Abstract
Various prospective trials have been performed to assess the roles of allogeneic hematopoietic cell transplantation (allo-HCT) and chemotherapy in patients with acute myeloid leukemia (AML) in first complete remission (CR1). However, the results have not always been consistent, and there has been a limited evaluation of quality of life (QOL) in these postremission strategies. We performed a Markov decision analysis that enabled us to compare survival outcomes with a QOL evaluation using a database of 2029 adult AML patients who achieved CR1. The Markov decision model compared 2 strategies: allo-HCT or chemotherapy in CR1. Patients who had intermediate- or unfavorable-risk AML had a longer life expectancy when they received allo-HCT in CR1 than patients treated with chemotherapy alone. Likewise, patients who had a suitable related donor who received allo-HCT in CR1 had a longer life expectancy. The life expectancy was shortened to a greater degree by adjustment for QOL in the allo-HCT group. Nevertheless, QOL-adjusted life expectancies in most of the subgroups remained longer in the allo-HCT group than in the chemotherapy group. Our results showed that older patients with a related donor and younger patients with unfavorable cytogenetics benefited the most from allo-HCT in CR1.
Introduction
Although 60%-80% of patients with acute myeloid leukemia (AML) achieve first hematologic complete remission (CR1) with chemotherapy, a substantial number of patients have an individualized risk of relapse.1 Allogeneic hematopoietic cell transplantation (allo-HCT) has been established as a powerful treatment method to reduce the risk of relapse in patients with AML. However, this approach still leaves concerns associated with a certain probability of nonrelapse mortality. Although several prospective trials that used genetic allocation have been performed to clarify the roles of postremission strategies, the results have not always been consistent.2-9 The role of allo-HCT in patients with AML in certain subgroups, including patients with intermediate-risk AML and elderly patients who have remained in CR1, remains unclear. A large meta-analysis that considered many of these prospective studies reported that allo-HCT in CR1 provided survival advantages not only in an unfavorable-risk group but also in an intermediate-risk group.10 Even with these numerous studies performed in a prospective setting, it is still controversial to simply define allo-HCT as a better decision because of concerns about various late effects such as graft-versus-host disease (GVHD) that might lower the quality of life (QOL) after cure of the disease.
A decision analysis is a statistical technique that is used to help decision making under uncertain conditions with the assumption of a QOL evaluation.11 When it is combined with a Markov process, it gives a flexible analytical method that makes it possible to track clinical events that occur after a certain decision with different probabilities and desirability over time.12 This technique can offer valuable information about what clinical decision should be taken by quantitatively integrating the risks and benefits of a certain decision, and, hence, has been widely applied in making decisions in various fields. For example, in the field of hematology, on the basis of the results of a Markov decision analysis, Lee et al13 reported the indications of allo-HCT for chronic myeloid leukemia in the era before imatinib, and Cutler et al14 elucidated the recommended timing of allo-HCT for younger patients with myelodysplastic syndrome. Regarding AML, Sung et al15 reported the results of a decision analysis with a conventional decision tree concerning consolidation strategies for patients in CR1. However, a Markov decision analysis has not yet been reported for postremission strategies in AML in CR1. To address this point, we performed a Markov decision analysis with the use of clinical information collected from 2029 patients.
Methods
Data source
The study protocol was approved by the Institutional Review Board at National Cancer Center Hospital. We constructed a new database that included the clinical data of adult patients (age 16-70 years) whose conditions were diagnosed as AML by the World Health Organization classification between 1999 and 2006 and who had achieved CR1 after 1 or 2 courses of induction chemotherapy. Clinical information on > 2600 patients was collected from 70 institutions across the country. Patients with biphenotypic leukemia who were treated with chemotherapy for acute lymphocytic leukemia; patients who had extramedullar AML without marrow invasion, an extramedullary lesion that did not totally disappear after remission induction chemotherapy, or acute promyelocytic leukemia; and patients who received autologous HCT in CR1 were excluded from the analysis. Consequently, a total of 2029 patients were considered for this analysis.
Decision strategy
The primary decision examined in this study was whether to perform allo-HCT in patients with AML who remained in CR1. Statistical analyses were performed as of January 2010 with the use of the software package TreeAge Pro 2009 (TreeAge Software Inc) and the SPSS software package (SPSS Inc).
Markov model.
