Abstract
A model of gram-negative lethal endotoxin shock, involving continuous peritoneal infusion of lipopolysaccharide (LPS), has been applied to wild-type (WT) mice and mice with a severe deficiency of endothelial protein C receptor (EPCRδ/δ). The survival of EPCRδ/δ mice was significantly diminished as compared to WT mice after administration of LPS via this route. Heart rates and central blood pressures also were significantly more depressed in EPCRδ/δ mice, indicating that the receptor-based protein C (PC) pathway functions in regulation of hemodynamic properties in the mouse. Further, heart muscle damage was more severe in EPCRδ/δ mice as compared to WT mice after endotoxin administration, as revealed by the more elevated plasma myoglobin levels in EPCRδ/δ mice and by microscopic examination of stained heart sections. Neutrophil infiltration was more pronounced in heart tissue of EPCRδ/δ mice, perhaps in response to the greatly increased expression level of the chemokine, MIP-2, which also significantly more up-regulated in the LPS-treated EPCRδ/δ mouse cohort. In conclusion, a severe deficiency of EPCR adversely affects survival of mice subjected to continuous infusion of endotoxin, via contributions of more responsive hemodynamic and cardiac alterations, thus suggesting that, among its other functions, the PC-based receptor system has a cardioprotective role after acute inflammatory challenge.
Introduction
Complications that arise during severe sepsis involve both coagulopathies and inflammatory reactions, and the presence of one of these states reinforces the development and progression of the other.1 One important pathway in the crosstalk between coagulation and inflammation occurs through the natural protein C (PC) anticoagulation pathway, optimal activation of which requires PC, its endothelial cell (EC) receptor, EPCR, its cellular activation modulator, thrombomodulin (Tm), and the PC protease activator, thrombin.2 PC signaling mechanisms, likely important to its anti-inflammatory properties, are believed to occur via binding of its activated form (aPC) to EPCR and the further involvement of coreceptor(s) of the protease-activated receptor family.3 Thus, the down-regulation of PC system components that occurs during acute inflammation cannot only lead to enhanced coagulation, up-regulation of a variety of inflammatory mediators,4-7 and activation and infiltration of inflammatory cells,8,9 but it also can lead to more indirect effects that involve thrombin-mediated signaling, through concomitant up-regulation of thrombin levels.
Apoptosis also plays a critical role in sepsis-mediated organ death, including that of the heart,10 in several possible ways, for example, by induction of EC death,11 by depletion of immune cells needed to combat infection,12 and/or by delaying invasive neutrophil death.13 aPC is an antiapoptotic protein and functions in this regard through modification of a number of relevant genes.14 In addition, it has been shown that the aPC/EPCR/PAR-1 pathway blocks p53-dependent apoptosis in ischemic brains,15 thus perhaps offering general protection of the endothelium from downstream ischemic damage in thrombotic episodes. Other studies have shown that murine neuronal cells are protected by aPC from N-methyl-D-aspartate (NMDA)– and staurosporine-induced apoptosis in a PAR-1– and PAR-3–dependent fashion.16,17
EPCR also may function independently as an anti-inflammatory agent. During inflammation, EPCR is shed from EC through limited proteolysis by thrombin or a metalloproteinase.18 The soluble form of EPCR binds to neutrophils in an integrin-dependent fashion.19 This process could inhibit neutrophil binding to the endothelium, thereby attenuating neutrophil trafficking.
Because of these multiple functions of aPC, interest has arisen in the drug potential of this system to counter the inflammatory, coagulant, and apoptotic responses in severe sepsis, and some success has been attained in a subset of these patients.20 In order to more fully assess the importance of EPCR in acute inflammatory damage and to determine whether EPCR lies on the in vivo mechanistic pathway of the benefits accrued by aPC, mice with a severe targeted genetic deficiency of EPCR have been used herein using a model of continuous intraperitoneal lethal lipopolysaccharide (LPS) administration, followed by studies of survival rates, thrombotic and inflammatory changes, and organ damage. The results of this study are summarized herein.
Materials and methods
Mice
The characteristics of low EPCR-expressing mice (EPCRδ/δ) have been described in a previous report.21 The mice were back-crossed for more than 10 generations into the C57Bl/6J (Jackson Laboratories, Bar Harbor, ME) strain. Male EPCRδ/δ mice at 7 to 8 weeks of age were used in this study. All mouse protocols were approved by the Institutional Animal Care and Use Committee (IACUC) of the University of Notre Dame.
LPS challenge
LPS (serotype O111:B4, Sigma, St Louis, MO) was dissolved in isotonic saline at a concentration of 5 μg/μL. A volume of 100 μL of this solution was placed in the osmotic pumps (model 1003 D; Durect, Cupertino, CA). A longitudinal 1-cm abdominal incision was made in the mice after shaving the surface and disinfecting with an iodine solution. The LPS-containing osmotic pumps were implanted into the peritoneal cavities, and the skins sutured with a 5.0 vycryl thread. This pump releases its contents at the rate of 1 μL/hour. The dose of LPS used was determined by preliminary experiments in male WT C57Bl/6J mice, such that 30% to 40% of these animals would die within 72 hours. Survival rates were then evaluated for 72 hours after the implantation of the pumps. In a separate series of experiments, mice were killed at various time points, and blood and tissue samples were collected.
