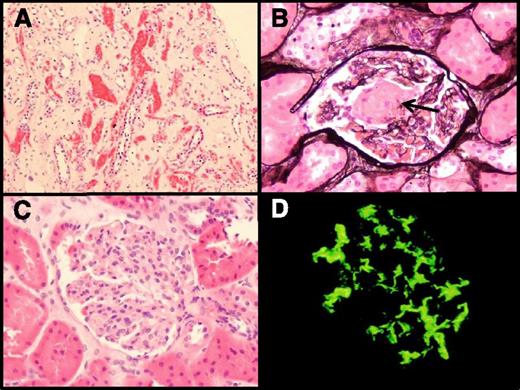
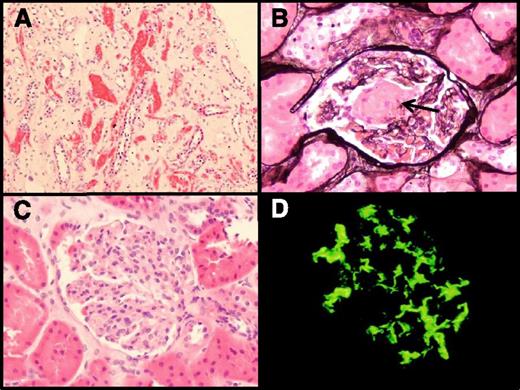
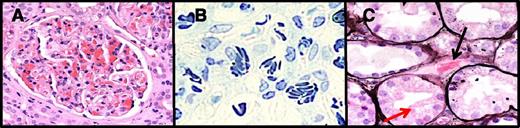
A 36-year-old West African woman with sickle-hemoglobin C (HbSC) disease was noted to have significant proteinuria (urinary protein to creatinine ratio [uPCR] of 103 mg/mmol [911 mg/g]) and a serum creatinine of 83 µmol/L (0.94 mg/dL, estimated glomerular filtration rate [eGFR] of 87 mL/min per 1.73 m2). She was commenced on 2.5 mg of ramipril daily, which was subsequently changed to candesartan 2 mg. Two years later, her uPCR had increased to 208 mg/mmol (1839 mg/g) and her eGFR had fallen to 77 mL/min per 1.73 m2, at which point candesartan was increased to 8 mg. After a further 3 months, her eGFR had fallen to 61 mL/min per 1.73 m2 and her serum albumin was low at 27 g/L. Nephrotic syndrome was diagnosed and a renal biopsy was recommended. This was preempted by an emergency admission for a painful vaso-occlusive crisis (VOC) and an associated acute kidney injury (AKI). Her pain and AKI improved with supportive treatment, but her serum albumin continued to fall to 23 g/L. A renal biopsy was then performed (Figure 1). Light microscopy demonstrated large glomeruli, congested glomerular and peritubular capillaries with sickled red blood cells, and focal segmental glomerular sclerosing lesions; all were consistent with a diagnosis of SCN. In addition, there was mild mesangial hypercellularity, and immunoglobulin A (IgA) deposition was noted on immunofluorescence, confirming a second diagnosis of IgA nephropathy.
Histopathology of renal biopsy. (A) Hematoxylin and eosin stain demonstrating congested peritubular capillaries. (B) Congested glomerulus with segmental sclerosing lesion (black arrow). (C) Large glomerulus with mesangial hypercellularity. (D) Immunofluorescence showing mesangial IgA deposition. Panels A-C were taken on an Olympus BX50 microscope using an Olympus DP12 camera and Olympus image software (Melville, NY). The fluorescent image (panel D) was taken on an Olympus BX51 microscope with an Olympus XC50 camera. Panel A was viewed with a ×10 objective at ×10 magnification (total magnification ×100). Panels B-D were viewed with a ×40 objective at ×10 magnification (total magnification ×400).
