Abstract
Deficiency of methylenetetrahydrofolate reductase (MTHFR) predisposes to hyperhomocysteinemia and vascular disease. We tested the hypothesis that heterozygous disruption of the Mthfr gene sensitizes mice to diet-induced hyperhomocysteinemia and endothelial dysfunction. Mthfr+/- and Mthfr+/+ mice were fed 1 of 4 diets: control, high methionine (HM), low folate (LF), or high methionine/low folate (HM/LF). Plasma total homocysteine (tHcy) was higher with the LF and HM/LF diets than the control (P < .01) or HM (P < .05) diets, and Mthfr+/- mice had higher tHcy than Mthfr+/+ mice (P < .05). With the control diet, the S-adenosylmethionine (SAM) to S-adenosylhomocysteine (SAH) ratio was lower in the liver and brain of Mthfr+/- mice than Mthfr+/+ mice (P < .05). SAM/SAH ratios decreased further in Mthfr+/+ or Mthfr+/- mice fed LF or LF/HM diets (P < .05). In cerebral arterioles, endothelium-dependent dilation to 1 or 10 μM acetylcholine was markedly and selectively impaired with the HM/LF diet compared with the control diet for both Mthfr+/+ (maximum dilation 5% ± 2% versus 21% ± 4%; P < .01) and Mthfr+/- (6% ± 2% versus 21% ± 3%; P < .01) mice. These findings demonstrate that the Mthfr+/- genotype sensitizes mice to diet-induced hyperhomocysteinemia and that hyperhomocysteinemia alters tissue methylation capacity and impairs endothelial function in cerebral microvessels.
Introduction
Elevation of plasma total homocysteine (tHcy) is associated with increased risk of stroke, myocardial infarction, and venous thrombosis.1,2 In a recent meta-analysis, a 25% elevation in plasma tHcy was associated with a 10% higher risk of cardiovascular disease and a 20% higher risk of stroke after adjustment for other known risk factors.3 The vascular pathogenic effects of homocysteine have not been fully characterized but are thought to involve oxidative inactivation of endothelium-derived nitric oxide and vascular inflammation.4-6 Impaired endothelium-dependent vasodilation has been observed in human subjects with acute hyperhomocysteinemia induced by oral methionine loading7-11 and animal models of diet-induced chronic hyperhomocysteinemia.12,13 Mice with hyperhomocysteinemia produced by heterozygosity for a targeted disruption of the cystathionine β-synthase (Cbs) gene have enhanced sensitivity to endothelial dysfunction in both the aorta14-16 and mesenteric arterioles.14,17
Some pathogenic effects of hyperhomocysteinemia may be related to the metabolic link between homocysteine and methionine. Within the methionine cycle, methionine is converted to S-adenosylmethionine (SAM), which serves as a methyl donor for numerous methyl acceptors, including DNA, RNA, protein, histones, neurotransmitters, and phospholipids.18 S-adenosylhomocysteine (SAH) is produced as a by-product of methyl donation, and homocysteine is formed through the (reversible) liberation of adenosine from SAH. During hyperhomocysteinemia, intracellular concentrations of SAH may increase, resulting in a lower SAM/SAH ratio and diminished methylation capacity.16,19 These metabolic effects of hyperhomocysteinemia potentially could contribute to vascular pathology, because hypomethylation of DNA has been detected in peripheral blood mononuclear cells of humans with hyperhomocysteinemia19,20 and altered DNAmethylation has been implicated as a cause of deregulated gene expression in atherosclerosis.21,22
Methylenetetrahydrofolate reductase (MTHFR) plays an integral role in the methionine cycle by supplying 5-methyltetrahydrofolate for the remethylation of homocysteine to methionine.18 A common polymorphism in the MTHFR gene, 677C>T, produces deficient MTHFR activity and is associated with hyperhomocysteinemia and increased risk of coronary heart disease, especially under conditions of compromised folate status.23-25 Mice that are heterozygous for a targeted disruption of the Mthfr gene have mild hyperhomocysteinemia and decreased SAM/SAH ratios in the liver and brain.26 Like Cbs+/- mice, Mthfr+/- mice have impaired endothelium-dependent vasomotor responses in mesenteric arterioles.27 It is not known if Mthfr+/- mice have vascular dysfunction in nonmesenteric vessels. It also is not known whether the effects of the Mthfr+/- genotype on hyperhomocysteinemia and methylation capacity are dependent on folate or other dietary factors or whether these metabolic abnormalities are related to the vascular phenotype.