Blood pressure (BP) measurements
Telemeters (model TA-F20 mouse transmitter; Data Sciences International, Arden Hills, MN) were implanted in the thoracic aortas of mice. Prior to doing so, the mice were anesthetized with an intraperitoneal dose of 0.075 mg ketamine/0.015 mg xylazine/0.0025 mg aceprozamine/g weight of mouse. After a longitudinal midline neck incision was made, the left common carotid artery was isolated and retracted (7-0 silk), and a small incision was made therein. The pressure-sensing catheter was inserted into the left carotid artery by use of vessel cannulation forceps. The catheter was then advanced 10 mm, such that the tip resided just inside the thoracic aorta and then secured by ligatures. The transmitter body was tunneled subcutaneously to a small pouch along the left ventral flank. The neck incision was closed with 6-0 silk, and the mice allowed to fully recover from anesthesia. After 7 days in cages that were placed on telemetric receivers, the devices were magnetically activated. Baseline values of systolic and diastolic arterial BPs, heart rates (HR), and pulse pressures (PP) were recorded. After this time, the osmotic pumps containing LPS were implanted in the animals. These same parameters were then recorded continuously for 72 hours, with sampling every 5 minutes for 10-second intervals. Data were collected online and stored using a Dataquest ART data acquisition system (Data Sciences International).
Assays for hemostasis function
Complete exsanguinations from vena cavas were performed and the blood placed in sodium citrate for coagulation tests or EDTA-2K (ethylenediaminetetraacetic acid-2K) for complete blood counts.
Platelets were counted in EDTA-treated blood using a VetScan HMT Hematology Analyzer (ABAXIS, Union City, CA).
Prothrombin times (PT) and activated partial thromboplastin times (aPTT) were determined using STA-NEOPLASTIN (rabbit brain thromboplastin) and STA-PTT AUTOMATE kits, respectively (Diagnostica Stago, Asnieres, France). The activity of FVII, FXI, and FXII were determined by the STA-Deficient VII, XI, and XII kits, respectively (Diagnostica Stago). All clotting assays were carried out with the STart 8 Coagulation Analyzer (Diagnostica Stago).
Generation of control RNA vectors for quantitative reverse transcription–polymerase chain reaction (Q-RT-PCR)
PCR primers and probes for tumor necrosis factor α (TNFα), interleukin 1 β (IL)1β, IL6, macrophage chemotaxis protein-1 (MCP-1), macrophage inflammatory chemokine-2 (MIP-2), inducible nitric oxide synthetase (iNOS), hypoxia inducible factor 1α (HIF1α), and vascular endothelial growth factor (VEGF), along with the housekeeping genes hydroxyphosphoribosyl transferase (HPRT) and ribosomal protein L19 (RPL19), were designed using the Primer Express software and published sequences.
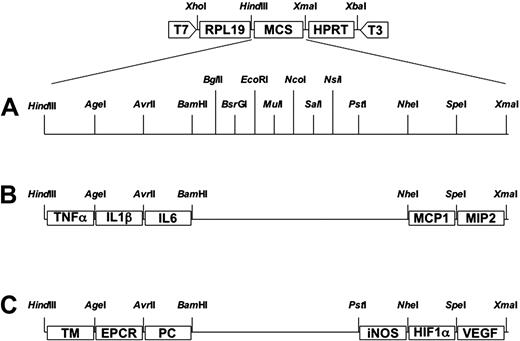
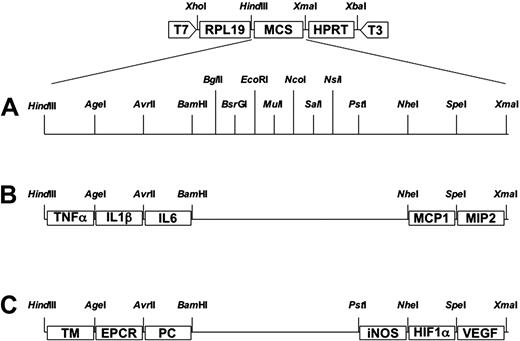
After deciding on the suitability of the primer and probe sets for each gene (Table 1), the DNA templates (pCYTO/CHEM and pPC/HYPO), used for standard curves for Q-RT-PCR, were constructed using standard molecular biology techniques. The template contained several linkers (Figure 1A), which were used to insert the short PCR amplicons (Table 1) of TNFα, IL1β, IL6, MCP-1, MIP-2, iNOS, HIF1α, and VEGF, along with similar amplicons of RPL19 and HPRT. The plasmids, pCYTO/CHEM and pPC/HYPO (Figure 1B-C), were isolated using the Plasmid Midi kit (Qiagen, Valencia, CA) and linearized with XbaI (Promega, Madison, WI). These standard RNAs for Q-RT-PCR were synthesized with the RiboMAX Large Scale RNA Production Systems-T7 kit (Promega).
