Abstract
Increased platelet activation is recognized in patients with sickle cell disease (SCD), but its pathogenesis and clinical relevance remain uncertain. Pulmonary arterial hypertension (PAH), an important complication of SCD, is characterized by a proliferative pulmonary vasculopathy, in situ thrombosis, and vascular dysfunction related to scavenging of nitric oxide (NO) by hemoglobin released into blood plasma during intravascular hemolysis. We investigated links between platelet activation, PAH and NO scavenging in patients with SCD. Platelet activation marked by activated fibrinogen receptor correlated to the severity of PAH (r = 0.58, P < .001) and to laboratory markers of intravascular hemolysis, such as reticulocyte count (r = 0.44, P = .02). In vitro exposure of platelets to pathologically relevant concentrations of cell-free hemoglobin promoted basal- and agonist-stimulated activation and blocked the inhibitory effects on platelet activation by an NO donor. In patients with SCD, administration of sildenafil, a phosphodiesterase-5 inhibitor that potentiates NO-dependent signaling, reduced platelet activation (P = .01). These findings suggest a possible interaction between hemolysis, decreased NO bioavailability, and pathologic platelet activation that might contribute to thrombosis and pulmonary hypertension in SCD, and potentially other disorders of intravascular hemolysis. This supports a role for NO-based therapeutics for SCD vasculopathy. This trial was registered at www.clinicaltrials.gov as no. NCT00352430.
Introduction
A chronic state of hemostatic activation in sickle cell disease (SCD) has been well documented by several investigators. Some have highlighted the role of the sickle red cell1,2 ; others have highlighted the contribution of abnormal tissue factor and secondary thrombin generation by a dysfunctional endothelium,3 the depletion of endogenous anticoagulants,4 or the activation of white blood cells.5 It is likely that the increased expression of adhesion molecules, tissue factor, and thrombin generation, the result of chronic endothelial dysfunction or acute injury, are all important contributors to the coagulopathy of SCD.6
Increased platelet activation is another known component of hemostatic activation in patients with SCD1,7–9 Increased percentages of platelets are activated during steady state in patients with SCD, and this accelerates during vaso-occlusive crisis (VOC).7–9 The exact inciting mechanism and clinical consequences of this process remain unknown, but platelet activation hypothetically might play a role in the development of chronic vascular complications, such as pulmonary arterial hypertension, by secreting mitogenic and vasoactive substances that promote intimal hyperplasia. In patients without SCD, platelet-derived growth factor plays a fundamental role in the pathogenesis of plexogenic pulmonary hypertension, and pathologic platelet activation likely contributes to the in situ thrombosis in pulmonary hypertension, which has recently been reviewed.10
Pulmonary arterial hypertension (PAH) is a common and serious vascular complication of SCD associated with early mortality in patients with SCD. PAH is found in about 30% of adults with SCD, with a mortality rate of at least 40% at 40 months.11–14 As seen in other forms of pulmonary hypertension, its histopathology features obliterative vascular smooth-muscle proliferation, resulting in vascular stenosis, abnormal endothelium, and in situ thrombosis.15,16 High levels of endothelial activation markers, including soluble vascular cell adhesion molecule-1 (sVCAM-1), are seen.17 Although its pathogenesis is likely multifactorial, PAH in SCD is epidemiologically associated with multiple markers of intravascular hemolysis.11,12,18 Intravascular hemolysis releases hemoglobin and arginase into blood plasma, where the former scavenges nitric oxide (NO), and the latter depletes plasma of L-arginine, the obligate substrate for NO synthase, with both processes severely reducing NO bioavailability.11,19,20 In a normal vascular environment, NO synthesized by the endothelium and platelets promotes vasodilatation and inhibits platelet activation and aggregation as well as endothelial adhesion.21–26
There is evidence in other diseases characterized by vascular dysfunction and impaired NO bioavailability that platelets are pathologically activated.27,28 In addition, platelet activation has been observed in patients with pulmonary hypertension associated to β-thalassemia.29 We therefore sought to determine the potential links between increased platelet activation, pulmonary hypertension, and clinical markers of hemolysis in patients with SCD, and to mechanistically examine in vitro and in vivo the role of cell-free hemoglobin and NO signaling on basal and stimulated platelet activation. The results of these studies suggest a pathologic mechanism linking platelet activation to PAH in SCD, via the intermediacy of NO inactivation by cell-free plasma hemoglobin. This mechanism may have additional relevance to other causes of intravascular hemolysis that predispose to thrombosis, such as paroxysmal nocturnal hemoglobinuria, thrombotic thrombocytopenic purpura, and disseminated intravascular coagulation.