The goal of the present study was to test the hypothesis that Mthfr+/- mice have enhanced sensitivity to diet-induced hyperhomocysteinemia, decreased methylation capacity, DNA hypomethylation, and endothelial dysfunction in the aorta and cerebral arterioles. Our results demonstrate that the Mthfr+/- genotype sensitizes mice to diet-induced hyperhomocysteinemia but that effects of hyperhomocysteinemia on endothelial dysfunction in cerebral arterioles are mediated primarily by diet rather than Mthfr genotype.
Materials and methods
Mice and experimental protocol
Mice heterozygous for disruption of the Mthfr gene,26 from 7 generations of backcrosses to BALB/c mice, and their wild-type littermates were used in the study. Mthfr genotype was determined by polymerase chain reaction (PCR) as described previously.26 At weaning, Mthfr+/- and Mthfr+/+ mice were randomly assigned to receive 1 of 4 diets (Table 1): control (LM 485; Harlan Teklad, Madison, WI); high methionine (HM) (control diet plus 0.5% l-methionine in drinking water); low folate (LF) (TD 00204; Harlan Teklad); and high methionine/low folate (HM/LF) (TD 00205; Harlan Teklad). All diets contained adequate levels of all nutrients, except for folate in the LF and HM/LF diets, for mice as recommended by the National Research Council.28 Mice were maintained on the diets for 7 to 15 weeks. We initially examined separate groups of mice that were fed the experimental diets for 7 weeks or 15 weeks. We found no differences in tHcy, SAM, SAH, or relaxation responses between the 2 groups, so we chose to include all mice that were fed the diets for 7 to 15 weeks in the overall analysis. At the end of the feeding period, mice were anesthetized with sodium pentobarbital (150 mg/kg intraperitoneally), and blood was collected by cardiac puncture into EDTA (ethylenediaminetetraacetic acid) (final concentration 5 mM). Samples of liver and brain were immediately deproteinized in ice-cold 0.4 M perchloric acid, homogenized, and centrifuged. The supernatant fraction was immediately frozen and stored at -80°C for later analysis for SAM and SAH. Additional samples of liver and brain were directly frozen and stored at -80°C for later extraction of genomic DNA for methylation analysis. The aorta was removed and used immediately for vasomotor studies. A second group of mice was fed either control or HM/LF diets for 25 to 40 weeks and then used for studies of vasomotor responses in cerebral arterioles. The protocol was approved by the University of Iowa and Veterans Affairs Animal Care and Use Committees.
Responses in aortic rings
Relaxation of precontracted aortic rings was measured in vitro as described previously.15,16 After removal of loose connective tissue, the proximal aorta was cut into multiple 3 to 4 mm rings and suspended in an organ chamber containing oxygenated Krebs buffer maintained at 37°C. Rings were precontracted submaximally using the thromboxane analog U46619, and relaxation dose-response curves were generated by cumulative addition of the endothelium-dependent vasodilator, acetylcholine (10-8 to 10-5 M), or the endothelium-independent vasodilator, sodium nitroprusside (10-8 to 10-5 M).
Responses in cerebral arterioles
Dilation of cerebral arterioles was measured as described previously.29 Briefly, mice were anesthetized and ventilated mechanically with room air and supplemental oxygen, a cranial window was made over the left parietal cortex, and a segment of a randomly selected pial arteriole (about 30 μm in diameter) was exposed. The diameter of the cerebral arteriole was measured, using a videomicroscope coupled to an image-shearing device, under control conditions and during superfusion with acetylcholine (1 and 10 μM) and nitroprusside (0.1 and 1 μM).