Histopathology of renal biopsy. (A) Hematoxylin and eosin stain demonstrating congested peritubular capillaries. (B) Congested glomerulus with segmental sclerosing lesion (black arrow). (C) Large glomerulus with mesangial hypercellularity. (D) Immunofluorescence showing mesangial IgA deposition. Panels A-C were taken on an Olympus BX50 microscope using an Olympus DP12 camera and Olympus image software (Melville, NY). The fluorescent image (panel D) was taken on an Olympus BX51 microscope with an Olympus XC50 camera. Panel A was viewed with a ×10 objective at ×10 magnification (total magnification ×100). Panels B-D were viewed with a ×40 objective at ×10 magnification (total magnification ×400).
Case 2
A 36-year-old man of West African descent with HbSS disease was first seen in the joint sickle/renal clinic in October 2004. He gave a history of frequent VOCs, bilateral avascular necrosis of the hips, previous pulmonary embolism, and leg ulcers that had healed. At that time, he had a uPCR of 919 mg/mmol (8124 mg/g), serum creatinine of 212 µmol/L (2.40 mg/dL), eGFR of 40 mL/min per 1.73 m2, and blood pressure (BP) of 150/80 mm Hg. He was commenced on perindopril and hydroxyurea (HU), and the frequency of his VOC episodes reduced, his BP came under control, his uPCR fell to 50 mg/mmol (442 mg/g), and creatinine fell to a stable 150 to 160 µmol/L (1.70-1.81 mg/dL) with an eGFR of 56 mL/min per 1.73 m2. In early 2010, he expressed a wish to start a family and elected to stop his HU. Within 6 months, he returned to experiencing frequent VOCs, his creatinine increased to 240 µmol/L (2.71 mg/dL, eGFR 33 mL/min per 1.73 m2), uPCR increased to 366 mg/mmol (3235 mg/g), and HU was restarted. He remained well thereafter, until a year later when he again wanted to start a family. HU was stopped and he was commenced on regular exchange blood transfusion (EBT), and he has remained well since. His eGFR has stabilized between 28 and 32 mL/min per 1.73 m2, and in July 2013, his wife gave birth to healthy twins.
Case 3
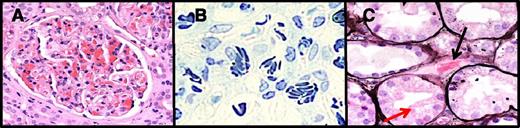
A 29-year-old man of West African descent with HbSS disease received a cadaveric renal transplant from a non–heart-beating donor with a 1-2-0 HLA mismatch in February 2007. Prior to this, he had been dialysis dependent for 8 years for end-stage renal disease (ESRD) secondary to SCN and had required regular blood transfusions, despite high doses of recombinant erythropoietin. On the day of transplantation, he received basiliximab induction therapy and was maintained thereafter with tacrolimus, mycophenolate mofetil, and prednisolone immunosuppression. Postoperatively, his graft did not function for 2 weeks, but on day 14, he started to produce urine. Over the next 18 days, his creatinine fell from 734 µmol/L (8.30 mg/dL) to 90 µmol/L (1.02 mg/dL), and his hemoglobin rose from 6.5 g/dL to 11.0 g/dL. Over the following year, he had several VOCs and sepsis including cytomegalovirus viremia and Pneumocystis carinii pneumonia requiring noninvasive ventilation. During 2007, his creatinine gradually increased to 200 µmol/L (2.26 mg/dL), but 2 renal biopsies demonstrated no evidence of rejection and his immunosuppression regime was reduced. In March 2008, following a further deterioration in eGFR, a third renal biopsy demonstrated severe glomerular congestion with diffuse sickle cell and rouleaux formation in keeping with acute sickle nephropathy (Figure 2). He was started on regular EBT and has remained free of VOCs and has been dialysis independent for the past 6 years.
