Comment on Zhang et al, page 3286
The frequencies of circulating endothelial cells and endothelial progenitors are increased in the blood of myeloma patients and parallel disease activity and response to thalidomide treatment.
Neoangiogenesis is a hallmark and prerequisite of tumor growth, invasion, and metastasis. Its pivotal role in tumor progression has also been established for a number of hematologic malignancies including multiple myeloma (MM). Increased microvessel density in MM marrow is positively correlated to disease activity and is a feature of poor prognosis. As the first clinically available agent with known antiangiogenic activity, thalidomide was consequently introduced as an effective drug in relapsed, refractory, and, most recently, in newly diagnosed MM (reviewed in Kyle and Rajkumar1 ). Yet, it is still a matter of debate whether thalidomide primarily acts through targeting of MM-associated marrow neoangiogenesis.
In recent years, intense research has also been devoted to the elucidation of tumor neovessel formation and, in particular, to the phenotype and origin of endothelial cells (ECs) involved. In addition to the recruitment of angiogenic ECs from neighboring micro-capillaries, a growing body of experimental work suggests that circulating endothelial progenitor cells (EPCs) essentially contribute to tumor angiogenesis. These EPCs are thought to originate from hemangioblasts persisting in adult bone marrow (reviewed in Ribatti,2 and Bailey and Fleming3 ). In a murine model, impaired recruitment of marrow-derived circulating EPCs was even shown to block tumor angiogenesis and growth, a finding that might pave the path for novel antiangiogenic strategies of cancer treatment.4 Along these lines, further intriguing evidence comes from studies in chronic myeloid leukemia. The latter data suggest that the endothelial progeny might also be derived from hemangioblastic precursors carrying the BCR/ABL fusion gene of the malignant clone.5
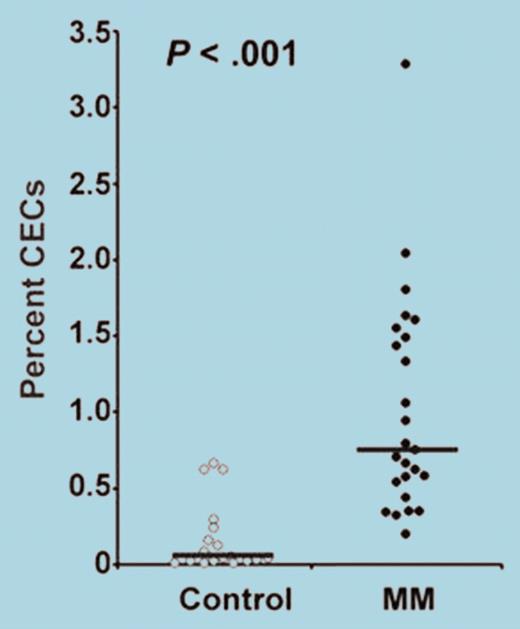
In the current issue of Blood, Zhang and colleagues demonstrate that circulating ECs (CECs) are significantly increased in the peripheral blood of MM patients (see figure) and that their frequency covaries with markers of disease activity, viz, levels of M protein and β2-microglobulin. Among CECs are EPCs endowed with angioblastic and neovascularization capabilities, and both CECs and EPCs decline in parallel as the disease responds to thalidomide treatment. EPCs in MM were shown to coexpress vascular endothelial growth factor receptor-2 (kinase insert domain-containing receptor/fetal liver kinase-1 [KDR]) and CD133 and to account for KDR mRNA elevations, which also correlate with M protein levels.FIG1
Frequency of circulating endothelial cells (CECs) shown as percentage of peripheral blood mononuclear cells in myeloma (MM) patients and healthy control subjects. See the complete figure in the article beginning on page 3286.
Frequency of circulating endothelial cells (CECs) shown as percentage of peripheral blood mononuclear cells in myeloma (MM) patients and healthy control subjects. See the complete figure in the article beginning on page 3286.
Clearly, the data demonstrate that CECs/EPCs can serve as novel biomarkers of myeloma activity. Whether they add to the information provided by parameters currently in routine use will have to be shown by larger longitudinal studies. In addition, the correlation of CECs/EPCs with response to thalidomide treatment may suggest a previously unknown, direct or indirect, antiangiogenic mechanism of thalidomide action. However, whether such correlations are unique to thalidomide and its derivatives will also require further clinical investigations. Finally, the obvious assumption that circulating EPCs indeed contribute to neoangiogenesis in MM marrow and, consequently, to MM progression will have to be substantiated by appropriate experimental data. Although these and other questions remain, the authors have introduced important new perspectives on the potential mechanisms and therapeutic targets of MM-associated neoangiogenesis. ▪