Construction of the vectors pPCYTO/CHEM and pPC/HYPO. The basic vectors contain the sequences for the PCR fragments of RPL19 and HPRT between T7 and T3 RNA polymerase recognition sites that facilitate in vitro RNA synthesis bi-directionally. (A) There is a multiple cloning site (MCS) between the sequences of the housekeeping genes RPL19 and HPRT. The MCS contains several restriction enzyme recognition sites. (B) The pCYTO/CHEM plasmid contains the sequences for the PCR fragments of TNFα, IL1β, IL6, MCP-1, and MIP-2. (C) The pPC/HYPO plasmid contains the sequences for the PCR fragments of TM, EPCR, PC, iNOS, HIF1α, and VEGF.
Construction of the vectors pPCYTO/CHEM and pPC/HYPO. The basic vectors contain the sequences for the PCR fragments of RPL19 and HPRT between T7 and T3 RNA polymerase recognition sites that facilitate in vitro RNA synthesis bi-directionally. (A) There is a multiple cloning site (MCS) between the sequences of the housekeeping genes RPL19 and HPRT. The MCS contains several restriction enzyme recognition sites. (B) The pCYTO/CHEM plasmid contains the sequences for the PCR fragments of TNFα, IL1β, IL6, MCP-1, and MIP-2. (C) The pPC/HYPO plasmid contains the sequences for the PCR fragments of TM, EPCR, PC, iNOS, HIF1α, and VEGF.
Q-RT-PCR
Total RNA was isolated from various organs by the RNeasy total RNA purification kit (Qiagen). Q-RT-PCR was carried out with primers and probes listed in Table 1 for each gene using the ABI Prism 7700 Sequence Detector. Serial dilutions of the standard RNA from pCYTO/CHEM or pPC/HYPO (calculated copy numbers: 1.0 × 104 to 1.0 × 109) were used to construct standard curves for determination of tissue copy numbers of the relevant genes. The crossing point (CP) for each reaction of each gene, defined as the PCR cycle at which fluorescence begins to increase above the background and marking the beginning of the log-linear phase of the PCR reaction, was determined. A standard curve was established for each gene by plotting the CP values of serial dilutions. After that, a CP for each gene from each tissue sample (100 ng of total RNA) was determined, and the mRNA copy number was calculated from this standard curve.
Histochemistry
Hearts were obtained at various times after LPS administration, fixed with periodate-lysine-paraformaldehyde, embedded in paraffin, and sectioned at a thickness of 3 to 4 μm. The slides were stained with hematoxylin II and eosin Y (H&E) (Richard Allen Scientific, Kalamazoo, MI) for morphological analysis.
Immunohistochemistry
For immunostaining of fibrin(ogen), CD45 for common antigen of leukocytes, and neutrophils, tissue sections were deparaffinized and placed in avidin and biotin blocking solutions (Zymed Laboratories, San Francisco, CA) to eliminate endogenous avidin- or biotin-like substances, followed by Peroxo-block (Zymed Laboratories) to inhibit endogenous peroxidase activity. After the blocking steps, heat-induced antigen retrieval was accomplished in a buffer of 0.1 M citrate buffer, pH 6.0. The slides were then incubated with preimmune rabbit serum (DAKO, Carpinteria, CA) and washed.
Fibrino(gen) stains
After the blocking steps, a preimmune rabbit serum also was applied. The sections were then incubated in a goat anti–mouse fibrin(ogen) antibody (Nordic Immunology, Tillburg, The Netherlands) solution, followed by rabbit anti–goat IgG in 10% normal mouse serum. A complex of horseradish peroxidase (HRP), conjugated to a goat anti–HRP IgG (DAKO) was added. The slides were developed with 3-amino-9-ethylcarbazole (AEC) and followed with a hematoxylin QS counterstain (Vector Laboratories, Burlingame, CA).
Leukocyte stains
The primary antibody was monoclonal rat anti–mouse CD45 (Pharmingen, San Diego, CA) and the secondary antibody was biotinylated rabbit anti–rat IgG. Streptavidin-HRP was then added. The slides were developed with diaminobenzidine (DAB) and followed with hematoxylin QS counterstain.
Neutrophil stains
The primary antibody was rat anti–mouse neutrophil IgG2a (Serotec, Raleigh, NC), and the secondary antibody was HRP-conjugated goat anti–rat IgG (STAR 72; Serotec). The slides were developed with DAB and followed by hematoxylin QS counterstain.
Measurements of myoglobin and MIP-2 in plasma
Enzyme-linked immunosorbent assay (ELISA) measurements of myoglobin and MIP-2 levels in plasma were performed using mouse myoglobin ELISA kit (Life Diagnostics, West Chester, PA) and Quantikine M Immunoassay kit for MIP-2 (R&D Systems, Minneapolis, MN), respectively.