Acute sickle nephropathy in a renal transplant biopsy specimen. (A) Hematoxylin and eosin stain of congested and large glomerulus. (B) Toluidine blue stain demonstrating sickle-shaped red blood cells and the glomerular capillaries. (C) Silver stain highlighting a congested peritubular capillary (black arrow). Panels A-C were taken on an Olympus BX50 microscope using an Olympus DP12 camera and Olympus image software (Melville, NY). Panels A and C were viewed with a ×40 objective at ×10 magnification (total magnification ×400); panel B was viewed with a ×20 objective ×10 magnification (total magnification ×200).
Acute sickle nephropathy in a renal transplant biopsy specimen. (A) Hematoxylin and eosin stain of congested and large glomerulus. (B) Toluidine blue stain demonstrating sickle-shaped red blood cells and the glomerular capillaries. (C) Silver stain highlighting a congested peritubular capillary (black arrow). Panels A-C were taken on an Olympus BX50 microscope using an Olympus DP12 camera and Olympus image software (Melville, NY). Panels A and C were viewed with a ×40 objective at ×10 magnification (total magnification ×400); panel B was viewed with a ×20 objective ×10 magnification (total magnification ×200).
Natural history, epidemiology, and genetic modifiers
In most cases, SCN develops slowly and insidiously over time, starting in the very young with glomerular hyperfiltration and leading to microalbuminuria in late childhood or early adulthood. The majority of patients do not progress further, but a number will gradually develop unselective proteinuria and slowly progressive CKD leading to decreased renal reserve. These patients are at increased risk of AKI-complicating VOCs or other interim illnesses, events that often precipitate a further decline in their baseline renal function following recovery from the acute episode. ESRD is a relatively rare complication, though its incidence is on the rise. A prospective case-control study from the early 1990s demonstrated that 4.2% of HbSS patients and 2.4% of HbSC patients had advanced renal failure with a median age of onset of 23.1 and 49.9 years, respectively.1 In the follow-up study, the prevalence of chronic renal failure in the HbSS patients increased to 12% in adults, but the mean age of onset had also risen to 37 years.2 Another study demonstrated that 10.5% of deaths in adult patients with SCD were associated with renal impairment.3 In keeping with this trend, in 2008, advanced CKD was reported as present in 24% of SCD patients who had survived to 60 years of age or more and was the cause of death in 45% in those who died above this age.4
Renal dysfunction is relatively more common and more severe in patients with HbSS and HbSβ0 genotypes than in patients with HbSC or HbSβ+ thalassemia.3,5 In our patient cohort, both the incidence and degree of microalbuminuria are much lower in adults with HbSC disease when compared with HbSS or HbSβ0.6 Indeed, all our patients with HbSC disease and eGFR <45 mL/min per 1.73 m2 have a second renal diagnosis to account for their CKD, as in case 1. The other 2 major genetic modifiers are fetal Hb (HbF) levels and α-globin genotype. In keeping with the protective effect of HbF, patients with the Central African Republic βS haplotype who have relatively lower HbF levels are at an increased risk of developing renal dysfunction. In their cohort of 725 HbSS patients, Powars et al observed that no patient with >20% HbF had renal insufficiency.1 Coinheritance of α thalassemia, present in 30% to 35% of SCD patients of African descent, delays the onset of microalbuminuria,6 an effect ascribed to the ensuing reduction in hemolysis and complications related to nitric oxide–depleted vasculopathy.
Genetic variations outside of the hemoglobin genes have also been implicated in the course of the disease. The TGF-β/BMP pathway is a key driving force in the pathogenesis of chronic kidney scarring, and single-nucleotide polymorphisms in genes related to this pathway have been implicated in SCN.7 A recent single study suggested that the MYH9-APOL1 locus, an important genetic risk factor for renal failure in non-SCD populations of African ancestry,8 is also associated with SCN.9
Although genetic modification can explain a large proportion of the variation in phenotype seen in patients with SCD, the environment in which they live must also be influential. Poverty and the prevalence of communicable diseases are obvious confounders, as are the accessibility and resourcefulness of the health care system available within the community. All 3 of our patients were born in West Africa but moved to the United Kingdom in childhood or early adulthood. The incidence of CKD within a cohort of patients increases with advancing age, and so its prevalence is dependent upon the longevity of that cohort and its relative protection from other complications. Given these major environmental differences, it is very difficult to assess more specific gene-environment interactions.