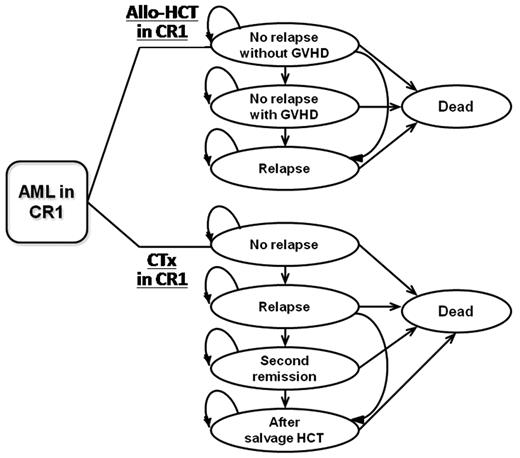
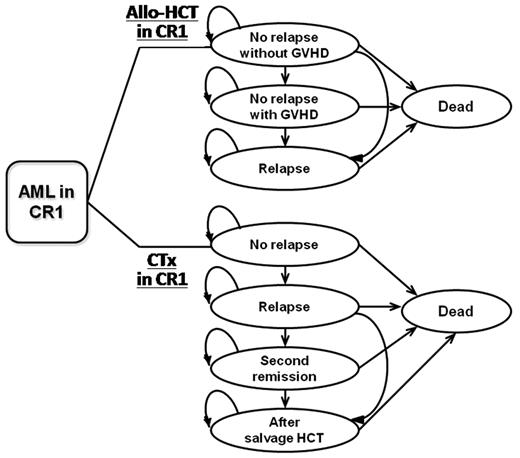
We constructed a Markov decision model to compare 2 strategies: performing allo-HCT in CR1 (HCT group) and continuing chemotherapy without allo-HCT in CR1 (CTx group; Figure 1). The possible health states that were considered to occur after each decision/strategy included, for the HCT group, (1) no relapse without GVHD, (2) no relapse with GVHD, (3) relapse, and (4) dead, and for the CTx group, (1) no relapse, (2) relapse, (3) second remission, (4) after salvage allo-HCT, and (5) dead. The “GVHD” state included chronic extensive GVHD. The “dead” state included death from any cause. A schematic of the tree file is shown in supplemental Figure 1, available on the Blood Web site; see the Supplemental Materials link at the top of the online article.
Markov decision model. Markov model that compares allo-HCT in CR1 and chemotherapy in CR1 is shown. Possible health states for each of the 2 groups are indicated in circles. Arrows indicate possible transitions between states. CR1 indicates first complete remission; allo-HCT, allogeneic hematopoietic cell transplantation; CTx, chemotherapy; and GVHD, graft-versus-host disease.
Markov decision model. Markov model that compares allo-HCT in CR1 and chemotherapy in CR1 is shown. Possible health states for each of the 2 groups are indicated in circles. Arrows indicate possible transitions between states. CR1 indicates first complete remission; allo-HCT, allogeneic hematopoietic cell transplantation; CTx, chemotherapy; and GVHD, graft-versus-host disease.
State transition probabilities.
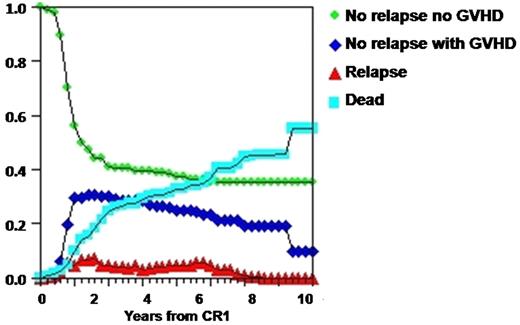
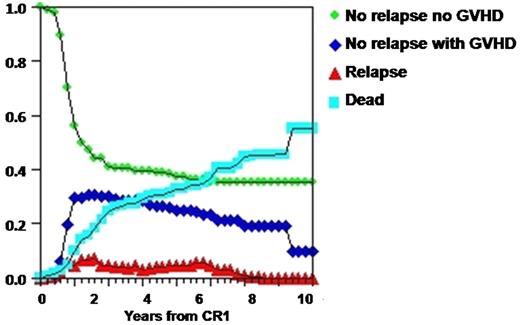
Transition probabilities between the states were calculated from the information in the database collected for this analysis as described in “Data source.” The probabilities of state transition were allowed to vary over time. As a result, patients were distributed in various health states with different proportions along with cycle advances, that is, as time advanced from CR1, as shown in Figure 2. To take into account patients who were unable to receive allo-HCT in CR1 even though they had made a decision to receive allo-HCT, patients who died or relapsed within 3 months from CR1 were excluded from the database when we calculated the probabilities. The cycle length between state transitions has previously been set at the time considered to represent the clinical features and decision-making process for the target disease. In a Markov decision analysis that targeted myelodysplastic syndrome,14 the cycle length was set at 6 months. In this analysis that targets patients with AML, we chose a shorter cycle length (3 months), and the analysis was performed for 40 cycles (10 years). The results are presented as life expectancy (LE), which is the average duration of life when patients are followed up for 10 years.