Measurement of fibrin in heart
The levels of fibrin(ogen) deposition in hearts were determined as previously reported,22 with several modifications. The hearts were dissected 48 hours after osmotic pump implantation, rinsed with isotonic saline, frozen in liquid N2, and the weight of tissue was recorded. The hearts were then thoroughly homogenized in 2-mL screw-cap tubes, containing 0.1 g of zirconia beads, in 10 mM sodium phosphate buffer (pH 7.5)/0.1 M ϵ-aminocaproic acid/5 mM EDTA/10 U/mL aprotinin/10 U/mL heparin/2 mM phenylmethylsulfonylfluoride (PMSF). The tubes were placed in an orbital tissue homogenizer (Fast Prep Bio 101; Thermo Savant, Holbrook, NY) and shaken 3 × for 30 seconds at maximum speed. The homogenate was mixed for 14 hours at 4°C and then centrifuged at times 9000g for 10 minutes. The resulting precipitate was resuspended in the same buffer without PMSF, recentrifuged, then resuspended in 3 M urea, mixed for 2 hours at 37°C, and centrifuged again at 16 000g for 15 minutes. The precipitate was dissolved in sodium dodecyl sulfate (SDS) buffer (60 mM Tris[tris(hydroxymethyl)aminomethane]-HCl, pH 6.8/10% glycerol/2% SDS/0.1 M β-mercaptoethanol 65°C, applied to a sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) gel (8%) and then transferred to a hydrophobic polyvinylidene difluride (PDVF) membrane (Hybond-P, Amersham Biosciences, Piscataway, NJ) by electroblotting. After blotting, the membrane was blocked with 5% skim milk in 20 mM Tris-HCl, pH 8.0/0.15 M NaCl/0.1% Tween 20 (TBS-T), and incubated with the same antibody used in immunohistochemistry of fibrin(ogen) at 1:1000 dilution in TBS-T, followed by an HRP anti–goat IgG (1:3000 dilution) in TBS-T. Fibrin(ogen) was visualized with an enhanced chemiluminescence-plus (ECL) system (Amersham Biosciences). Fibrin standards were prepared by clotting known amounts (0 to 5 μg/μL) of murine fibrinogen (ERL, South Bend, IN) with an excess amount of murine thrombin (ERL) in the absence of Ca2+. The intensity of each sample on the film, as evaluated with the Eagle Eye system in the densitometry mode, was converted into micrograms of fibrin(ogen) in 0.1 g of heart tissue.
Pretreatment of mice with hirudin
The contents of clinical vials of hirudin (lepirudin; Berlex, Montville, NJ) were dissolved in isotonic saline at a concentration of 12.5 μg/μL, and 100 μL of the solution was placed in the osmotic pumps (model 1003 D; Durect). The lepirudin- or saline-containing osmotic pump was implanted to peritoneal cavity, as described under “LPS challenge,” 24 hours prior to the implantation of LPS-containing pumps. The dose of lepirudin was determined by experiments in WT and EPCRδ/δ mice based on determinations of aPTT times at various dosages (2.5 μg/μL, 12.5 μg/μL, and 25 μg/μL).
Statistical analyses
Data are represented as a mean ± SEM. The survival rates were analyzed using log-rank and Wilcoxon tests. Hemodynamic parameters, levels of hemostatic factors, protein levels of fibrin, MIP-2 and myoglobin, and transcript levels of a variety of genes were analyzed using the Student t test. All analyses were performed using the computer-assisted Statview program (Abacus Concepts, Berkeley, CA), and P below .05 was considered as significant.
Results
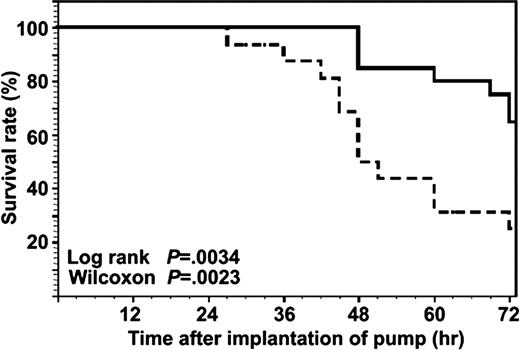
Survival rates
The survival rates were evaluated up to 72 hours after the implantation of osmotic pumps. The low EPCRδ/δ mice had significantly lower survival rates (25% at 72 hours) than WT mice (65% at 72 hours) (Figure 2).
Survival of WT and EPCRδ/δ mice after implantation of the LPS-containing osmotic pumps. The solid line indicates the survival curve of WT mice (n = 19), and the broken line depicts the survival curve of EPCRδ/δ mice (n = 16). The difference in the survival rates was compared using the log-rank and Wilcoxon tests. The P values were .0034 and .0023, respectively. Thus, there was a significant difference between the survival of WT and EPCRδ/δ mice.
Survival of WT and EPCRδ/δ mice after implantation of the LPS-containing osmotic pumps. The solid line indicates the survival curve of WT mice (n = 19), and the broken line depicts the survival curve of EPCRδ/δ mice (n = 16). The difference in the survival rates was compared using the log-rank and Wilcoxon tests. The P values were .0034 and .0023, respectively. Thus, there was a significant difference between the survival of WT and EPCRδ/δ mice.