Patients and methods
Study population
All subjects were enrolled in a protocol approved by the Institutional Review Board of the National Heart, Lung and Blood Institute (NHLBI) after written informed consent was obtained in accordance with the Declaration of Helsinki. Our main study group consisted of a convenience sample of 33 adult patients with homozygous sickle cell disease (HbSS) seen at the Clinical Center of the National Institutes of Health (NIH) in Bethesda, MD. The group consisted of 16 patients with PAH and 17 without PAH, whose clinical and laboratory characteristics are summarized in Table 1. None of these patients had received transfusions during the 4 weeks prior to their blood draws or therapy with aspirin or other nonsteroidal anti-inflammatory drugs during the previous week. In addition, blood specimens were obtained from 25 healthy control participants (14 African-American and 11 white) for baseline measurement of platelet activation and 21 patients with SCD admitted to the hospital with the diagnosis of VOC, defined as an acute episode of pain that required a hospital admission for appropriate management. The results of the comparisons were not significantly different when non–African-American control participants were excluded from the analysis.
Samples for in vitro platelet activation experiments were obtained from 3 healthy adult African-American patients who had not received any medication during the previous week, and from 10 patients with SCD at steady state. Finally, we obtained blood samples from a group of 12 patients with SCD and PAH being treated with sildenafil. To assess the effect of sildenafil on their platelet activation, baseline samples were drawn at least 8 hours after the previous dose was given, and a posttreatment sample was drawn at the expected time of peak sildenafil blood levels, approximately 2 hours after an oral dose of 50 to 100 mg.30
Blood sample collection
Peripheral blood samples were obtained by standard venous puncture using a light tourniquet and discarding the first 2 mL of blood to avoid platelet activation.
The samples from the study group were obtained during routine clinic visits or elective hospitalizations while in steady state, within a 2-week period of their last echocardiogram or as specified.
Materials
Chemicals.
Adenosine diphosphate (ADP) was obtained from Bio/Data (Horsham, PA), thrombin receptor–activating peptide (TRAP) was obtained from Bachem (Torrance, CA), the arginine-glycine-aspartate-serine (RGDS) peptide was obtained from Sigma (St Louis, MO), and formaldehyde was obtained from Polysciences (Warrington, PA). MAHMA-NONOate and DEA-NONOate were purchased from Alexis USA (San Diego, CA). Healthy human hemoglobin was purified from red blood cells by hypotonic lysis and differential centrifugation as previously described.31
Monoclonal antibodies.
PerCp-labeled anti-CD61, FITC-labeled PAC1, PE-labeled anti-CD62P, and PE-labeled mouse anti-human IgG1 antibodies were purchased from Becton Dickinson (San Jose, CA).
Preparation of whole-blood platelet samples
Whole-blood samples were used to determine the in vivo baseline and stimulated platelet activation of patients and controls. Upon withdrawal, citrated venous whole blood (450 μL) was mixed gently with either 50 μL phosphate-buffered saline (PBS), 50 μL of 1 to 10 μM (final concentration) ADP or 50 μL of 1 to 100 μM (final concentration) TRAP and allowed to incubate for 3 minutes at 22°C (room temperature).
Preparation of PRP samples
Platelet-rich plasma (PRP) samples were used during the in vitro experiments to study the effects of cell-free hemoglobin, platelet agonists, and NO on platelet activation. For their preparation, the blood was drawn into sodium citrate tubes and immediately centrifuged at 750g for 5 minutes at 22°C. The supernatant was separated and diluted 1:10 in PBS. The samples were then gently mixed with either increasing concentrations (0-100 μM) of purified human hemoglobin, a fixed concentration of ADP (2.5 μM), or MAHMA NONOate (50 μM) alone or in combination, and allowed to incubate for 10 minutes at 22°C.
