Comment on Flotho et al, page 1050
Levels of caspase 8–associated protein 2 (CASP8AP2) are strongly associated with apoptosis, early response to therapy, and event-free survival in children with ALL.
Prognosis of children with acute lymphoblastic leukemia (ALL) has been associated with a variety of disease-, patient-, and treatment-related factors. Some of these make biologic sense (white blood cell count [WBC] at diagnosis as a measure of initial disease burden, rapidity of response to therapy) while others (age at diagnosis, ploidy) are probably surrogates for yet-to-be discovered biologic processes.
Apoptosis is an important mechanism for cell death in ALL. Activation of caspase 8 is important for apoptosis induced by death receptor ligands and may also contribute to activation of the mitochondrial apoptosome. Activation of caspase 8 requires a protein complex that includes CASP8AP2.
In this issue of Blood, Flotho and colleagues correlate rapidity of early response (minimal residual disease [MRD] at days 19 and 46) with gene expression in blasts obtained at diagnosis of ALL. Of the 17 most highly correlated genes, CASP8AP2 was chosen for further analyses because of its roles in apoptosis and in glucocorticoid receptor activation. Higher expression of CASP8AP2 was strongly associated with lower MRD. In an independent cohort, regression analysis indicated that increased risk of relapse was associated with low CASAP8AP2, age older than 10 years, BCR-ABL, and T-ALL. Other factors including race, sex, WBC, and protocol were not significant.
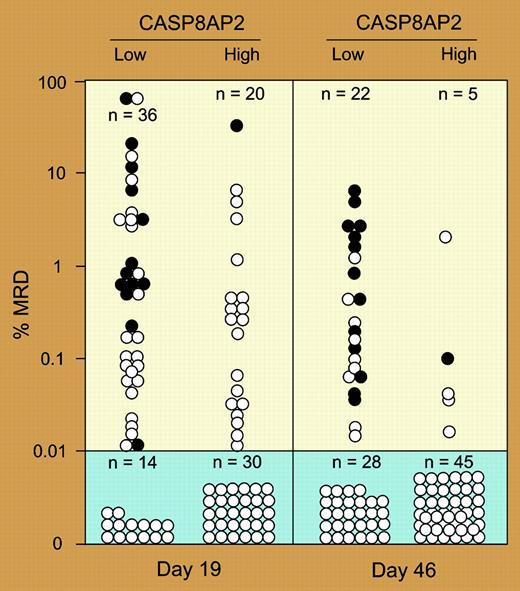
Can we use this information for risk assignment (see figure)? In this study, (1) all relapses occurred in patients with higher levels of MRD, (2) patients with lower CASP8AP2 were more likely to have higher MRD, (3) patients with high or low CASP8AP2 were unlikely to relapse despite high MRD at day 19, and (4) patients with high MRD and low CASP8AP2 at day 46 were more likely to relapse, but fewer were in this category. Thus neither MRD, CASP8AP2 levels, nor a combination of both of these factors predict relapse with 95% sensitivity and specificity.FIG1
MRD at days 19 and 46 in patients with the highest and lowest levels of CASP8AP2. See the complete figure in the article beginning on page 1050.
MRD at days 19 and 46 in patients with the highest and lowest levels of CASP8AP2. See the complete figure in the article beginning on page 1050.
Are the conclusions here generalizable or are they specific to the treatments and methods that were used in this study? Other studies have not found (or tested for) an association of CASP8AP2 with outcomes. In addition, there is no reason to believe that caspase 8 pathways are the only routes to cell death in ALL. Thus MRD should be a sum of the effects of multiple pathways. These in turn may be affected by different treatment plans. In this regard, it would be interesting to know whether MRD or CASP8AP2 was more predictive of relapse in the current study.
Flotho et al have peeled back another layer of the onion, enabling us to get closer to understanding the core biology that affects outcomes in ALL. The ultimate goal is to be able to answer for each individual (as in the game Clue) who, how, and where? ▪