Distribution of patients in each health state. Distribution of patients with intermediate-risk AML in each health state is shown. Transition probabilities between the states were calculated for each subgroup with the use of the database. The probabilities of state transition were allowed to vary along with the cycle (1 cycle = 3 months) advances, depending on the states that the cohorts move from and to. As a result, the patients were distributed in each health state in changing proportions at different times from CR1. GVHD indicates graft-versus-host disease; and CR1, first complete remission.
Distribution of patients in each health state. Distribution of patients with intermediate-risk AML in each health state is shown. Transition probabilities between the states were calculated for each subgroup with the use of the database. The probabilities of state transition were allowed to vary along with the cycle (1 cycle = 3 months) advances, depending on the states that the cohorts move from and to. As a result, the patients were distributed in each health state in changing proportions at different times from CR1. GVHD indicates graft-versus-host disease; and CR1, first complete remission.
QOL utilities.
We also assessed QOL-adjusted life expectancy (QALE) for the HCT and CTx groups. The time spent in each health state was adjusted for the estimated QOL that patients experienced while they remained in that state, which was represented by a utility value. In this study, utility values were derived from a questionnaire (supplemental Figure 2) that used a visual analog scale and was presented to 35 physicians who were familiar with the treatment of AML. Among them, 25 were physicians who were mainly involved in transplantation, and 10 were physicians mostly involved in chemotherapy with knowledge of transplantation. The utility values were expressed as numerical values between 0 (a health state equivalent to dead) and 1 (perfect health) (Table 1) and were used to adjust for QOL by being multiplied by the expected length of life for each state in each cycle. For long-term survivors who developed chronic extensive GVHD, the utility value was changed on the basis of the previously reported probability of the discontinuation of immunosuppressive treatment.16,17
Comparison of HCT with CTx in CR1 and sensitivity analyses.
Both LE and QALE were analyzed for the HCT group and the CTx group. LE and QALE, which represent the average expected duration of life in 10-year follow-up from CR1, were obtained from the area under the survival curves depicted by TreeAge Pro software. An annual discount rate of 3% was used for all analyses. Subgroup analyses were performed on the basis of patient age, the Southwest Oncology Group (SWOG) cytogenetic classification,2 and donor availability. We performed sensitivity analyses to test the robustness of our conclusions. Variable measures that were tested in the sensitivity analysis included the range of patients who were excluded from the database on the assumption that they were unable to receive the decided treatment, the plausible range of QOL utilities, 95% confidence intervals of the state transition probabilities, and the age range of subgroups.
Results
Patients
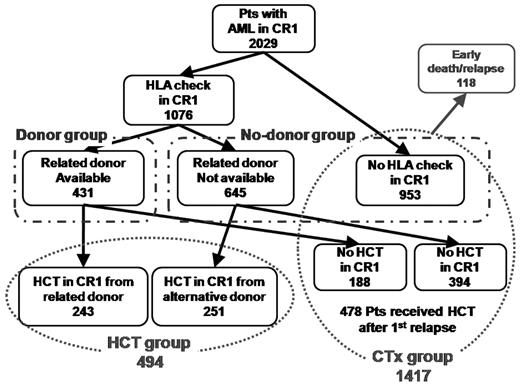
A total of 2029 patients were eligible for this analysis (Table 2). The median age was 50 years, and the median follow-up of the surviving patients was 49.8 months (range, 0.2-116.3 months). The proportions of patients with favorable, intermediate, unfavorable, and unknown cytogenetic risk according to the SWOG criteria were 19%, 52%, 18%, and 11%, respectively. Therapies performed at CR1 were allo-HCT in 494 patients (24%) and chemotherapy in 1535 patients (76%). The HCT group included all the 494 patients who received allo-HCT in CR1. The median interval from CR1 to allo-HCT was 4.7 months (range, 0-37 months). Among patients who were treated with chemotherapy in CR1, 118 patients who died or relapsed within 3 months were excluded when calculating state transition probabilities on the assumption that they might have decided to receive allo-HCT while they remained in CR1. As a consequence, 1417 patients, including 478 who received allo-HCT after their first relapse, were included in the CTx group (Figure 3). The patients in the HCT group were younger and were more often associated with unfavorable features compared with those in the CTx group. Table 3 and Figure 3 show donor availability and actual application of allo-HCT in CR1. Among 1076 patients for whom human leukocyte antigen (HLA) was typed in CR1, 431 had HLA-matched or 1-antigen (Ag)–mismatched related donors (40%). Donor group included the 431 patients who had a suitable related donor. Among them, 243 actually received allo-HCT in CR1 (related donor, 240; unrelated donor, 3). The no-donor group included the 645 patients who did not find a related donor and 953 for whom HLA was not typed in CR1. Among them, 251 received allo-HCT in CR1 from an alternative donor (unrelated bone marrow, 177; unrelated cord blood, 62; haploidentical related donor, 12). In both the donor and no-donor groups, subgroup analyses were separately performed by comparing patients who received allo-HCT in CR1 (HCT group) and patients who did not (CTx group). Overall survival curves obtained by a Kaplan-Meier estimation of all of the patients registered in our original database stratified according to the SWOG classification and the treatment chosen in CR1 are shown in supplemental Figure 3. Survival curves depicted by TreeAge Pro are shown in supplemental Figure 4.