Blood coagulation factors and platelet counts
Global coagulations assays—namely, the PT and aPTT—along with assays for specific coagulation factors—namely, FVII and FXII activities—as well as platelet counts, were measured at zero time, continuing to times of 6 hours, 24 hours, and 48 hours after pump implantation. The results obtained are summarized in Table 2. The PT values increased in both genotypes up to 48 hours after LPS treatment, indicating the presence of a coagulopathy. The PT value of EPCRδ/δ plasma at the 48-hour time point was significantly longer than that of WT mice at this time, showing a more pronounced coagulation disorder in EPCRδ/δ mice. The aPTTs of the plasmas derived from both genotypes were much more responsive to LPS than the PT values, and the increases in aPTTs were more pronounced in EPCRδ/δ mouse plasmas. The FVII activities of these latter mice slightly decreased subsequent to LPS administration in both genotypes, and there was no significant difference between both groups at each time point. FXII activities decreased rapidly after pump implantation, and these values from EPCRδ/δ plasmas were significantly lower than those from WT plasmas at 24 hours and 48 hours after LPS, thus supporting the dramatic effects of LPS exposure on the aPTT values. The number of platelets was lower at 6 hours in both of groups of mice, with EPCRδ/δ mice displaying a more significant decrease at 24 hours and 48 hours.
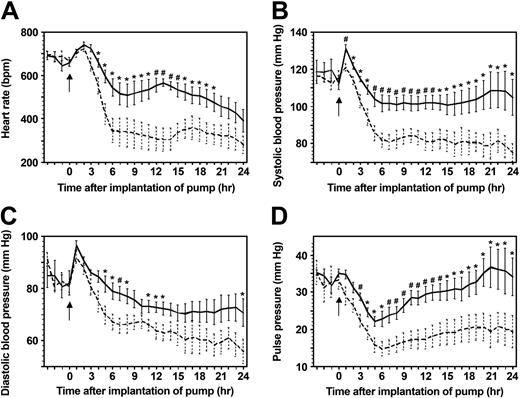
HRs and BPs
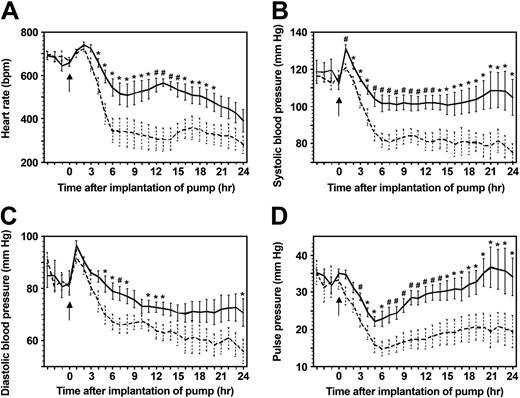
The HRs of both genotypes increased slightly from 0 to 2 hours after LPS treatment in this model. After this time, the HRs of WT mice further decreased slightly from 2 hours to 6 hours, to about 600 bpm. On the other hand, the decline of HRs in EPCRδ/δ mice was much steeper during this same time period and reached a lower limit of approximately 300 bpm. This difference was statistically significant between 4 hours and 21 hours (Figure 3A). The systolic BPs showed similar patterns (Figure 3B). Interestingly, the pulse pressures (PPs) of both genotypes diminished between 0 and 6 hours, but after this period, the PPs of WT mice recovered. Those same values of EPCRδ/δ mice remained low (Figure 3D).
Continuous HRs and BPs of mice after LPS administration. In all panels, the solid line indicates WT mice (n = 10), and the broken line represents EPCRδ/δ mice (n = 8). The arrow indicates the time of the implantation of the osmotic pumps. The statistical difference was indicated as * or #, P < .05 or P < .01, respectively. (A) HR in beats/minute (bpm); (B) systolic BP in mmHg; (C) diastolic BP in mmHg; and (D) pulse pressures in mmHg. Error bars indicate SEM.
Continuous HRs and BPs of mice after LPS administration. In all panels, the solid line indicates WT mice (n = 10), and the broken line represents EPCRδ/δ mice (n = 8). The arrow indicates the time of the implantation of the osmotic pumps. The statistical difference was indicated as * or #, P < .05 or P < .01, respectively. (A) HR in beats/minute (bpm); (B) systolic BP in mmHg; (C) diastolic BP in mmHg; and (D) pulse pressures in mmHg. Error bars indicate SEM.
Plasma levels of myoglobin and MIP2
Plasma myoglobin levels represent an early marker of heart muscle damage. The concentrations of this protein in both genotypes were not changed at 6 hours after implantation of the pump. These values increased at 24 hours in both groups, and those of EPCRδ/δ mice were significantly higher than those of WT mice (Table 3). MIP-2 plasma levels also greatly increased by at least 1000-fold in both genotypes at 6 hours after pump placement and were significantly higher (approximately 1.6-fold) in EPCRδ/δ mice than in WT mice at this time period (Table 3). At 24 hours, these values decreased by approximately 10-fold from their 6-hour levels and tended to remain slightly higher for EPCRδ/δ mice.
mRNA levels of inflammatory marker expression in the heart
mRNA expression levels in the heart of a variety of proinflammatory cytokines and chemokines, including TNFα, IL1β, IL6, and MCP-1, are up-regulated after LPS administration in this model, but the responses are the same in the 2 genotypes. The expression level of HIF1α was significantly higher in EPCRδ/δ mice than in WT mice at 3 hours after LPS (Table 4). In addition, there were no significant differences between the genotypes in expression in heart of iNOS and VEGF mRNA (Table 4). On the other hand, expression of MIP-2 mRNA in heart was significantly up-regulated in EPCRδ/δ mice as compared to WT mice (Table 4), and this could serve as the basis of the more pronounced leukocyte invasion of the hearts in EPCRδ/δ mice.
