Abstract
Abstract 1727
Myelofibrosis (MF) is characterized by cytopenias, splenomegaly, and burdensome symptoms that may worsen over time. Ruxolitinib (RUX) has been shown to reduce splenomegaly and improve MF-associated symptoms in 2 phase III studies, including COMFORT-I, a randomized, double-blind, placebo (PBO)-controlled trial, which also showed prolonged survival in favor of RUX.
In this post hoc analysis of COMFORT-I, the efficacy of RUX in patients with varying degrees of splenomegaly and symptom severity at baseline was evaluated to assess the potential effects of earlier versus later intervention in this progressive disease.
COMFORT-I participants randomized to RUX (n=155) or PBO (n=154) had MF with an International Prognostic Scoring System (IPSS) score ≥2 and a platelet count of ≥100 × 109/L. Patients with protocol-defined worsening splenomegaly were permitted to cross over from PBO to RUX. The primary endpoint was the percentage of patients with ≥35% reduction in spleen volume (SV) at week (wk) 24. Change in Total Symptom Score (TSS) was a secondary endpoint. TSS was the sum of 6 symptom scores (night sweats, itching, abdominal discomfort, pain under ribs on left side, early satiety, muscle/bone pain) assessed with the modified MF Symptom Assessment Form (MFSAF) v2.0 on a scale of 0 (“absent”) to 10 (“worst imaginable”).
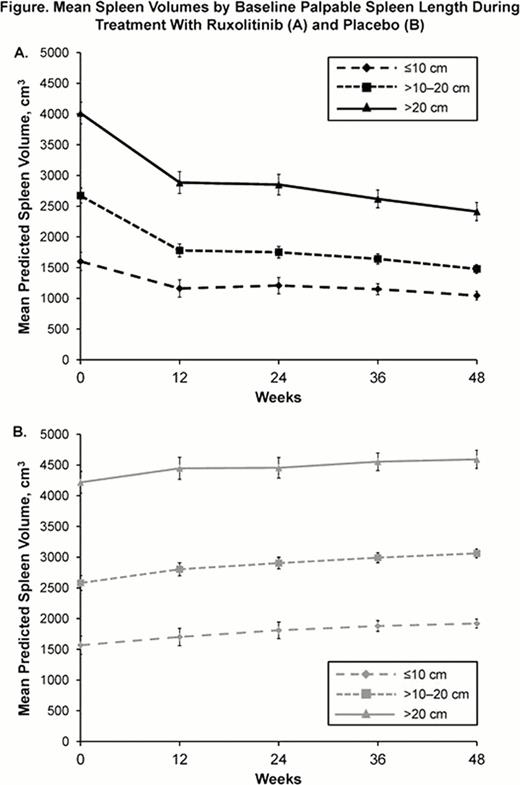
Patients were stratified by palpable spleen length (SL) (≤ 10 cm, <10 to 20 cm, >20 cm) and TSS tertile (≤11.1, >11.1 to 22.0, >22.0) at baseline. SV and TSS stratified by baseline values as described were summarized over time. To account for PBO crossover, modeling was performed to predict SV after crossover using a nonlinear mixed model that best predicted individual patient data. Last observation carried forward was used to impute missing TSS data.
Mean absolute SV and TSS worsened over time in the PBO group regardless of baseline SL and TSS, demonstrating the progressive nature of MF. In patients treated with RUX, mean absolute SV and TSS at wk 24 were lower for patients with smaller SL and less severe TSS at baseline, respectively (Table); absolute differences with PBO were significant within each subgroup. Therefore, patients who initiated RUX therapy with more advanced MF were less likely to achieve the same clinical status experienced by patients initiating therapy with less advanced MF. Notably, even after 24 wks of RUX treatment, SV and TSS reductions in the cohorts with larger SL or greater TSS at baseline did not achieve levels equivalent to baseline of the next lesser baseline severity group (Table; Figure).
Although the severity of splenomegaly and symptoms at baseline influenced the absolute SV and TSS achieved at wk 24, RUX treatment resulted in similar percent reductions in SV and improvements TSS across all subgroups, with the exception of the lower TSS tertile (where there is less room for improvement). In contrast, PBO treatment resulted in increases in SV and worsening of symptoms and patients with less severe SV and TSS at baseline experienced the greatest percent increases in SV and TSS at wk 24.
RUX therapy was associated with SV reduction and symptom improvement regardless of spleen size or symptom severity at baseline, whereas patients on PBO experienced disease progression across all subgroups. Patients receiving RUX with less advanced disease achieved an overall better clinical status, as defined by lower absolute SV and symptom scores. This analysis suggests that initiation of RUX in patients with less severe splenomegaly and symptoms may contribute to improved patient outcomes.