Biochemical assays
Plasma tHcy, defined as the total concentration of homocysteine after quantitative reductive cleavage of all disulfide bonds,30 was determined by high-performance liquid chromatography using electrochemical detection as described previously.31 SAM and SAH concentrations in liver and brain were determined by high-performance liquid chromatography using UV detection as described previously.32
DNA hypomethylation
Genomic DNA was extracted from liver and brain using the DNeasy kit (Qiagen, Valencia, CA). Global DNA hypomethylation was determined using a cytosine extension assay33 in which genomic DNA is digested with HpaII (New England Biolabs, Beverly, MA), a methylation-sensitive restriction enzyme, followed by single nucleotide extension with [3H] deoxycytidine triphosphate ([3H]dCTP) (Perkin-Elmer, Boston, MA). Undigested samples served as background controls. Samples were also digested with MspI (New England Biolabs), an isoschizomer of HpaII that is not sensitive to methylation, to verify that the incorporation of tritium was greater than with HpaII-digested samples.
Statistical analysis
Two-way analysis of variance (ANOVA), followed by the Fisher least significant difference (LSD) test for pair-wise comparisons, was used to analyze the effects of Mthfr genotype and diet on plasma tHcy; liver and brain SAM, SAH, and SAM/SAH ratios; and global DNA hypomethylation. Responses to vasodilators in aorta were analyzed by 2-way repeated measures ANOVA with the Tukey post hoc test for multiple comparisons. This analysis was accomplished by SigmaStat version 3.0 (SPSS, Chicago, IL).
Results
Plasma tHcy
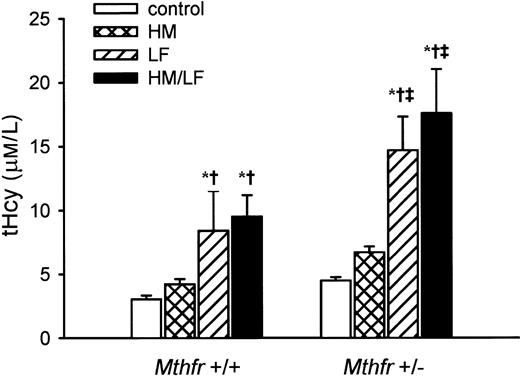
The LF and HM/LF diets produced higher levels of plasma tHcy than the control or HM diets (P < .01 and P < .05, respectively) in both Mthfr+/- and Mthfr+/+ mice (Figure 1). The effect of diet was more pronounced in Mthfr+/- mice, with the LF and HM/LF diets raising plasma tHcy to 14.7 ± 2.6 μM and 17.6 ± 3.5 μM, respectively, compared with 8.4 ± 3.1 and 9.5 ± 1.7 μM, respectively, in Mthfr+/+ mice. The overall effect of Mthfr genotype on plasma tHcy was highly significant (P < .01).
Plasma concentration of total homocysteine (tHcy). Values are mean ± SEM. *Significantly different than mice of the same genotype fed control diet (P < .01). †Significantly different than mice of the same genotype fed HM diet (P < .05). ‡Significantly different than Mthfr+/+ mice fed the same diet (P < .01).
Plasma concentration of total homocysteine (tHcy). Values are mean ± SEM. *Significantly different than mice of the same genotype fed control diet (P < .01). †Significantly different than mice of the same genotype fed HM diet (P < .05). ‡Significantly different than Mthfr+/+ mice fed the same diet (P < .01).
Hepatic SAM, SAH, and DNA hypomethylation
Mice fed the LF or HM/LF diets had lower hepatic SAM levels and lower hepatic SAM/SAH ratios than mice fed the control diet for both Mthfr+/+ and Mthfr+/- genotypes (P < .05) (Table 2). Hepatic SAM/SAH ratios also were lower in Mthfr+/+ or Mthfr+/- mice fed the HM diet than in mice of the same genotype fed the control diet (P < .05), but this effect was largely due to increased SAH rather than decreased SAM. A significant effect of Mthfr genotype was observed only for the control diet, with which Mthfr+/- mice had lower hepatic SAM levels (P < .05) and a lower SAM/SAH ratio (P < .05) than Mthfr+/+ mice. No significant differences in hepatic global DNA hypomethylation were observed between diets or Mthfr genotypes (Table 2).