Flow cytometry for detection of platelet activation
One 5-μL aliquot from each whole-blood or PRP sample was added to tubes containing saturating concentrations of either FITC-labeled PAC-1, PE-labeled mouse anti-human IgG1 and Per-CP–labeled CD-61, or FITC-labeled PAC-1, PE-labeled CD-62P, and Per-CP–labeled CD-61with RGDS as a competitive inhibitor of PAC-1 binding. Samples were incubated in the dark at room temperature for 15 minutes, fixed with 1 mL of cold 1% paraformaldehyde solution, and stored at 4°C. Samples were analyzed on a FACScan flow cytometer (Becton Dickinson). Platelets were distinguished by the characteristic light scatter and the platelet-specific antibody CD61 binding to GPIIb/IIIa, the fibrinogen receptor. After appropriate color compensations were defined, the percentage of platelets positive for PAC-1, representing activated fibrinogen (activated GPIIb/IIIa) receptors, or CD62-P, representing the surface expression of P-selectin (a marker of platelet alpha-granule release) were calculated from 20 000 events positive for CD-61 with a fluorescent intensity greater than a threshold set at 1% from the respective negative control sample. Pilot experiments showed no significant interference of by anti-CD61 on PAC-1 binding to platelets (data not shown). For the purposes of comparison, platelet activation levels were also analyzed in the assays on patients in steady state by determining the mean fluorescence intensity (MFI) of the PAC-1 or anti-CD62–P staining. The comparison of platelet activation on these specimens between patients with and without pulmonary hypertension was also analyzed as percentage of platelets above the activation threshold or as platelet MFI. These results corroborated each other (Tables S1Table S2. SCD Patients on hydroxyurea: PAH vs. no PAH (PDF, 12.4 KB)Table S3. SCD Patients off hydroxyurea: PAH vs. no PAH (PDF, 12.4 KB)Table S4. Correlations of TRV to platelet activation markers by hydroxyurea status (PDF, 14.2 KB)Table S5. Correlation between GPIIb/IIIa activation and surface P-selectin, percentage activated, and mean florescence intensity (PDF, 14.1 KB)Table S6. Mean fluorescent intensity: SCD without PAH vs. with PAH (PDF, 12.4 KB)–S7, available on the Blood website; see the Supplemental Tables link at the top of the online article). We elected to present the platelet activation data in this paper as percentage above threshold, consistent with most other similar published studies.
Measurement of pulmonary artery pressures
Pulmonary hypertension was defined as the presence of a tricuspid regurgitant jet velocity (TRV) equal or higher than 2.5 m/second measured on continuous-wave Doppler echocardiograms (equivalent to a pulmonary artery systolic pressure of approximately 30 mmHg) as previously described.11 These echocardiograms were performed during outpatient visits while the patients were relatively pain-free and clinically stable.
Laboratory assays
Blood samples for standard clinical laboratory tests were obtained at the same time as the platelet activation samples and determined by standard techniques at the Department of Laboratory Medicine of the NIH Clinical Center.
Statistics
Multiple groups of data were compared by 1-way analysis of variance (ANOVA), if significant, were further evaluated by the Bonferroni multiple comparison test. Paired and unpaired individual group samples were compared by appropriate Student t tests, while correlations were performed by 2-tailed nonparametric Spearman correlations and linear regression analysis with 95% confidence interval; P values less than .05 were considered significant. All data are presented as the means plus or minus standard error of the mean, unless otherwise specified. In the data presented in Figure 4, similar results were obtained by either paired t test or Wilcoxon signed rank test.
Results
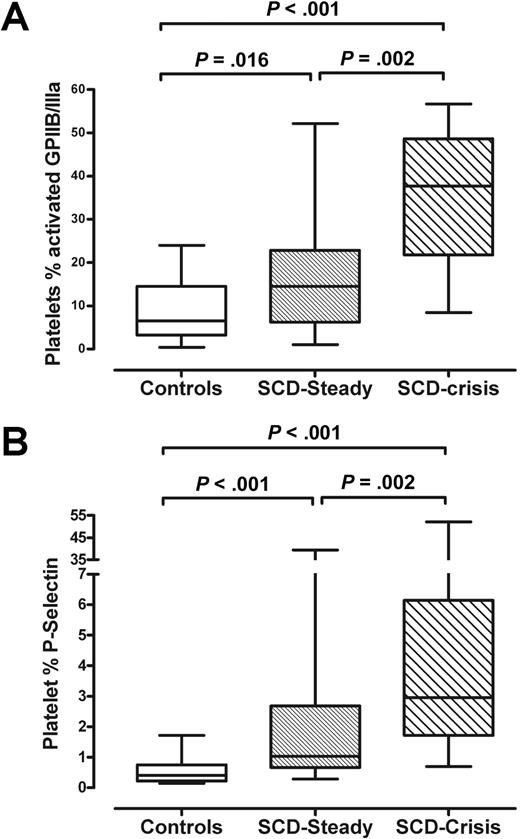
Platelet activation in patients with SCD at rest and during VOC
The 3-color flow cytometric analysis of our samples demonstrated higher mean percentages of activated platelets in 33 patients with SCD at steady state compared with 25 healthy control participants (percentage of platelets displaying activated GPIIb/IIIa receptors: 17.6% ± 2.4% vs 9.4% ± 1.6%, P < .05; surface expression of P-selectin: 3.4% ± 1.2% vs 0.5% ± 0.1%, P < .05), with the highest levels of platelet activation observed in the 21 patients with SCD during acute pain crisis (activated GPIIb/IIIa receptors: 34.8% ± 3.2%; surface expression of P-selectin: 7.9% ± 3.0%; P < .001) for all comparisons versus controls and patients at steady state (Figure 1). These findings confirm that many patients with SCD have platelet activation levels above normal, with increased activation during VOC.