Diagnosing SCN
It is important to remember that the patient population at risk of developing SCN is also at risk of other diseases that affect the kidneys such as lupus nephritis, blood-borne viruses, and various forms of glomerulonephritis. Not only are these diseases managed differently than SCN, but they may also influence the prognosis when they coexist. In case 1, the patient presented with moderate proteinuria and normal renal function, as may be expected for SCN. However, the rapid decline to nephrotic syndrome and progressive renal impairment are both atypical for SCN in a patient with HbSC disease. Although light microscopy of her renal biopsy specimen was compatible with SCN, immunofluorescence revealed a second diagnosis of IgA nephropathy, which is sufficient to explain her nephrotic syndrome but unfortunately worsens her renal prognosis.
Because microalbuminuria (albumin to creatinine ratio >3.5 mg/mmol or 30 mg/g) is so common in adults with SCD (see below), it is our practice to investigate all patients who develop or present with a urinary protein to creatinine ratio of >50 mg/mmol (442 mg/g), persistent microscopic hematuria, declining renal function (>10% fall in eGFR per annum), or an eGFR <60 mL/min per 1.73 m2 in a joint clinic attended by both a hematologist and a nephrologist familiar with the renal complications of SCD. These patients are screened for other causes of CKD (see recommended investigations below), and if any of these investigations are positive or if the patient’s signs and symptoms do not conform to those expected within the natural history of SCN as described above, they are referred on for further renal or urologic investigations. Patients with sudden onset of heavy proteinuria with or without nephrotic syndrome undergo renal biopsy.
The recommended investigations for sickle patients with proteinuria and/or hematuria are as follows:
Immunology for lupus nephritis (autoantibodies, double-stranded DNA antibodies, and complement levels)
Virus serology (HIV, hepatitis B and C, and human parvovirus B19 [if new-onset nephrotic syndrome or recent transient pure red cell aplasia is present])
Myeloma screen (if >40 years old)
Renal tract ultrasound scan or computed tomography and urine cytology (if hematuria is present)
Renal biopsy should be considered if any of 1-3 is positive or if acute nephrotic syndrome is present
Pathobiology of SCN
The pathogenesis of SCN is intimately related to the vascular supply of the kidney. Although the renal cortex receives an ample blood supply, the inner medulla is perfused through a sluggish but intricate circulation. This is critical to maintaining the osmotic gradient that drives water and solute reabsorption, but the resulting hypoxia, acidosis, and hyperosmolarity make the inner medulla an ideal environment for polymerization of deoxygenated hemoglobin S. Over time, repeated cycles of ischemic injury lead to the chronic microvascular disease that is apparent in established SCN. In parallel with this, cortical renal blood flow and glomerular filtration rate (GFR) are increased in response to anemia and vasodilation. The subsequent hyperfiltration eventually results in proteinuria and glomerulosclerosis, which together with tubulointerstitial fibrosis heralds the onset of progressive CKD.10
What are the sickle-related complications? Presentation patterns of SCN
Hyposthenuria
Hyposthenuria (the inability to concentrate urine >450 mOsm/kg under water-deprived conditions) is a universal finding in patients with SCD. In children, this is usually reversible by blood transfusion, but with age, the renal damage becomes irreversible and the hyposthenuria becomes a permanent feature.11 This is often manifest as nocturnal enuresis, a debilitating problem experienced by many children and young adults alike, and also predisposes patients to dehydration when unwell.12