Brain SAM, SAH, and DNA hypomethylation
Mice fed the LF or HM/LF diets had higher brain SAH levels and lower brain SAM/SAH ratios than mice fed the control diet for both Mthfr+/+ and Mthfr+/- genotypes (P < .05) (Table 3). Compared with the control diet, the HM diet also produced higher brain SAH levels and lower brain SAM/SAH ratios in Mthfr+/+ mice (P < .05) but not in Mthfr+/- mice. A significant effect of Mthfr genotype was observed in mice fed the control diet, with higher brain SAH levels and lower SAM/SAH ratios in Mthfr+/- mice than in Mthfr+/+ mice (P < .05). No significant effects of diet on global DNA hypomethylation in brain were observed for Mthfr+/+ mice (Table 3), but increased DNA hypomethylation was observed in Mthfr+/- mice fed the HM diet (P < .05 versus Mthfr+/+ mice).
Vasomotor responses
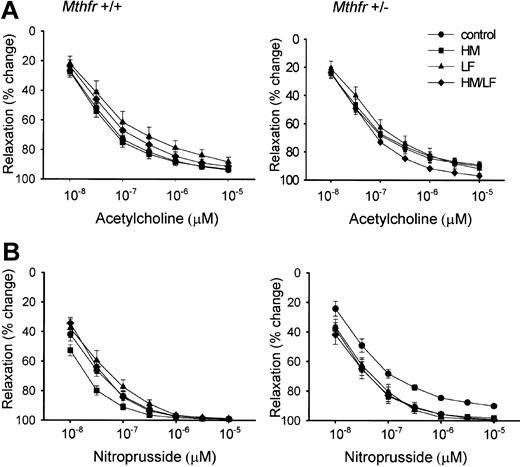
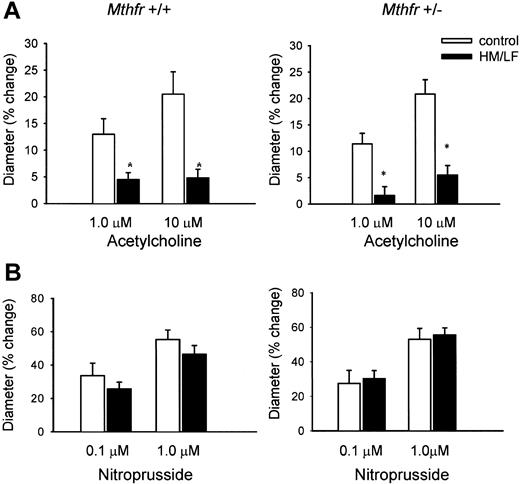
Concentration-dependent relaxation of aortic rings to the endothelium-dependent vasodilator, acetylcholine, was similar in Mthfr+/+ and Mthfr+/- mice, regardless of diet (Figure 2A). Similarly, no significant effects of Mthfr genotype or diet were observed for relaxation of aortic rings to the endothelium-independent vasodilator, nitroprusside (Figure 2B). To determine the effects of Mthfr genotype and diet on responses in the cerebral circulation, Mthfr+/+ and Mthfr+/- mice were fed either control or HM/LF diets and dilation of cerebral arterioles to acetylcholine or nitroprusside was measured by videomicroscopy in vivo. With the control diet, Mthfr+/+ and Mthfr+/- mice exhibited similar, dose-dependent, dilation of cerebral arterioles to acetylcholine (Figure 3A). Dilation responses to acetylcholine were significantly impaired in mice fed the HM/LF diet compared with mice fed the control diet for both the Mthfr+/- and Mthfr+/+ genotypes (P < .05). Concentration-dependent dilation of cerebral arterioles to nitroprusside was not affected by Mthfr genotype or diet (Figure 3B).
Relaxation responses of aortic rings. Relaxation responses of aortic rings were measured in response to acetylcholine (A) or nitroprusside (B). No significant effects of diet on responses to acetylcholine or nitroprusside were observed for Mthfr+/+ or Mthfr+/- mice. Error bars indicate means ± SEM.
Relaxation responses of aortic rings. Relaxation responses of aortic rings were measured in response to acetylcholine (A) or nitroprusside (B). No significant effects of diet on responses to acetylcholine or nitroprusside were observed for Mthfr+/+ or Mthfr+/- mice. Error bars indicate means ± SEM.
Dilation of cerebral arterioles. Dilation of cerebral arterioles was measured in response to (A) 1.0 μM and 10 μM acetylcholine or (B) 0.1 μM and 1.0 μM nitroprusside. *Significantly different than mice fed control diet (P < .001). Error bars indicate means ± SEM.