Platelet activation in control participants and in patients with SCD at steady state and during VOC. Each dot represents the percentage of activated platelets from an individual patient with SCD or control participant, as determined by flow cytometry detection of platelet cell-surface (A) activated fibrinogen receptors and (B) P-selectin. Significant P values are indicated as determined by unpaired t test. P-selectin values were analyzed by the Mann-Whitney test because these results were not normally distributed. Boxes indicate median and interquartile ranges, and whiskers indicate ranges.
Platelet activation in control participants and in patients with SCD at steady state and during VOC. Each dot represents the percentage of activated platelets from an individual patient with SCD or control participant, as determined by flow cytometry detection of platelet cell-surface (A) activated fibrinogen receptors and (B) P-selectin. Significant P values are indicated as determined by unpaired t test. P-selectin values were analyzed by the Mann-Whitney test because these results were not normally distributed. Boxes indicate median and interquartile ranges, and whiskers indicate ranges.
Platelet activation and severity of pulmonary hypertension in SCD
Platelet activation was significantly increased in those patients at steady state with PAH compared those without PAH. A higher percentage of platelets from 17 patients with PAH displayed activated GPIIb/IIIa receptors than those from 16 patients without PAH (27.2% ± 4.6% vs 10.25% ± 1.8%; P < .001). This result was corroborated in these same specimens by the higher percentage of platelets showing surface expression of P-selectin in the patients with PAH (5.1% ± 2.1% vs 2.0% ± 0.7%; P < .03). Qualitatively similar results were obtained when an alternative analysis was performed using mean fluorescence intensity for PAH versus no PAH for both activated GPIIb/IIIa and surface P-selectin (Tables S5Table S6. Mean fluorescent intensity: SCD without PAH vs. with PAH (PDF, 12.4 KB)–S7). Results of subgroup analyses accounting for hydroxyurea use were not significantly different (Tables S1Table S2. SCD Patients on hydroxyurea: PAH vs. no PAH (PDF, 12.4 KB)–S3).
Activated GPIIb/IIIa highly correlated with the level of pulmonary artery pressure as measured by TRV (Table 2). This association was supported by a trend toward correlation between the TRV and the percentage of platelets with P-selectin expression. Another marker of pulmonary hypertension and risk of death in sickle cell disease, the N-terminal pro–brain natriuretic hormone (NT-proBNP)14 also correlated with both markers of platelet activation and activated GPIIb/IIIa and cell-surface P-selectin. These relationships were also not significantly different when hydroxyurea use was taken into account (Table S4). These data provide evidence of a link between platelet activation and PAH in SCD.