Ruxolitinib Efficacy by Baseline Palpable Spleen Size and Symptom Severity
| SV (cm3) . | ≤10 cm . | >10–20 cm . | >20 cm . | |||
|---|---|---|---|---|---|---|
| RUX . | PBO . | RUX . | PBO . | RUX . | PBO . | |
| n=32 . | n=27 . | n=89 . | n=89 . | n=34 . | n=37 . | |
| Baseline, mean ± SEM | 1602 ± 107 | 1568 ± 148 | 2672 ± 98 | 2580 ± 122 | 4015 ± 224 | 4218 ± 176 |
| Wk 24, mean ± SEM | 1208 ± 93* | 1810 ± 135 | 1751 ± 82‡ | 2903 ± 95 | 2851 ± 207‡ | 4454 ± 167 |
| % change from baseline at Wk 24 ± SEM | –26.1 ± 3.3 | 17.7 ± 4.3 | –34.7 ± 2.0 | 13.3 ± 1.8 | –29.9 ± 2.8 | 7.3 ± 3.0 |
| SV (cm3) . | ≤10 cm . | >10–20 cm . | >20 cm . | |||
|---|---|---|---|---|---|---|
| RUX . | PBO . | RUX . | PBO . | RUX . | PBO . | |
| n=32 . | n=27 . | n=89 . | n=89 . | n=34 . | n=37 . | |
| Baseline, mean ± SEM | 1602 ± 107 | 1568 ± 148 | 2672 ± 98 | 2580 ± 122 | 4015 ± 224 | 4218 ± 176 |
| Wk 24, mean ± SEM | 1208 ± 93* | 1810 ± 135 | 1751 ± 82‡ | 2903 ± 95 | 2851 ± 207‡ | 4454 ± 167 |
| % change from baseline at Wk 24 ± SEM | –26.1 ± 3.3 | 17.7 ± 4.3 | –34.7 ± 2.0 | 13.3 ± 1.8 | –29.9 ± 2.8 | 7.3 ± 3.0 |
| TSS . | Lower . | Middle . | Upper . | |||
|---|---|---|---|---|---|---|
| . | RUX . | PBO . | RUX . | PBO . | RUX . | PBO . |
| . | n=46 . | n=57 . | n=49 . | n=49 . | n=54 . | n=45 . |
| Baseline, mean ± SEM | 5.8 ± 0.6 | 5.6 ± 0.4 | 16.6 ± 0.5 | 16.4 ± 0.5 | 30.2 ± 0.7 | 31.8 ± 1.1 |
| Wk 24, mean ± SEM | 4.3 ± 0.7† | 9.4 ± 0.9 | 8.5 ± 1.2‡ | 21.4 ± 1.5 | 16.2 ± 1.5‡ | 33.4 ± 1.7 |
| % change from baseline at Wk 24 ± SEM | –25.8 ± 10.4 | 98.4 ± 26.2 | –49.6 ± 6.7 | 32.3 ± 10.1 | –45.6 ± 5.2 | 6.1 ± 4.5 |
| TSS . | Lower . | Middle . | Upper . | |||
|---|---|---|---|---|---|---|
| . | RUX . | PBO . | RUX . | PBO . | RUX . | PBO . |
| . | n=46 . | n=57 . | n=49 . | n=49 . | n=54 . | n=45 . |
| Baseline, mean ± SEM | 5.8 ± 0.6 | 5.6 ± 0.4 | 16.6 ± 0.5 | 16.4 ± 0.5 | 30.2 ± 0.7 | 31.8 ± 1.1 |
| Wk 24, mean ± SEM | 4.3 ± 0.7† | 9.4 ± 0.9 | 8.5 ± 1.2‡ | 21.4 ± 1.5 | 16.2 ± 1.5‡ | 33.4 ± 1.7 |
| % change from baseline at Wk 24 ± SEM | –25.8 ± 10.4 | 98.4 ± 26.2 | –49.6 ± 6.7 | 32.3 ± 10.1 | –45.6 ± 5.2 | 6.1 ± 4.5 |
PBO, placebo; RUX, ruxolitinib; SEM, standard error of the mean.
P-value for RUX vs PBO: *<0.05; †<0.01; ‡<0.001.
Mesa:Incyte: Research Funding; Lilly: Research Funding; Sanofi: Research Funding; NS Pharma: Research Funding; YM Bioscience: Research Funding. Gotlib:Incyte: Consultancy. Kantarjian:Incyte: grant support Other. Sun:Incyte: Employment. Verstovsek:Incyte Corporation: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.