Patient flow. The flow of HLA check, donor availability, and actual application of allo-HCT in CR1 are shown. Among the total of 2029 patients with AML in CR1, 494 received allo-HCT in CR1 and were included in the HCT group. Among the remaining 1535 patients, 118 patients who died or relapsed within 3 months were excluded to take into account patients who were unable to receive allo-HCT in CR1 even though they had made a decision to receive HCT in CR1. Consequently, 1417 patients were included in the CTx group. Among them, 478 received allo-HCT after first relapse. The donor group included the 431 patients who had a suitable related donor. The no-donor group included the 645 patients who did not find a related donor and 953 for whom HLA was not typed in CR1. CR1 indicates first complete remission; and HCT, hematopoietic cell transplantation.
Patient flow. The flow of HLA check, donor availability, and actual application of allo-HCT in CR1 are shown. Among the total of 2029 patients with AML in CR1, 494 received allo-HCT in CR1 and were included in the HCT group. Among the remaining 1535 patients, 118 patients who died or relapsed within 3 months were excluded to take into account patients who were unable to receive allo-HCT in CR1 even though they had made a decision to receive HCT in CR1. Consequently, 1417 patients were included in the CTx group. Among them, 478 received allo-HCT after first relapse. The donor group included the 431 patients who had a suitable related donor. The no-donor group included the 645 patients who did not find a related donor and 953 for whom HLA was not typed in CR1. CR1 indicates first complete remission; and HCT, hematopoietic cell transplantation.
Markov decision analysis
The discounted LE and QALE for the HCT and CTx groups were analyzed for patients of all ages, younger patients (16-49 years) and older patients (50-70 years; Table 4). In each age group, LE and QALE were analyzed in different cytogenetic subgroups and donor-availability subgroups.
Analysis of all patients.
An analysis that included patients of all ages showed that LE in the HCT group was 3 months longer than that in the CTx group (69.7 vs 66.7 months; Table 4). After we adjusted for QOL, QALE in the HCT group was only 0.5 months longer than that in the CTx group (55.9 vs 55.4 months). The LE was generally shortened to a greater degree in the HCT group after adjustment for QOL. This trend was consistent throughout all of the subgroups.
We performed subset analyses according to cytogenetic risk stratified according to the SWOG criteria. Patients with favorable-risk AML in the CTx group had a longer LE than patients in the HCT group. In contrast, patients with intermediate, unfavorable, and unknown-risk AML in the HCT group had a longer LE than patients in the CTx group (intermediate, 73.6 vs 66.4 months; unfavorable, 61.6 vs 53.4 months). Although QALE was shortened to a greater degree in the HCT group, we found that QALE remained longer in the HCT group for all cytogenetic risks except for the favorable-risk group (favorable, 56.0 vs 64.3 months; intermediate, 59.4 vs 55.6 months; unfavorable, 47.6 vs 44.4 months). In the analysis of AML other than favorable risk, patients in the HCT group had a longer LE and a longer QALE than patients in the CTx group (LE, 69.5 vs 62.5 months; QALE, 55.8 vs 52.0 months).