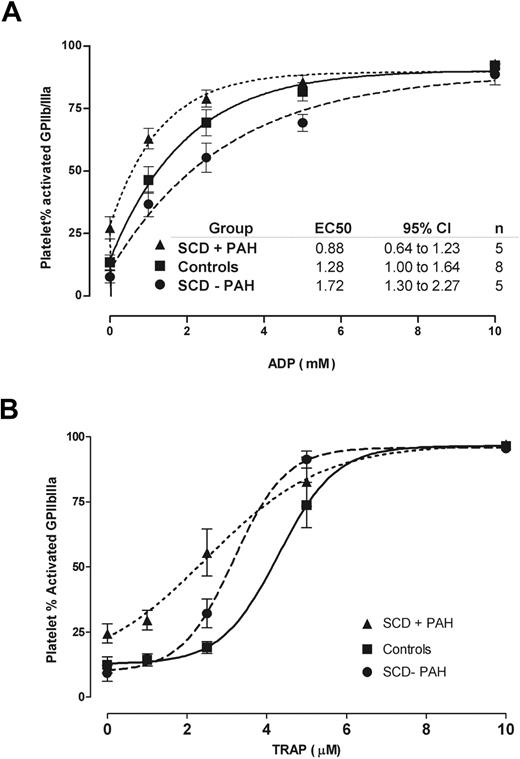
Platelets from patients with SCD with PAH and agonist-induced activation
Whole-blood samples from a subset of patients and healthy control participants were stimulated with escalating doses of the platelet activation agonist ADP to determine threshold concentrations for high level activation. Patients with SCD and secondary PAH reached higher degrees of activation with significantly lower concentrations of ADP (EC50, 0.88 μM; 95% confidence interval [CI], 0.64-1.23 μM) compared with control participants (EC50 1.3 μM; 95% CI, 1.00-1.64; P < .01), and particularly to patients without PAH (EC50 1.7 μM; 95% CI, 1.31-2.27; P < .01) (Figure 2A). This appears primarily due to the high basal level of activation in the platelets from patients with SCD with PAH, which was maintained throughout the ADP titration range. For unclear reasons, platelets from patients with SCD without PAH were less easily activated than platelets from control participants. Platelets from patients with SCD with PAH also reached high-level activation with lower concentrations of TRAP than patients with SCD without PAH and control participants (Figure 2B). These ex vivo findings suggest that patients with SCD and pulmonary hypertension may attain high percentages of activated platelets in vivo with only low levels of platelet agonists.
Effects of agonist-induced activation on platelets from patients with SCD or healthy participants. (A) ADP reactivity of platelets from patients with SCD and PAH. The curves represent the mean percentage plus or minus SEM of activated platelets (activated GPIIb/IIIa) after their incubation with increasing concentrations of ADP. Patients with SCD and secondary pulmonary hypertension (SCD + PAH; ▲) reached higher degrees of activation with significantly lower concentrations of ADP compared with control participants (■) and patients with SCD without PAH (SCD − PAH; ●). (B) Reactivity of platelets from patients with SCD and PAH to activation by TRAP is compared with that of platelets from healthy control participants or patients with SCD without PAH.
Effects of agonist-induced activation on platelets from patients with SCD or healthy participants. (A) ADP reactivity of platelets from patients with SCD and PAH. The curves represent the mean percentage plus or minus SEM of activated platelets (activated GPIIb/IIIa) after their incubation with increasing concentrations of ADP. Patients with SCD and secondary pulmonary hypertension (SCD + PAH; ▲) reached higher degrees of activation with significantly lower concentrations of ADP compared with control participants (■) and patients with SCD without PAH (SCD − PAH; ●). (B) Reactivity of platelets from patients with SCD and PAH to activation by TRAP is compared with that of platelets from healthy control participants or patients with SCD without PAH.
Platelet activation and laboratory markers of hemolysis
Flow cytometric markers of platelet activation correlated with clinical laboratory markers of hemolytic severity. While the hemoglobin level was inversely correlated to the degree of activation as assessed by surface P-selectin (with a similar trend seen with GPIIb/IIIa activation), clinical markers of hemolysis such as serum lactate dehydrogenase and reticulocyte count were directly correlated to the degree of activation. We found no correlation between markers of platelet activation and platelet count (P > .1) or white blood cell counts (P > .1). These findings, summarized in Table 3, suggest a link between platelet activation and the severity of intravascular hemolysis.
Effects of cell-free hemoglobin on NO inhibition of platelet activation
To investigate a possible link between hemolysis-associated NO scavenging and platelet activation, we performed a series of in vitro experiments. We exposed PRP samples to increasing concentrations of purified human cell-free hemoglobin (0-100 μM final concentration), and/or to a fixed concentration of the NO donor MAHMA NONOate (50 μM). The percentage of activated platelets tended to increase with increasing hemoglobin concentrations within the range of values found in plasma of patients with SCD in steady state (P = .08, 1-way ANOVA), while the NO-mediated inhibition of platelet activation was blocked by hemoglobin in a dose-dependent fashion (P = .002; Figure 3A). This result indicates that cell-free hemoglobin induces platelet activation in vitro via a mechanism that is partially reversible by NO.
