Abstract
Background: The Durie-Salmon staging system utilizes both laboratory features and information on MBS-FL. We hypothesized that, by detecting FL in the bone marrow prior to MBS-recognizable bone destruction, MRI would provide a biologically and clinically more relevant feature of FL-type MM (Tian et al, NEJM 2003).
Patients and Methods: As part of a tandem transplant trial, TT2, MBS, MRI, clinical workup and cytogenetics were performed on 611 cases.
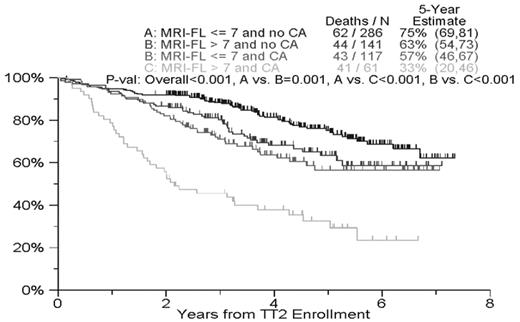
Results: In a comparison of all areas imaged by both techniques, at least one FL was detected in 451 (74%) on MRI and 344 (56%) on MBS; 128 (21%) had no FL by either technique while 312 (51%) showed FL on both MBS and MRI. Importantly, of 267 patients without FL on MBS, 139 (52%) had FL on MRI; conversely, among 160 without FL on MRI, 32 (20%) had FL on MBS examination. The mean FL number among those with FL was 13 in case of MRI and 8 with MBS. Significantly higher proportions of patients had FL on MRI than MBS in spine (78% vs. 16% p<0.001), pelvis (64% vs. 28%, p<0.001) and sternum (24% vs. 3%, p<0.001). Higher FL number on both MRI and MBS and heterogeneity of the diffuse marrow signal on MRI STIR (indicating micro-nodular disease), cytogenetic abnormalities (CA), elevated serum levels of beta-2-microglobulin (B2M), C-reactive protein (CRP) and lactate dehydrogenase (LDH), in case of hypo-albuminemia and advanced age, were prognostically negative. On multivariate analysis (MVA), MRI- but not MBS-defined FL number was an independent adverse baseline feature for overall survival (HR=1.73; p<.001), independent of CA (HR=2.11; p<.001) and elevations of LDH (HR=1.56; p=.006) and B2M levels (HR=1.43; p=.026). Clinical complete response (CCR) (MVA HR=0.60; p=0.007) and MRI-CR (univariately: HR, 0.58; p=0.004) were favorable features when examined as time-dependent variables along with baseline features. Higher MRI-FL number (>7) was significantly associated with higher serum levels of LDH, CRP and creatinine as well as with hypo-albuminemia, whereas no correlations were noted with levels of B2M, bone marrow plasmacytosis, hemoglobin, CA, age, gender, race and Ig isotype.
Conclusion: MRI examination in MM is justified:
as an imaging tool that permits detection of FL long before osteolytic disease is recognized on MBS,
as an independent staging tool with prognostic implications (that should replace MBS used in the Durie-Salmon staging system) after accounting for the presence of CA, LDH and B2M;
as a means of documenting a superior state of CR (MRI-CR) conferring survival advantage, in patients with a high focal lesion number at baseline; and, not addressed here,
as a tool for detecting and staging non-secretory and macro-focal MM, the latter often having minimal or no involvement on random bone marrow examination.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author