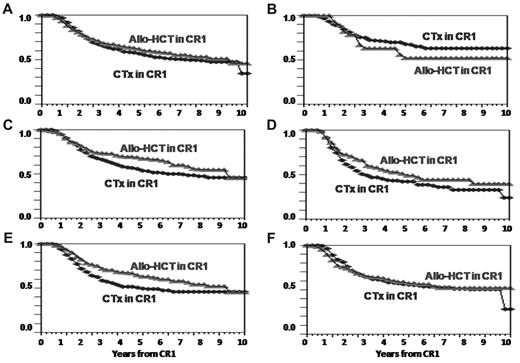
We also performed subset analyses on the basis of the availability of a related donor. Patients who were known to have an HLA-matched or 1-Ag– mismatched related donor (donor group) in the HCT group had a longer LE and a longer QALE than patients in the CTx group (LE, 72.2 vs 63.0 months; QALE, 57.6 vs 49.9 months). However, in patients who did not have a suitable related donor (no-donor group), there were no differences in LE or QALE between the HCT and CTx groups (LE, 67.7 vs 67.0 months; QALE, 54.6 vs 54.4 months). Analyses of the donor and no-donor groups were also conducted with the database whereby the favorable-risk patients were excluded. There was almost no change in LE and QALE in the HCT group (less than a month) compared with the results obtained with the whole database. However, LE and QALE in the CTx group were shortened by several months by excluding the patients with favorable-risk AML from analysis. Consequently, in the donor group, the differences of LE and QALE between the HCT and CTx group increased (LE, 72.0 vs 60.5 months; QALE, 57.2 vs 47.6 months). Meanwhile in the no-donor group, LE and QALE in the HCT group became longer than those in the CTx group (LE, 67.3 vs 64.2 months; QALE, 54.5 vs 52.2 months). Survival curves that compare the HCT and CTx groups in these subgroups depicted by TreeAge Pro software are shown in Figure 4.
Survival curves of allo-HCT versus CTx by TreeAge. The overall survival curves of the HCT and CTx groups depicted by TreeAge Pro 2009 in (A) total patients, (B) SWOG favorable-risk group, (C) intermediate-risk group, (D) unfavorable-risk group, (E) donor group, and (F) no-donor group. allo-HCT indicates allogeneic hematopoietic cell transplantation; CTx, chemotherapy; and CR1, first complete remission.
Survival curves of allo-HCT versus CTx by TreeAge. The overall survival curves of the HCT and CTx groups depicted by TreeAge Pro 2009 in (A) total patients, (B) SWOG favorable-risk group, (C) intermediate-risk group, (D) unfavorable-risk group, (E) donor group, and (F) no-donor group. allo-HCT indicates allogeneic hematopoietic cell transplantation; CTx, chemotherapy; and CR1, first complete remission.
Analysis of younger patients.
For younger patients, LE and QALE were analyzed with the data from patients aged 16-49 years (median 35 years). In the HCT group, LE in younger patients was 6 months longer than that in older patients (71.4 vs 65.8 months). In the CTx group, LE in younger patients was longer than that in older patients by more than a year (73.2 vs 60.0 months).
Younger patients with favorable-risk AML had both a longer LE and a longer QALE in the CTx group than in the HCT group. Allo-HCT in CR1 among younger patients was associated with a longer LE in both the unfavorable-risk group (62.8 vs 55.3 months) and donor group (73.0 vs 67.6 months). After we adjusted for QOL, these patients in the HCT group had a longer QALE than those in the CTx group (unfavorable, 48.7 vs 44.8 months; donor group, 58.3 vs 54.2 months). Younger patients with intermediate-risk AML in the HCT group had a slightly longer LE than those in the CTx group (76.2 vs 75.1 months). However, QALE did not improve when they received allo-HCT in CR1 (62.0 vs 62.4 months).
Analysis of older patients.
The outcomes for older patients were analyzed with the data from patients aged 50-70 years (median, 60 years). Older patients who received allo-HCT in CR1 had a longer LE than patients who received chemotherapy in all subgroups, except for the no-donor group (intermediate, 68.5 vs 60.7 months; unfavorable, 61.6 vs 53.3 months; donor group, 73.4 vs 53.2 months). The data available for favorable-risk patients who received allo-HCT in CR1 were insufficient to perform an analysis. Because of the large decrease in LE in the CTx group among older patients, differences in LE between the HCT and CTx groups became more prominent in older patients than in younger patients. Although the difference in the duration of life between the HCT and CTx groups decreased after we adjusted for QOL, we found that older patients in the HCT group had a longer QALE in the intermediate- and unfavorable-risk groups. The difference in QALE between the HCT and CTx groups was most prominent among older patients who had a suitable related donor (donor group, 57.7 vs 40.4 months).
Sensitivity analysis and external validation.