Hyperfiltration
Hyperfiltration is detectable early in childhood as has been demonstrated in babies recruited to the BABY HUG study.13 As children get older, the GFR rises further and can often peak at levels above 200 mL/min per 1.73 m2. This may be partially accounted for by an increased cardiac output driven by anemia, although it is not reversed by regular red cell transfusion.14 Localized prostaglandin release and an increase in nitric oxide synthase in response to hypoxia both result in an increase in total renal blood flow, and inhibition of prostaglandin synthesis with indomethacin has been shown to have a significant negative impact on GFR.15
Proteinuria
The appearance of albumin in the urine (albumin to creatinine ratio repeatedly >3.5 mg/mmol or 30 mg/g) can be detected in 20% of children with SCD (prevalence increasing with age) and marks the onset of SCN.16 In our own cohort of adult patients, microalbuminuria was detectable in 28% of patients in the 16- to 25-year age group, 38% in patients 26 to 35 years, 50% in those 36 to 45 years, and >60% in those 46 years of age or older.6 In a subset of patients, microalbuminuria progresses to unselective proteinuria, occasionally becoming nephrotic in range (>3 g total protein in 24 hr) after many years. Full nephrotic syndrome is uncommon at approximately 4%, but when it does occur, it is associated with a very poor outcome.17 A recognized trigger for nephrotic syndrome, which has been highlighted in patients with SCD, is a recent infection with human parvovirus B19. Early renal biopsy may demonstrate the collapsing variant of focal segmental glomerulosclerosis, the classical lesion associated with virus-induced glomerulopathy.18,19 Although the nephrotic syndrome often spontaneously resolves, the long-term prognosis is poor because many develop rapidly progressing CKD.
Tubular disorders
SCD is associated with both proximal and distal tubular abnormalities. The high GFR in association with the increased loss of salt and water leads to a reactive increase in sodium and water reabsorption by the proximal tubule17 driving the reabsorption of other solutes such as phosphate and β2 microglobulin; hence, many patients have hyperphosphatemia. Other solutes such as creatinine and uric acid have a marked increase in proximal tubular secretion. Up to 30% of the total creatinine excretion can arise from tubular secretion, resulting in an overestimation of GFR when creatinine-base formulas are used.
Distal tubule function is often impaired, leading to reduced potassium and hydrogen ion excretion and an incomplete type IV renal tubular acidosis. Although in steady state this is not normally clinically apparent, unwell patients are often disproportionately acidotic and hyperkalemic.
Hematuria
Hematuria is common in patients with SCD and sickle cell trait. Microinfarcts in the renal papillae can lead to painless but visible hematuria, which is self-limiting. These infarcts can occasionally be large, causing papillary necrosis and painful clot colic. Renal papillary necrosis can be diagnosed by ultrasonography, but computed tomography urography and direct ureterorenoscopy have a much higher diagnostic rate.20,21 Due to its self-limiting nature, the management of hematuria is usually conservative and limited to good hydration, pain relief, and antibiotics if necessary. Although usually benign, hematuria can herald the presence of the rare medullary cell carcinoma and should therefore always be investigated. This tumor is only found in patients with HbS, can occur in children as young as 2, and is highly aggressive.