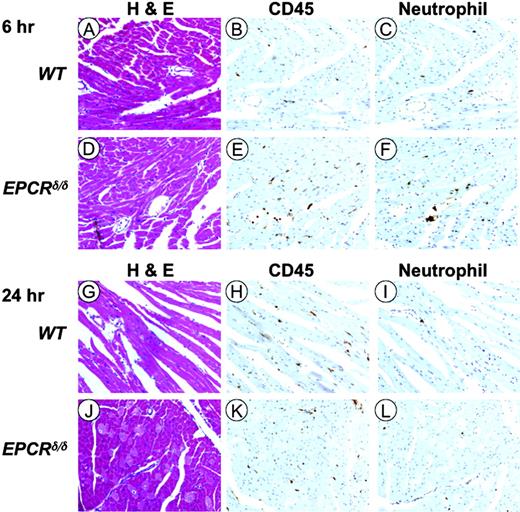
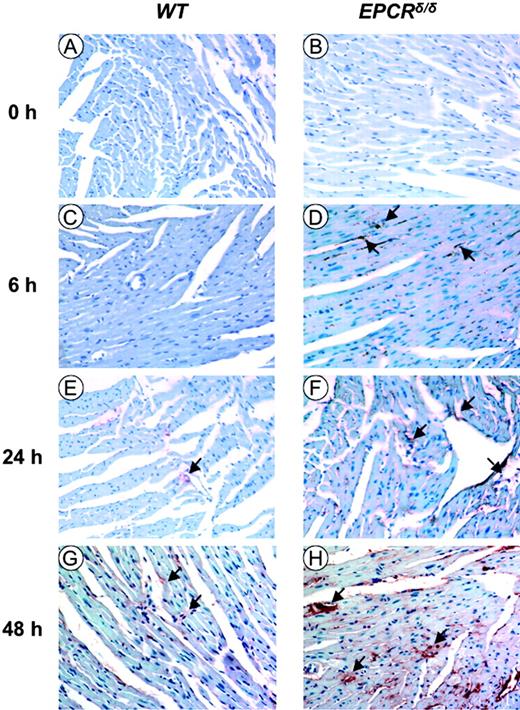
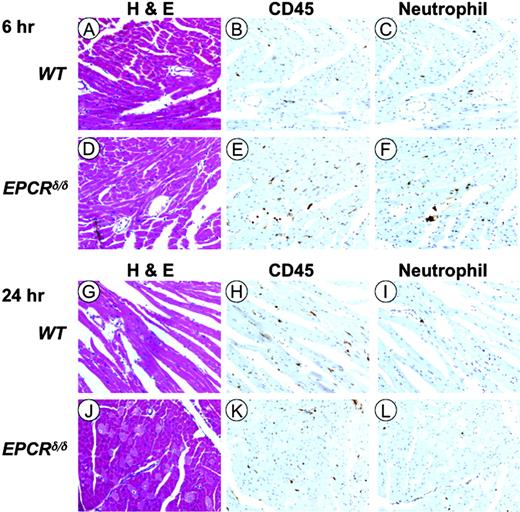
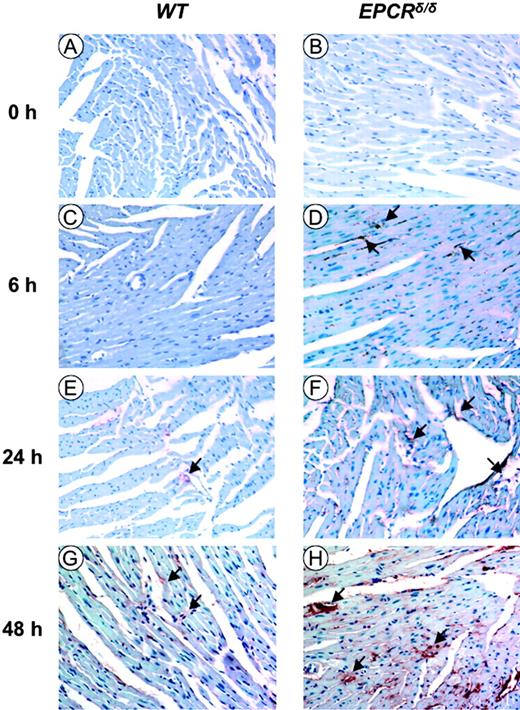
Cardiac histopathology of LPS-treated mice
H&E staining of heart sections at 6 hours and 24 hours after LPS (Figure 4A,D,G,J) revealed muscular degradation in EPCRδ/δ mice (Figure 4D,J) as compared to WT mice at those same time points (Figure 4A,G). The migration of CD45+ cells at 6 hours in the heart was observed in both genotypes; however, the positive stains were more dominant in EPCRδ/δ mice than in WT mice (Figures 4B,E). Furthermore, neutrophil stains were associated with CD45+ stains (Figure 4C,F). CD45 (Figure 4H) and neutrophil (Figure 4I) stains in WT mice at 24 hours were more intense than those at 6 hours (Figure 4B-C). In contrast, those same stains in EPCRδ/δ mice at 24 hours (Figure 4K-L) appear less intense than at 6 hours (Figure 4E-F). Fibrin deposition in EPCRδ/δ mice at 6, 24, and 48 hours was more pronounced than in WT mice at all time points (Figure 5), and quantitative measurements of fibrin in heart tissue present in 48 hours after pump implantation was 0.628 ± 0.081 and 1.20 ± 0.24 (P = .04) for WT and EPCRδ/δ mice, respectively. Fibrin was undetectable in hearts in experiments with mice dosed similarly with saline.