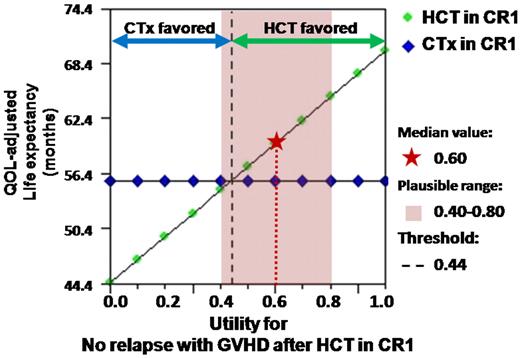
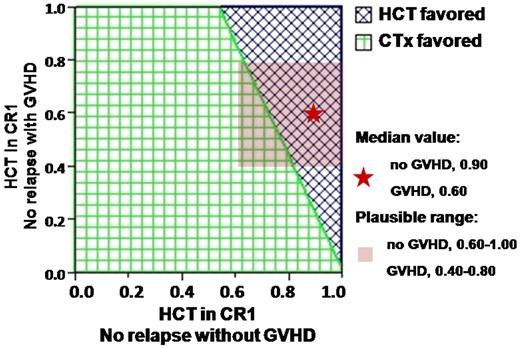
Sensitivity analyses were performed for the assumption of “patients who were unable to receive allo-HCT in CR1 despite the decision to perform allo-HCT,” the plausible range of QOL utilities (Figures 5–6; supplemental Figure 5), 95% confidence intervals of the state transition probabilities, and the age range. We found that the optimal decisions could be altered in both directions, allo-HCT favored versus CTx favored, by changing the population that was excluded from the database, changing the utility values within the plausible range of physicians' opinions, changing the state transition probabilities within the range of the confidence interval, and changing the cutoff point for the age at which the age subgroups were divided. We also compared the overall survival curves depicted by TreeAge Pro software with the use of our database with those obtained by a Kaplan-Meier estimation as reported in prospective studies from other countries.2,6 The curves had similar shapes (supplemental Figure 4).
One-way sensitivity analysis. One-way sensitivity analysis for the utility of the state “No relapse with GVHD” after allogeneic transplantation in CR1 among patients with intermediate-risk AML is shown. The green dot represents the QOL-adjusted life expectancy when allo-HCT was performed in CR1. The blue dot represents the QOL-adjusted life expectancy when treated with chemotherapy in CR1. The median value of the utility for this state provided by physicians was 0.60, shown as a red star. At the median value, QOL-adjusted life expectancy in the HCT group is shown to outweigh that in the CTx group. The threshold value at which the favored decision is altered was 0.44, shown as a black dotted line. The plausible range of the utility provided by physicians was 0.40-0.80, shown as a red transparent square. Because the threshold value, 0.44, was included within the plausible range, this sensitivity analysis indicates that this result favoring HCT may be altered, depending on how the QOL of chronic GVHD is evaluated. Such results that favored a decision may change within the plausible range are interpreted as “sensitive.” If the plausible range was provided in 0.50-0.80, this result would turn to “not sensitive,” indicating that the favored decision does not change. QOL indicates quality of life; CR1, first complete remission; HCT, allogeneic hematopoietic cell transplantation; CTx, chemotherapy; and GVHD, graft-versus-host disease.
One-way sensitivity analysis. One-way sensitivity analysis for the utility of the state “No relapse with GVHD” after allogeneic transplantation in CR1 among patients with intermediate-risk AML is shown. The green dot represents the QOL-adjusted life expectancy when allo-HCT was performed in CR1. The blue dot represents the QOL-adjusted life expectancy when treated with chemotherapy in CR1. The median value of the utility for this state provided by physicians was 0.60, shown as a red star. At the median value, QOL-adjusted life expectancy in the HCT group is shown to outweigh that in the CTx group. The threshold value at which the favored decision is altered was 0.44, shown as a black dotted line. The plausible range of the utility provided by physicians was 0.40-0.80, shown as a red transparent square. Because the threshold value, 0.44, was included within the plausible range, this sensitivity analysis indicates that this result favoring HCT may be altered, depending on how the QOL of chronic GVHD is evaluated. Such results that favored a decision may change within the plausible range are interpreted as “sensitive.” If the plausible range was provided in 0.50-0.80, this result would turn to “not sensitive,” indicating that the favored decision does not change. QOL indicates quality of life; CR1, first complete remission; HCT, allogeneic hematopoietic cell transplantation; CTx, chemotherapy; and GVHD, graft-versus-host disease.