Effects of cell-free hemoglobin and NO exposure on platelet activation. (A) The in vitro exposure of purified human cell-free hemoglobin to platelets from healthy donors increased the percentage of activated platelets as indicated by cell-surface expression of activated GPIIb/IIIa (Plt + Hb; ■). The NO donor MAHMA-NONOate (50 μM) inhibited baseline activation, but this inhibitory effect was overcome by the NO-scavenging activity of cell-free hemoglobin in a dose-dependent manner (Plt + Hb + NO; ▲). (B) Platelet activation was induced significantly by cell-free hemoglobin. Activation was inhibited by the NO donor, but this inhibition was eliminated by the addition of 50 μM cell-free hemoglobin. The markers and bars represent the mean percentages (± SEM) of activated platelets after 3 experiments of healthy donor samples (*P < .05 compared with baseline samples; †P < .05 compared with NO alone; paired t test). (C) The induction of platelet activation by ADP was nearly abolished by the NO donor, but this action was again inhibited by cell-free hemoglobin (50 μM).
Effects of cell-free hemoglobin and NO exposure on platelet activation. (A) The in vitro exposure of purified human cell-free hemoglobin to platelets from healthy donors increased the percentage of activated platelets as indicated by cell-surface expression of activated GPIIb/IIIa (Plt + Hb; ■). The NO donor MAHMA-NONOate (50 μM) inhibited baseline activation, but this inhibitory effect was overcome by the NO-scavenging activity of cell-free hemoglobin in a dose-dependent manner (Plt + Hb + NO; ▲). (B) Platelet activation was induced significantly by cell-free hemoglobin. Activation was inhibited by the NO donor, but this inhibition was eliminated by the addition of 50 μM cell-free hemoglobin. The markers and bars represent the mean percentages (± SEM) of activated platelets after 3 experiments of healthy donor samples (*P < .05 compared with baseline samples; †P < .05 compared with NO alone; paired t test). (C) The induction of platelet activation by ADP was nearly abolished by the NO donor, but this action was again inhibited by cell-free hemoglobin (50 μM).
We found additional evidence in unstimulated and agonist-stimulated platelets from healthy control participants that cell-free hemoglobin blocks NO effects on platelets. Consistent with published data, a NO donor inhibited platelet activation in unstimulated platelets (P < .05; Figure 3B). Conversely, cell-free hemoglobin induced platelet activation from the baseline (P < .05), and completely abolished the inhibitory effect of NO (P < .05). In the same experiments, platelet activation was induced in vitro readily by 2.5 μM ADP (Figure 3C). The NO donor completely extinguished this ADP-induced platelet activation. Although hemoglobin did not show a priming effect in potentiating ADP-induced activation, more important, cell-free hemoglobin inhibits the platelet-inhibitory activity of NO. These findings suggest that platelets may become activated upon exposure to cell-free hemoglobin, and demonstrate that normal NO-inhibitory effects on platelet activation can be blocked by cell-free hemoglobin.
Platelet activation reduced by sildenafil in patients with SCD and PAH
In 12 patients with SCD and PAH, we investigated the effects of the pulmonary vasodilator sildenafil citrate on markers of platelet activation. In tissues that express phosphodiesterase-5 (PDE5), this drug amplifies NO signaling by inhibiting hydrolysis of the NO signal transduction mediator, cyclic GMP. Given that PDE5 is present in human platelets, the effect of NO and NO donors on platelet function is potentiated by sildenafil.32,33
At times of trough drug levels, GPIIb/IIIa activation was detectable in all 12 patients. This activation decreased significantly at the expected time for the peak plasma level of sildenafil, 2 hours after its oral administration (30.6% ± 4.4% vs 17.3% ± 3.6%; P = .01) (Figure 4). A similar trend was observed for the reduction of platelet surface expression of P-selectin by sildenafil (6.3% ± 1.6% vs 3.2% ± 0.6%; P = .08). This result suggests that enhancement of platelet sensitivity to NO by PDE5 inhibition restores platelet activation to more normal levels in patients with SCD and PAH.
Effects of sildenafil on platelet activation of patients with SCD and PAH. The lines connect the percentages of activated platelets of 12 patients before and after (off-on) a dose of sildenafil. The percentage of activated platelets decreased after sildenafil from 30.6% (± 4.4%) to 17.3% (± 3.6%) for activated GPIIb/IIIa (P = .01, paired t test), and from 6.3% (± 1.6%) to 3.2% (± 0.6%) for P-selectin (P = .08).
