Abstract
Background: AL amyloidosis is generally caused by a kappa or lambda light-chain producing plasma cell clone in the bone marrow. High-dose melphalan (HDM) followed by autologous stem cell transplantation (ASCT) is effective in AL amyloidosis. Pretreatment of these patients with vincristine, doxorubicin and dexamethasone (VAD) may have a rapid and additive effect on the underlying plasma cell clone.
Objective: To study the feasibility and efficacy of VAD followed by HDM and ASCT in AL amyloidosis.
Patients and Methods: In a prospective multicenter phase II study, the Dutch-Belgian Hemato-Oncology Cooperative Group (HOVON) studied the effect of three courses of VAD followed by HDM with ASCT on hematological and clinical response rates and overall survival in AL amyloidosis. Untreated patients aged ≤ 65 years with proven AL amyloidosis and monoclonal gammopathy or multiple myeloma stage I were included. Patients with recent prior malignancy, other types of amyloidosis, and severe other diseases not related to AL amyloidosis were excluded. High risk was defined as cardiac septum ≥ 15 mm, cardiac ejection fraction ≤ 55%, creatinine > 177 μmol/L, or bilirubin > 34 μmol/L (
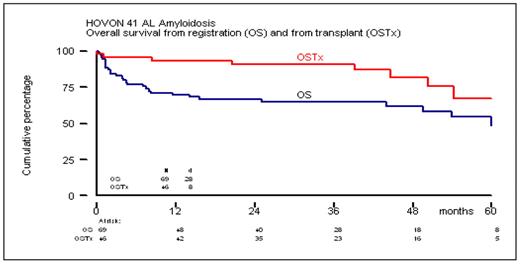
Results: Sixty-nine newly diagnosed patients with AL amyloidosis were included between September 2000 and January 2006: 37 men and 32 women with a median age of 55 years and WHO performance status 0–2. Organ involvement was renal in 58 (84%), cardiac in 32 (46%), hepatic in 12 (17%), and neuropathic in 18 (26%); 15 patients (22%) had involvement of 3 or 4 organs. Thirty-seven (54%) could be classified as high-risk patients. Forty-six patients (67%) could proceed to HDM (140–200 mg/m2) after VAD induction. The transplants were performed in tertiary referral centres. Median haematological recovery time of ANC > 1.0 × 109/L and platelets > 50 × 109/L was 17 and 21 days, respectively. End of survey was November 2007. Overall hematological response was 39% including 16% with a complete response. Overall clinical response was 26% and stabilization in 35%. In 43% of patients only the clinical response could be assessed. Overall survival of all patients was median 60 months and had not been reached for the transplanted patients (Figure). Nine patients died from TRM (11%), 7 during VAD and 2 following HDM. Side effects CTC grade ≥ 2 were recorded in 46% of patients during VAD induction and in 87% of patients after HDM; infections CTC grade ≥ 2 were recorded in 13% and 65%, respectively.
Conclusions: VAD induction followed by HDM and ASCT for AL amyloidosis is feasible, has acceptable TRM, and results in a remarkable prolonged survival. This two-step approach of induction with non-intensive chemotherapy in all patients followed by HDM with ASCT in eligible patients is now recommended as standard treatment by HOVON for newly diagnosed patients with AL amyloidosis who are eligible for high-dose therapy.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author