Two-way sensitivity analysis. Two-way sensitivity analysis for the utilities of the states “No relapse without GVHD” and “No relapse with GVHD.” The blue area represents the range in which HCT is favored. The green area represents the range in which CTx is favored. Although the median value (0.90 for “without GVHD” and 0.60 for “with GVHD,” shown as a red star) indicates that HCT in CR1 is favored, the plausible range (0.60-1.00 for “without GVHD” and 0.40-0.80 for “with GVHD,” shown as a red transparent square) overlaps the threshold line. This result is interpreted as “sensitive,” which means the outcome is changeable within the plausible range of QOL evaluation provided by physicians. CR1 indicates first complete remission; HCT, allogeneic hematopoietic stem cell transplantation; CTx, chemotherapy; and GVHD, graft-versus-host disease.
Two-way sensitivity analysis. Two-way sensitivity analysis for the utilities of the states “No relapse without GVHD” and “No relapse with GVHD.” The blue area represents the range in which HCT is favored. The green area represents the range in which CTx is favored. Although the median value (0.90 for “without GVHD” and 0.60 for “with GVHD,” shown as a red star) indicates that HCT in CR1 is favored, the plausible range (0.60-1.00 for “without GVHD” and 0.40-0.80 for “with GVHD,” shown as a red transparent square) overlaps the threshold line. This result is interpreted as “sensitive,” which means the outcome is changeable within the plausible range of QOL evaluation provided by physicians. CR1 indicates first complete remission; HCT, allogeneic hematopoietic stem cell transplantation; CTx, chemotherapy; and GVHD, graft-versus-host disease.
Discussion
We performed a decision analysis that applied a Markov process to evaluate 2 postremission strategies: allo-HCT and CTx in AML in CR1. Our results showed that the LE of patients with intermediate- and unfavorable-risk AML were longer when they received allo-HCT in CR1. We also found that patients who were known to have a suitable related donor had a longer LE in the HCT group. After adjustment for QOL, QALE in most of these subgroups remained longer in patients who received allo-HCT in CR1 than in patients who received chemotherapy.
In subset analyses according to the cytogenetic risk, we showed that favorable-risk patients had a longer LE and a longer QALE in the CTx group, which is consistent with previous reports. However, the results in favorable-risk patients may not be reliable because only a few patients with favorable-risk AML received allo-HCT in CR1 and patients in the HCT group may have had specific reasons (eg, 2 courses of remission induction chemotherapy or antecedent hematologic dysplasia).
In intermediate-risk and unfavorable-risk patients, LE was longer in the HCT group. This result was consistent with that of a large meta-analysis.10 If we integrate the assumption about the QOL obtained after the 2 strategies using utility values provided by physicians, the LE was shortened to a greater degree in the HCT group. This observation may indicate that there are more concerns about the deterioration of the QOL after allo-HCT than after chemotherapy alone. However, we still found that the QALE was longer in the HCT group, except for younger intermediate-risk patients.
In subset analyses that were based on donor availability, we found that patients who had an HLA-matched or 1-Ag–mismatched related donor had a longer LE and a longer QALE when allo-HCT was performed during CR1. A purposeful delay of allo-HCT has not been fully studied in patients with AML when they have a suitable related donor.6 This result may recommend that we consider allo-HCT in CR1 rather than wait until after relapse when a suitable related donor is available. LE in older patients who received allo-HCT from a suitable related donor was even comparable to that in younger patients (73.0 vs 73.4 months), which led to a more conspicuous superiority of allo-HCT compared with CTx when older patients had a suitable related donor. In addition, the QALE of older patients with a related donor was 17 months longer in the HCT group than in the CTx group. This result suggests that allo-HCT in CR1 from a suitable related donor for older patients may provide an improved outcome even after we take into account transplantation-related toxicities, which are generally a greater concern among older patients.18 However, among patients who did not have a suitable related donor, we did not find any advantages of allo-HCT from an alternative donor in CR1 compared with the CTx group. In recent years, the outcomes of allo-HCT from a matched related donor and that from a matched unrelated donor have been reported to be comparable.19 Because this database included the clinical information of patients treated between 1999 and 2006, most of the unrelated bone marrow (BM) donor sources were selected on the basis of HLA serum matches and not on allele matches. In addition, our database included 1-Ag–mismatched unrelated BM and unrelated cord blood as alternative donors. Regarding the indications for allo-HCT from an alternative donor, further studies may be needed to evaluate whether there is a population that benefits from allo-HCT from well-matched unrelated BM.