Effects of sildenafil on platelet activation of patients with SCD and PAH. The lines connect the percentages of activated platelets of 12 patients before and after (off-on) a dose of sildenafil. The percentage of activated platelets decreased after sildenafil from 30.6% (± 4.4%) to 17.3% (± 3.6%) for activated GPIIb/IIIa (P = .01, paired t test), and from 6.3% (± 1.6%) to 3.2% (± 0.6%) for P-selectin (P = .08).
Discussion
The present study provides insights regarding increased platelet activation in patients with SCD. We show that increased platelet activation is associated with high hemolytic rate and the severity of PAH in these patients. In addition, our data indicate a heightened state of platelet reactivity to agonist stimuli and that free hemoglobin may trigger platelet activation and block the inhibitory effects of nitric oxide on platelet activation. Confirming the relevance of the NO pathway to platelet activation in vivo, we demonstrate reversal of platelet activation by specific PDE5 inhibition in patients with SCD and PAH.
Increased platelet activation has been described in patients with SCD,8,9,35 a phenomenon that may contribute to the hemostatic activation observed in SCD. The mechanism responsible for this heightened degree of activation is not fully understood, but thought to be the result of the proinflammatory and prothrombotic characteristics of the microvasculature in SCD.1,2,35–38 The novel link between platelet activation and severity of pulmonary hypertension in SCD identified in our study may offer a new perspective into the pathobiology of both conditions. PAH is a chronic vasculopathy recognized as the greatest mortality risk factor in the adult population with SCD.11 Its origin is likely multifactorial, but its pathophysiology, characterized by increased vascular tone, vascular proliferation, and in situ thrombosis, is ascribed in part to a hemolysis-associated impairment of NO bioavailability.11,12,39 Patients with all forms of PAH are at risk for the development of in situ pulmonary thrombosis, and these are seen prominently in autopsy studies, including PAH in SCD.40–42 Activated platelets conceivably might play a direct role in the development of these thrombi, which worsen pulmonary hypertension. Furthermore, their degree of activation might be a marker for ongoing prothrombotic activity and risk of pulmonary thrombi.43 This intriguing hypothesis will require further investigation.
The statistical link between platelet activation, intravascular hemolysis, and PAH in SCD may reflect a common mechanism, the decreased NO bioavailability associated with severe hemolysis in patients with SCD and PAH. Chronic intravascular hemolysis releases erythrocyte hemoglobin and arginase into plasma. The hemoglobin stoichiometrically inactivates endothelium-derived NO, while the arginase depletes plasma arginine, the obligate substrate for NO synthesis, through conversion of arginine to ornithine. In this model, reduced NO bioavailability and endothelial dysfunction results in the clinical development of pulmonary hypertension.11,28,44,45 Increased platelet activation is another well-described consequence of endothelial dysfunction and decreased NO bioavailability.25,46
In addition to the associations of platelet activation with PAH and hemolytic rate, our data indicate that platelets in patients with SCD and PAH are easily activated to high levels ex vivo. A similar phenomenon has been described by Rickles and others when performing platelet aggregation studies on specimens from patients with SCD.47 It was not within the scope of this study to identify the causes for this finding, but increased baseline activation levels were readily augmented by low doses of agonists in platelets from patients with PAH. Furthermore, we found that exogenous cell-free hemoglobin could reproduce this platelet reactivity in platelets from healthy donors, and even block the inhibitory effect of NO donors ex vivo, in the process apparently generating methemoglobin, the hallmark of hemoglobin oxidation by NO. There are many other potential platelet agonists in vitro in SCD, including ADP released from lysed red cells, and thrombin, generated due to tissue factor activation in SCD. Since our platelet preparations contained leukocytes and intact erythrocytes, we cannot rule out a role of those cells in producing activation. We also note in our data higher sensitivity of the conformation-dependent antibody to the fibrinogen receptor compared with surface P-selectin. This might be technical, due to shedding of the surface P-selectin, or might represent some potential intermediate state of platelet activation. Thus, the platelet activation syndrome in SCD may be multifactorial, but the ability of NO donors or scavengers to modify the activation state ex vivo in our results is significant, and consistent with our data correlating activation in vivo to pulmonary pressure and hemolytic rate. This suggests that hemolysis-associated defects in NO bioactivity in SCD may have consequences on platelet activation, and conversely, platelet activation may serve as a marker of endothelial dysfunction and activation in SCD consequent to low NO bioactivity.