SCN: when, what, and how to treat
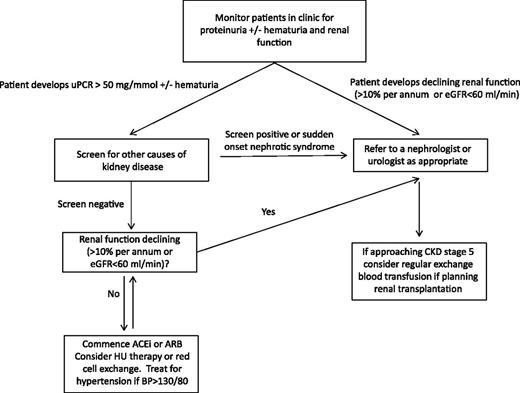
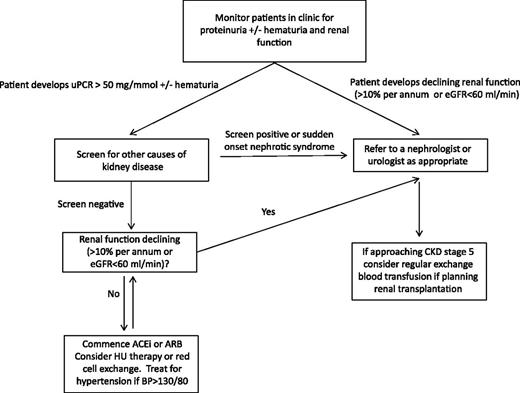
We suggest a practical schema for managing patients with SCN (Figure 3).
Management pathway for renal complications in sickle cell disease. ACE, angiotensin-converting enzyme.
Management pathway for renal complications in sickle cell disease. ACE, angiotensin-converting enzyme.
Monitoring renal function
Serum cystatin C has been demonstrated to be a more accurate surrogate marker of renal function than creatinine in adults and children with SCD and may detect a decline in GFR earlier.22-25 Although promising, it has yet to be fully validated as a marker of renal function against gold-standard measures that calculate true GFR. Until such time, creatinine and creatinine-based equations, which estimate GFR, will continue to be used in patients with SCD. Given the limitations of serum creatinine as a marker of glomerular function in these patients,26 it is the pattern and rate of change of either serum creatinine or eGFR that should be considered rather than the absolute value; in particular, relatively modest changes in creatinine at higher levels of GFR can represent significant decline in renal function. For example, a doubling in creatinine from 40 to 80 µmol/L (0.45-0.90 mg/dL) in a 25-year-old woman is equivalent to a drop in eGFR from 217 to 97 mL/min per 1.73 m2 and is likely to represent a significant deterioration in renal function, even though neither serum creatinine value falls outside the normal range. By monitoring the rate of change of eGRF in this way, we rarely feel it necessary to undertake formal GFR measurements.
Hypertension
Although patients with SCD tend to have a lower systemic BP than age- and ethnic-matched controls, it has been shown that those with high-normal BP values (systolic BP 120-139 mm Hg, diastolic BP 70-89 mm Hg) have higher serum creatinine levels and an increased risk of pulmonary hypertension when compared with SCD patients with lower blood pressures.27,28 Although unproven, it is possible that moderate degrees of hypertension are more damaging from a renal perspective in patients with SCD than without SCD, and it is our practice to treat it aggressively for this reason.
HU
The BABY HUG multicenter study was designed to ascertain whether HU therapy is safe in infants and whether it influences renal function. Although there was no impact on this primary end point, those children treated with HU could achieve higher urine osmolarities and had smaller renal volumes compared with placebo-treated children.29 A follow-up study (HUSTLE) demonstrated that 18 of 23 children treated with HU for a 3-year period had an improvement (ie, reduction) in their GFR. A number of small-scale studies in adults with SCD have shown an association between HU use and a reduction in the presence and/or degree of proteinuria.30 In case 2, HU treatment was associated with a stabilization in renal function that had been previously declining. Although these studies and anecdotal cases do not offer conclusive evidence that HU treatment prevents the progression of SCN to CKD directly, overall, HU should have a beneficial effect through reduction of frequency of VOCs that can precipitate AKI. Circumstantial evidence suggests that HU can limit some of the early symptoms and signs of renal involvement and should be considered in all patients with SCN, unless indicated otherwise.