The ability to consider QOL is one of the advantages of performing a decision analysis. We adjusted for QOL by applying QOL utility values provided by physicians. Utility values for various health states were obtained over a wide range. This observation may indicate that, even for the same patient, different therapeutic strategies may be chosen at the discretion of the physician. Another reason why the range of utility was broad may be the diverse symptoms and QOL within the same health state, such as the severity of “extensive chronic GVHD.”20,21 Consequently, in our study, sensitivity analyses showed that a better decision with a higher QALE was frequently altered to the other decision within the plausible range of utility values provided by physicians. There were no significant difference between the values provided by transplantation physicians and chemotherapy physicians. However, interestingly, median values of QOL utility in our study were lower than those used in prior analyses performed in North America. For example, although the utility for “no relapse with GVHD” was set at 0.6 (range, 0.4-0.8) in our study, this value was set at around 0.9 in other studies.13-15,22 This trend was more prominent in the HCT group, which might indicate differences in approaches to estimating the same complications that may be due to ethnicity or differences in the contents of questionnaires.
It might be ideal to evaluate QALE based on QOL utility values obtained from patients who actually live with various disease states.23,24 However, most prior studies on decision analysis in this field have used utility values provided by physicians.13-15 Sung et al15 stated that their utility values provided by physicians were consistent with those provided by patients in the European Organization for Research and Treatment of Cancer and Gruppo Italiano Malattie Ematologiche dell' Adulto trial.24 Patients may even give diverse QOL values for a certain health state according to differences in age, background, and philosophy. We believe that a QOL validation by patients is an important issue and is worth being pursued in another study.
Our data surely reflect the nature of a retrospectively collected database, including a diverse heterogeneity in treatment strategies chosen after the achievement of CR1. However, it may be difficult to obtain a database that was collected purely prospectively, especially in patients who were treated with chemotherapy alone. Therefore, we considered that this database, which consists of the clinical information for 2029 patients, was sufficient for us to perform this analysis. Another concern is that, because we collected clinical data on Japanese patients, the application of these results to other ethnic populations needs to be carefully evaluated. However, we have shown that the survival curves obtained from this analysis are similar to those reported in prospective studies from other countries. In decision analysis, the P value is not used to show the “significantly” better decision. Sensitivity analysis is a way to investigate the robustness of our conclusions when various parameters are changed within a possible range. It might be difficult to draw a definite conclusion in this study because, as a result of the sensitivity analysis, a favorable decision could be switched to the other decision. Nevertheless, we have been able to show that a decision analysis with a Markov model can be effectively used to evaluate the QOL-adjusted survival outcomes of allo-HCT versus chemotherapy in CR1.
In summary, by using a Markov decision analysis that was based on an original database collected for this study, we have shown that patients with intermediate- and unfavorable-risk AML and patients who had a suitable related donor had a longer LE and a longer QALE when they received allo-HCT in CR1. A subgroup analysis showed that older patients with a suitable related donor benefited the most from allo-HCT in CR1. Although it is clear that both methods of treatment still require improvement, we believe that this observation serves as an important guide for considering the indications for allo-HCT in AML in CR1 by incorporating the evaluation of QOL. Adjustment for QOL with the use of utility values provided by patients who live with the disease should add valuable clues for weighing the value of a postremission strategy for each person. In addition, an investigation that applies a prospectively collected database for a multiethnic population should help to further show the roles of allo-HCT and chemotherapy in AML in CR1.
An Inside Blood analysis of this article appears at the front of this issue.
The online version of this article contains a data supplement.
Presented at the 51st annual meeting of the American Society of Hematology in New Orleans, LA, December 6, 2009.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Dr Corey Cutler and Dr John Koreth for helpful discussion.
This work was supported by grants from the Japanese Ministry of Health, Labor and Welfare and the Advanced Clinical Research Organization.
Authorship
Contribution: S.K. designed the study, prepared the data file, performed the analysis, interpreted data, and wrote the manuscript; T. Yamaguchi was primarily responsible for the study design, data analysis, and interpretation of the data; S.M., N.U., H.K., K.U., T. Yamashita, M.W., K.Y., S.Y., Y. Nawa, J. Taguchi, J. Takeuchi, J. Tomiyama, and Y. Nakamura obtained the patients' data and interpreted data; I.M. reviewed the cytogenetic reports and interpreted data; Y.K. helped to design the study and to interpret data; Y.T. interpreted data and helped to write the paper; and T.F. was primarily responsible for the entire paper as an accurate and verifiable report.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Takahiro Fukuda, Stem Cell Transplantation Division, National Cancer Center Hospital, 5-1-1 Tsukiji, Chuo-ku, Tokyo, 104-0045, Japan; e-mail: tafukuda@ncc.go.jp.