Histochemical and immunohistochemical analysis of murine cardiac tissue after LPS administration. H&E staining of WT (A) and EPCRδ/δ (D) mouse heart sections 6 hours after LPS administration. (B,E) Anti-CD45 immunostaining of serial heart sections of WT and EPCRδ/δ mice, respectively, 6 hours after LPS administration. (C,F) Antineutrophil protein immunostaining of serial heart sections of WT and EPCRδ/δ mice, respectively, 6 hours after LPS administration. (G-L) Similar H&E (G,J), anti-CD45 (H,K), and antineutrophil protein (I,L) staining and immunostaining of WT and EPCRδ/δ mice, respectively, at 24 hours after LPS treatment. A Nikon Eclipse E600 light microscope (Nikon, Melville, NY) with a Nikon Plan Fluor objective (magnification, × 20; numerical aperture, 0.5). Images were captured with a SPOT 2 slider (model 1.4.0) camera (Diagnostic Instruments, Sterling Heights, MI) using SPOT software. The images were transferred to Adobe Photoshop 7.0 (Adobe, San Jose, CA) for final reproduction.
Histochemical and immunohistochemical analysis of murine cardiac tissue after LPS administration. H&E staining of WT (A) and EPCRδ/δ (D) mouse heart sections 6 hours after LPS administration. (B,E) Anti-CD45 immunostaining of serial heart sections of WT and EPCRδ/δ mice, respectively, 6 hours after LPS administration. (C,F) Antineutrophil protein immunostaining of serial heart sections of WT and EPCRδ/δ mice, respectively, 6 hours after LPS administration. (G-L) Similar H&E (G,J), anti-CD45 (H,K), and antineutrophil protein (I,L) staining and immunostaining of WT and EPCRδ/δ mice, respectively, at 24 hours after LPS treatment. A Nikon Eclipse E600 light microscope (Nikon, Melville, NY) with a Nikon Plan Fluor objective (magnification, × 20; numerical aperture, 0.5). Images were captured with a SPOT 2 slider (model 1.4.0) camera (Diagnostic Instruments, Sterling Heights, MI) using SPOT software. The images were transferred to Adobe Photoshop 7.0 (Adobe, San Jose, CA) for final reproduction.
Antifibrin(ogen) immunostaining of heart sections at various times after LPS administration for WT and EPCRδ/δ mice, respectively. (A-B) WT and EPCRδ/δ control heart tissue (time = 0), respectively; (C-D), WT and EPCRδ/δ heart tissue, respectively, at 6 hours after LPS; (E-F), WT and EPCRδ/δ heart tissue, respectively, at 24 hours after LPS; (G-H), WT and EPCRδ/δ mice, respectively, at 48 hours after LPS. Microscopy was performed as described in Figure 4.
Antifibrin(ogen) immunostaining of heart sections at various times after LPS administration for WT and EPCRδ/δ mice, respectively. (A-B) WT and EPCRδ/δ control heart tissue (time = 0), respectively; (C-D), WT and EPCRδ/δ heart tissue, respectively, at 6 hours after LPS; (E-F), WT and EPCRδ/δ heart tissue, respectively, at 24 hours after LPS; (G-H), WT and EPCRδ/δ mice, respectively, at 48 hours after LPS. Microscopy was performed as described in Figure 4.
Effects of hirudin administration
It has been reported previously that administration of hirudin led to improvement in survival of LPS-treated mice, reduced the levels of the thrombin-antithrombin complex (TAT), and attenuated fibrin deposition in livers. However, LPS-stimulated TNFα and IL6 levels were not diminished.23 We expanded this experiment to show that under conditions wherein sufficient hirudin is present to maintain aPTT times at 2.5 times those of saline-treated EPCRδ/δ mice, LPS-stimulated BP and HR decreases are not affected, suggesting that thrombin plays a minimal role in the hemodynamic effects observed in this model.
Discussion
Because of the emergence of PC as a potential drug for treatment of severe sepsis, all components of the PC pathway are under increased scrutiny regarding their contributions to the in vivo roles of PC and aPC in acute and chronic inflammatory disease. Thus, using our low EPCR-expressing mice (< 10% of WT EPCR expression in all organs tested), which have been generated by targeted disruption of the EPCR promoter region,21 we have studied herein the effects of an EPCR deficiency on the response of mice to an acute inflammatory LPS challenge. Since mice with a total deficiency of EPCR are not embryonically viable,24 generation of these very low-expressing EPCR mice allowed for their normal development and survival and provided a means to study the susceptibility to inflammation of mice with a severe EPCR deficiency.