Dilation of cerebral arterioles. Dilation of cerebral arterioles was measured in response to (A) 1.0 μM and 10 μM acetylcholine or (B) 0.1 μM and 1.0 μM nitroprusside. *Significantly different than mice fed control diet (P < .001). Error bars indicate means ± SEM.
Discussion
The work reported here sought to determine if a genetic defect in the homocysteine remethylation pathway (heterozygosity for a targeted defect in the Mthfr gene) sensitizes mice to diet-induced hyperhomocysteinemia and endothelial dysfunction. There are 3 major findings of this study. First, Mthfr+/- mice have markedly enhanced sensitivity to hyperhomocysteinemia induced by dietary folate deficiency but are relatively insensitive to excess dietary methionine. Second, diet-induced hyperhomocysteinemia is associated with decreased tissue methylation capacity, exemplified by decreased tissue SAM/SAH ratios, in both Mthfr+/- and Mthfr+/+ mice. In the liver, this effect is primarily mediated by a decrease in SAM, whereas in brain it is mediated by an increase in SAH. Third, diet-induced hyperhomocysteinemia produces selective impairment of endothelium-dependent dilation of cerebral arterioles in both Mthfr+/- and Mthfr+/+ mice.
The enhanced sensitivity of Mthfr+/- mice to hyperhomocysteinemia induced by dietary folate deficiency is in accordance with observations in human subjects who are homozygous for the MTHFR 677C>T allele.24 The lack of a significant hyperhomocysteinemic effect of excess dietary methionine in Mthfr+/- mice also fits well with previous observations in which human subjects with the MTHFR 677TT and MTHFR 677CC genotypes responded similarly to methionine loading despite higher fasting levels of plasma tHcy in MTHFR 677TT subjects.34 In this regard, the effects of MTHFR deficiency contrast with those of CBS deficiency, in which there is increased sensitivity to hyperhomocysteinemia induced by excess dietary methionine in human subjects35 and mice.16
We found that the effect of Mthfr genotype on methylation capacity was tissue specific and highly dependent on diet. With the control diet, Mthfr+/- mice had lower SAM/SAH ratios than Mthfr+/+ mice in both liver and brain. These findings are similar to those reported previously for Mthfr+/+ and Mthfr+/- mice fed a different standard rodent chow.26 With the LF or HM/LF diets, we observed further decreases in hepatic SAM levels and SAM/SAH ratios in both Mthfr+/+ and Mthfr+/- mice. These findings are consistent with previous findings of decreased hepatic levels of SAM in animals maintained on folate-deficient diets.36 Interestingly, the effects of the folate-deficient diets on hepatic SAM and SAM/SAH ratios were nearly identical in Mthfr+/+ and Mthfr+/- mice (Table 2) despite higher levels of plasma tHcy in Mthfr+/- mice (Figure 1). These observations suggest that hepatic methylation capacity may be influenced not only by remethylation of homocysteine to methionine but perhaps also by other folate-dependent factors. Alternatively, the contrasting effects of Mthfr genotype on plasma tHcy and hepatic SAM may reflect a substantial nonhepatic source of plasma tHcy in these mice.