Inhibitors of the renin angiotensin system
Proteinuria has been known for many years to be associated with rapid progression of CKD, and reducing this proteinuria with inhibitors of the renin angiotensin system (either angiotensin-converting enzyme inhibitors [ACEi] or angiotensin receptor blockers [ARBs]) slows this progression in patients with either diabetic or nondiabetic proteinuric renal disease.31,32 In keeping with this, in 2 studies of patients with SCN, proteinuria and eGFR responded predictably to ACEi.33,34 We recommend commencing ACEi or ARB treatment when the uPCR is >100 mg/mmol (884 mg/g). These drugs must be introduced cautiously, because many patients have a low/normal blood pressure and so moderate doses can cause postural hypotension, which can be partially circumvented by taking the medication at bedtime. Patients have reported that this has the benefit of reducing their nocturnal urinary frequency, presumably as a direct result of a functional drop in GFR. Patients with SCN are prone to hyperkalemia, which can be exacerbated by ACEi and ARB treatment and is often the dose-limiting factor.
Other preventative or early treatment options
Red cell transfusion
A retrospective analysis of 120 children with sickle hemoglobinopathies concluded that chronic transfusion protected against the onset of microalbuminuria when commenced before the age of 9 years.35 Two further studies, however, found that chronic transfusion made no difference to the onset of proteinuria.36,37 Although it seems logical that chronic transfusion could be effective at preventing many of the renal complications of SCD, this therapy is not a minor undertaking, and evidence of its benefits is needed before it can be justified for the treatment or prevention of SCN. However, in those with established and progressive CKD, in whom HU is ineffective, there is anecdotal evidence that regular EBT can slow or halt the progression of CKD, as in case 2 above. For such situations, we maintain HbS levels at <40% to 50%, but this is based on pragmatism rather than evidence.
Hemopoietic stem cell transplantation
Hemopoietic stem cell transplantation (HSCT) is potentially curative but has largely been limited to children with severe complications, and there are no reports in the literature of it being undertaken in children <16 years for treatment of SCN. One study on 22 children demonstrated a 93% survival rate. None developed proteinuria, and the average GFR in those with hyperfiltration normalized, although 2 patients developed significant renal impairment.38 Established SCN has been considered an indication for HSCT in a few adult patients. One 18-year-old woman with early CKD developed rapidly declining renal function post-HSCT and required a cadaveric kidney transplant 2 years later.39 In another series, HSCT did not impact the slope of renal decline in 3 adults with pre-HSCT CKD.40 Before considering HSCT as a treatment of SCN, it is worth remembering that HSCT itself carries a significant risk of long-term renal disease, even in patients without other risk factors.41,42
Management of advanced CKD
Erythropoiesis-stimulating agents
As the GFR falls, the ability of the kidneys to synthesize erythropoietin declines, and so worsening anemia accompanies the rising creatinine. Erythropoiesis-stimulating agents (ESAs) can be useful, particularly in combination with HU in patients who are intolerant of HU alone due to reticulocytopenia. Patients with CKD stage 3-4 (eGFR 15-60 mL/min per 1.73 m2) often require very high doses of ESAs to have an impact on their hemoglobin levels. Due to the increased risk of triggering VOCs, hemoglobin targets should be lower than in the general CKD population (< 10 mg/dL), but they are rarely achieved, and most patients become transfusion dependent by the time they reach ESRD.
Renal replacement therapy
Dialysis
Once the GFR falls below 40 mL/min per 1.73 m2 in patients with SCN, the subsequent rate of decline can be quite rapid, so timely referral to a nephrology service for preparation for renal replacement therapy (RRT) is vital. Patients with SCD often have very poor peripheral venous access, so dialysis needs to be carefully planned. Outcome data for patients with SCD on dialysis are few, but Powars reported that ESRD is associated with a very poor prognosis with a mean time to death of only 4 years.1 Similar findings were reported in patients in Saudi Arabia.43 Those with SCD suffered more infectious complications, lived on average for only 27 months after commencing RRT, and were significantly younger when they died (31 vs 47.8 years) when compared with patients with ESRD of other causes.43 An examination of the US Renal Data System of all patients who commenced RRT between 1992 and 1997 revealed not only that was SCN an independent risk factor for death, worse even than diabetes, but also that patients with SCD were much less likely to receive a kidney transplant.44 More recently, it was reported that although patients with SCD are at high risk of dying within the first year of starting dialysis, the mortality rate in this group was significantly lower in those who received predialysis nephrology care compared with those who did not.45
In our practice, we have success with both hemodialysis and peritoneal dialysis in patients with ESRD secondary to SCN. Hemodialysis offers the advantage of ease of access for blood transfusion, whereas peritoneal dialysis is often preferable for those who have run out of options for permanent venous access. With a combination of predialysis counseling, dialysis access planning, ESA therapy, and regular transfusion, patients can remain alive and well on dialysis for many years (as in case 3).