In order to mimic the conditions of endotoxin shock more closely than the usual bolus LPS injection methods, we used a continual intraperitoneal exposure model in mice with the aid of osmotic pumps, similar to models that have been used in rats.25 Using this model, we find that low EPCR-expressing mice die significantly more rapidly, when compared to WT mice, in response to LPS administration. This is coupled with a significantly more rapid entrance into endotoxin shock of EPCRδ/δ mice, compared to WT mice. The participation of the PC system in in vivo hemodynamic properties of the organism has been observed from the viewpoint of administration of aPC as a preventive measure against LPS-induced hypotension,5 but we have taken an opposite approach and have shown previously and herein that low PC and EPCR mice display enhanced polymicrobial sepsis-,26 and now LPS-, induced hypotension. The correlation of both of these approaches suggests that aPC, via an EPCR-mediated effect(s), is mechanistically involved, perhaps through attenuation of iNOS production,5 in regulation of hemodynamics of the mouse and that acute inflammation disrupts its homeostasis, directly or indirectly, through aPC-induced signaling.
Global measures of coagulation, for example, the PTs and aPTTs, are temporally increased subsequent to LPS administration in WT mice in this model but are more prolonged at later times in low EPCR mice than in WT mice after LPS administration. Platelet counts are more diminished in the former mice under these same conditions. The platelet counts tend to be lower even prior to LPS administration in EPCRδ/δ mice and remain so during the entire course of treatment with LPS. Thus, this model of continuous LPS administration results in a gradual coagulopathy that is enhanced by an EPCR insufficiency, most likely via an induced aPC deficiency and consequent lack of control of FVa and FVIIIa activities. The drop in FXII plasma levels certainly contributes to the prolongation of the aPTT activities, which approach approximately 17% of WT FXII levels in low EPCR mice at 48 hours after LPS, a value nearly one half of the FXII concentration for treated WT mice at that same time point. Thus, it is clear that a coagulation disorder is induced by LPS and that EPCR plays a role in protection of the organism against possible disseminated intravascular coagulation (DIC) when an endotoxin challenge is present. As we have observed in a cecal ligation and puncture model of polymicrobial sepsis, fibrinogen levels substantially rise during these types of acute inflammatory challenges,26 also possibly contributing to a prothrombotic state in the absence of consumption of coagulation proteins. These consistent increases of the fibrinogen levels in different models of sepsis and endotoxemia are most likely an acute phase response, resulting from the inflammatory challenge.
Microscopic examination of organs in response to continuous LPS administration revealed that dramatic changes occurred in the heart. Myoglobin plasma levels rise more dramatically in low EPCR mice than in WT mice at 24 hours after LPS, indicative of more severe heart damage in the EPCRδ/δ mice. This is supported by histochemical evidence, wherein a more serious degradation of heart tissue is noted in EPCRδ/δ mice, compared with WT mice, and leukocyte/neutrophil invasion of heart tissue at early times (6 hours) after LPS administration is more advanced in low EPCR mice. While a number of inflammatory mediators are up-regulated in this model in both genotypes, of the cytokines/chemokines examined, MIP-2 expression levels in the heart were significantly more elevated at early times in EPCRδ/δ mice compared with their WT counterparts. MIP-2, which is directly expressed by cardiac myocytes in response to LPS, may attract neutrophils to cardiac tissue,27 and this investigation now links the more serious heart abnormalities found in low EPCR mice with enhanced MIP-2 gene expression in heart tissue.
At later time points (48 hours), comparatively more enhanced fibrin deposition occurs in low EPCR murine hearts, showing that EPCR is involved in preventing late-stage thromboses during an acute inflammatory challenge. Since thrombosis is not seen in the heart at early times after challenge, the heart damage observed during endotoxemia is likely due more to inflammatory damage, rather than consequences of thrombosis, although it is possible that microthrombi, below the detection levels of the assays, could conceivably establish an ischemic state, resulting in cardiac defects.
In conclusion, this study provides evidence that EPCR offers protection against death following administration of lethal levels of LPS in mice. This may be due to the involvement of EPCR in regulating hemodynamic properties, along with moderating the MIP-2–mediated inflammatory response. In addition, it has recently been reported that aPC induces EC proliferation via an EPCR and PAR-1–dependent mechanism, possibly offering another rationale for vascular protection in heart tissue.28 Lastly, diminished EPCR may exacerbate later-stage thrombosis in the heart. The similarities between aPC and EPCR in these responses strongly suggest that aPC likely functions via EPCR in attenuating the response of the organism to acute inflammation.
Prepublished online as Blood First Edition Paper, November 4, 2004; DOI 10.1182/blood-2004-06-2456.
Supported by grants HL19982 and HL73750 (F.J.C.) from the National Institutes of Health and the Kleiderer-Pezold endowed professorship (F.J.C.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Ms Stacy Raje and Ms Angelik Anderson for maintenance of the mouse colonies, Ms Mayra Sandoval-Cooper for assisting with the histology, and Ms Deborah Donahue for implanting BP modules into the mice.