The folate-deficient diets also decreased SAM/SAH ratios in the brain, and, as in the liver, this effect was independent of Mthfr genotype (Table 3). In contrast to the liver, however, the decreased SAM/SAH ratios in the brain of mice fed folate-deficient diets resulted primarily from higher levels of SAH rather than lower levels of SAM. The greater effect of folate deficiency on SAH in brain compared with liver may be due to the absence of betainehomocysteine methyltransferase in the brain; tissue-specific differences in other methionine cycle enzymes such as CBS, SAH hydrolase, or methionine adenosyltransferase; or differences in the relative activities of SAM-dependent methyltransferases.18 Overall, these findings demonstrate that diet-induced hyperhomocysteinemia decreases methylation capacity in both liver and brain but through distinct mechanisms. The low-folate diets decreased the SAM/SAH ratio by a greater factor in the liver (about 4-fold) than in the brain (about 2.5-fold), but there was a greater relative increase in SAH in the brain. These observations suggest that the low-folate diets may have a more profound inhibitory influence on methylation reactions in the brain than in the liver, because elevation of SAH is more indicative of inhibition of methylation reactions than decreased SAM/SAH ratio.19
Cerebral arterioles of Mthfr+/+ or Mthfr+/- mice fed the HM/LF diet had markedly impaired responses to the endothelium-dependent vasodilator, acetylcholine (Figure 3). Responses to the endothelium-independent vasodilator, nitroprusside, were unaffected by the HM/LF diet or Mthfr genotype. This selective attenuation of endothelium-dependent responses is consistent with a previous study in which superfusion of the rat parietal cortex with a relatively high concentration (1 mM) of homocysteine decreased cerebral blood flow and attenuated responses to endothelium-dependent vasodilators.37 It is intriguing that the effect of the HM/LF diet on endothelial function, like its effect on tissue methylation capacity but unlike its effect on plasma tHcy, was independent of Mthfr genotype. These observations raise the possibility that the vascular effects of hyperhomocysteinemia may be related to altered methylation rather to a direct effect of homocysteine. To begin to explore this possibility, we measured global DNA hypomethylation in the liver and brain. Surprisingly, despite large changes in hepatic SAM/SAH ratio, no significant changes in hepatic global DNA hypomethylation were observed for diet or Mthfr genotype (Table 2). Similarly, no major effects of diet on global DNA hypomethylation were observed in the brain, although Mthfr+/- mice fed the HM diet had modestly increased DNA hypomethylation (Table 3). Effects of altered methylation on vascular function are likely to be mediated through changes in methylation patterns of specific genes21,22 rather than changes in global DNA methylation, which is a general measure of maintenance methylation of epigenetically regulated genes.38 Future progress in this area, therefore, will require the analysis of vascular gene-specific methylation patterns in animal models of hyperhomocysteinemia.
We observed no effect of Mthfr genotype or diet on vasomotor responses to acetylcholine or nitroprusside in aortic rings (Figure 2). This lack of endothelial dysfunction in the aorta contrasts with our previous findings in CBS-deficient mice with diet-induced hyperhomocysteinemia.15,16 We suspect that this disparity may be related to the lower levels of plasma tHcy in the current study (up to 17 μM in Mthfr+/- mice fed the HM/LF diet) compared with previous studies (about 25 μMin Cbs+/- mice fed high-methionine or low-folate diets). Therefore, the levels of plasma tHcy observed in the current study may not have been high enough to produce impaired endothelial function in the aorta. Alternatively, the different genetic backgrounds of the mice in the current study (BALB/c) and those studied previously (C57BL/6J) may have contributed to differences in vasomotor responses. Nevertheless, the current findings clearly demonstrate that cerebral arterioles are highly sensitive, whereas aortic rings are relatively insensitive, to endothelial dysfunction caused by diet-induced hyperhomocysteinemia. We also have found recently that mild hyperhomocysteinemia produces endothelial dysfunction,39 as well as hypertrophy and altered vascular mechanics,40 in cerebral arterioles of CBS-deficient mice. Small arterioles in the mesentery also appear to be sensitive to modest elevations in plasma tHcy.14,17,27 Taken together, these findings suggest that microvessels are more sensitive to hyperhomocysteinemia than large conduit vessels.
In summary, we have found in this study that mice heterozygous for disruption of the Mthfr gene develop hyperhomocysteinemia that is exacerbated by dietary deficiency of folate. The strong interaction between Mthfr genotype and dietary folate in mice mimics the folate dependence of the human MTHFR 677TT genotype on plasma tHcy.23-25 In distinction to the clear effect of Mthfr genotype on plasma tHcy, however, the effects of hyperhomocysteinemia on endothelial function in cerebral arterioles are mediated primarily by diet rather than Mthfr genotype. These findings may have implications for the ongoing clinical trials of folate supplementation for the prevention and treatment of cardiovascular disease and venous thrombosis.41 Additional work will be required to define the relative roles of impaired homocysteine remethylation and altered gene-specific methylation in pathogenesis of cerebral vascular dysfunction in hyperhomocysteinemia.
Prepublished online as Blood First Edition Paper, November 20, 2003; DOI 10.1182/blood-2003-09-3078.
Supported by the Office of Research and Development, United States Department of Veterans Affairs; National Institutes of Health grants HL63943, NS24621, and HL62984; and an operating grant and a Senior Scientist Award (R.R.) from the Canadian Institutes of Health Research.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Kara Brown, Rochelle Erger, and Cynthia Lynch for technical assistance.