Renal transplantation
Although there may be many obstacles to kidney transplantation, for those for whom it is suitable, it is the modality that offers the best outcome.10 In the US Renal Data System study, SCN ceased to be an independent risk factor for death after renal transplantation.44 Further, although the post–renal-transplantation survival discrepancy still exists between SCD and non-SCD patients with ESRD, the overall mortality for SCD patients posttransplantation has improved and is now comparable with patients with diabetes.46
Once a patient is listed for renal transplantation, s/he should be started on regular blood transfusion (preferably EBT), which improves their well-being and fitness for surgery while awaiting transplantation. Patients on regular EBT posttransplantation have better graft survival and fewer adverse events, including painful crises and acute sickle nephropathy. This point is illustrated clearly in case 3. Following 2 weeks of delayed graft function, recovery of GFR was accompanied by a rapid rise in hemoglobin leading to frequent VOC, a complication that the patient had not suffered from for more than 10 years and one that is well recognized after renal transplantation.47,48 Commencement of regular EBT posttransplantation in case 3 has not only stabilized his renal function, albeit at a relatively poor level, but also allowed him to remain dialysis independent and relatively free of complications. It has become our policy to commence all patients on regular EBT as soon as they are placed on the transplant waiting list (or a few months prior to living donor transplantation) and to continue this postoperatively for the life of the graft. Although alloimmunization is a risk with this course of treatment, we have not found this to be a significant problem. The most frequent serious complication posttransplantation remains sepsis, and we now avoid the use of anti-thymocyte globulin for the treatment of graft rejection.
Iron chelation therapy
Iron overload is an inevitable consequence of long-term blood transfusion therapy. Although the oral iron chelator deferasirox works extremely well in patients with normal renal function, it is nephrotoxic and not suitable for use in patients with predialysis CKD. Once ESRD has been reached, nephrotoxicity ceases to be of concern, and although this medication is not licensed for use in these patients, we and others have used it with relative safety and success in patients on dialysis.49 However, one must exercise caution in prescribing deferasirox posttransplantation; although the creatinine may return to the normal range, transplanted kidneys offer less renal reserve than normally functioning native kidneys, and the drug should be withdrawn if the serum creatinine begins to rise above baseline. Deferoxamine is an alternative treatment of iron (and aluminum) overload in patients on dialysis. Although much of the iron-bound molecule is normally excreted through the urinary tract, some is also excreted through dialysate and the fecal route, giving this drug some efficacy in ESRD.50 However, it is not well tolerated, and infusions are required on each dialysis session for many months to be effective.51 Since the advent of ESAs and better water-purification techniques, iron and aluminum overload have ceased to be major problems in the majority of patients on dialysis, and so this drug is now rarely used.
Acknowledgments
The authors thank Drs Catherine Horsfield and Patrick O’Donnell, consultant histopathologists at St Thomas Hospital, for help with the histopathology images and Claire Steward for help in preparation of the manuscript.
Authorship
Contribution: C.C.S. and S.L.T. wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Swee Lay Thein, King’s College London School of Medicine, Molecular Haematology, The James Black Centre, 125 Coldharbour Ln, London SE5 9NU, UK; e-mail: sl.thein@kcl.ac.uk.