Sildenafil is a drug that may provide dual therapeutic benefits in patients with SCD and PAH. A pilot study from our group indicated that sildenafil improves pulmonary hypertension and exercise capacity in patients with SCD.48 Other investigators from our institution have shown that sildenafil inhibits platelet activation while improving endothelial function and coronary artery vasodilation in people without SCD.49 In addition to relieving pulmonary pressures in patients with SCD and PAH, our study confirms that sildenafil provides the additional benefit of decreasing platelet activation. A heterogeneous, predominantly favorable therapeutic response was observed, as might be expected for a heterogeneous group of adult patients with SCD with a variety of comorbid complications and concurrent drug therapies. The effects of NO in human platelets has both soluble guanylate cyclase (sGC)–dependent and sGC-impendent pathways.50 Sildenafil potentiates NO platelet antiaggregation effects mainly by its inhibition of PDE5, a sGC-dependent pathway. Mechanisms involving other platelet phosphodiesterases and cyclic AMP had been described as participating on NO antisecretory effects.51 These effects might conceivably reduce the incidence of the well-known PAH complication of in situ pulmonary thrombosis.
Cerebrovascular disease is another complication of SCD bearing striking similarities to PAH in risk factors, physiology, and histopathology.26 Although the present study did not involve prospective assessment and follow-up of cerebrovascular disease, 3 patients who had among the highest levels of baseline platelet activation subsequently suffered clinical strokes during the course of the study (data not shown). This anecdotal observation raises the provocative question whether platelet activation may be a risk factor for stroke in SCD. We hypothesize that platelet activation may be part of a shared pathophysiology between PAH and cerebrovascular disease, potentially both related to impaired NO bioavailability. This hypothesis merits investigation.
SCD is not the only disorder of intravascular hemolysis associated with hemostatic activation. Hemoglobinemia, disordered platelet function, and thrombosis are features of paroxysmal nocturnal hemoglobinuria, thrombotic thrombocytopenic purpura, hemolytic-uremic syndrome, and disseminated intravascular coagulation. There is evidence of platelet activation in these conditions,52–59 but the potential contribution of NO scavenging by plasma hemoglobin to platelet activation and thrombosis has not yet been investigated. This mechanism is supported by evidence of NO scavenging by cell-free cross-linked hemoglobin artificial blood substitutes in rats, promoting platelet deposition at sites of subintimal injury.60 Impaired NO bioavailability and platelet activation might play a general role in the predisposition to thrombosis in hemolytic anemias.
In summary, our findings reveal that patients with SCD and secondary PAH exhibit significant platelet activation, and suggest that hemolysis is a potential pathologic mechanism that contributes to its development. Cell-free hemoglobin can trigger platelet activation, an effect that may be mediated by the consumption of NO, a key inhibitor of platelet activation. The role of the NO pathway in this pathophysiologic mechanism is further highlighted by our observation that sildenafil decreased PAH-associated platelet activation in patients with SCD. It is attractive to hypothesize that in SCD, platelet activation might also be a risk factor for other thromboembolic complications, particularly cerebrovascular disease with stroke, as proposed in cerebral atherosclerosis.61 Further studies of platelet activation in SCD will be required to confirm this mechanistic pathway and potential prognostic value.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Mary K. Hall for protocol coordination, J. Philip McCoy and Michael Riordan for flow cytometry training and technical assistance, and Candido Rivera and Xunde Wang for scientific advice.
This work was supported by intramural funding from the National Institutes of Health Clinical Center and the National Heart, Lung and Blood Institute (M.T.G), extramural grant T32 CA60441 from the National Cancer Institute, and a grant 5K12HD001399 Child Research Center Development Award Grant (J.V.).
National Institutes of Health
Authorship
Contribution: J.V., M.T.G., and G.J.K. planned the study, interpreted results, and prepared the manuscript. J.V. and S.S. obtained the experimental laboratory results. R.F.M. recruited pulmonary hypertension patients, collected blood specimens, and obtained and interpreted clinical pulmonary hypertension data. L.A.H. obtained informed consent, coordinated patient involvement, and obtained and processed blood specimens.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Gregory J. Kato, Director, Sickle Cell Vascular Disease Unit, Vascular Medicine Branch, National Heart Lung and Blood Institute, National Institutes of Health, Bldg 10-CRC, Rm 5-5140, 10 Center Dr, MSC 1476, Bethesda, MD 20892-1476; e-mail: gkato@mail.nih.gov.