Graft-versus-host disease (GVHD) of the liver is characterized by bile duct damage and portal lymphocytic infiltrate. We report acute hepatitislike presentation of GVHD after donor lymphocyte infusion (DLI). Between April 1998 and September 2001, 73 patients received 94 DLI treatments. Liver GVHD developed after DLI in 22 (30%) patients whose median age was 43 years (range, 21 to 61 years). Onset of liver dysfunction was at 35 days (range, 11 to 406 days) after DLI. Fifteen patients underwent liver biopsy, and the diagnosis of liver GVHD was confirmed in 13 (87%) patients. After viral hepatitis and recent drug exposure were excluded, 11 (50%) patients were given a diagnosis of a hepatitic variant of GVHD based on histologic evidence of lobular hepatitis (n = 5), elevation of maximum serum alanine aminotransferase (ALT) or aspartate aminotransferase (AST) level more than 10 times the upper normal limit (n = 9), or both. There was a significant difference in maximum ALT (P = .002) and AST (P = .01) level between the hepatitic-variant and classical GVHD groups. GVHD progressed in 14 (64%) patients, and 10 patients died after a median follow-up of 221 days (range, 31-1284 days). These observations suggest that GVHD that occurs after DLI may have distinct clinical features. Hepatitic-variant GVHD should be considered in the differential diagnosis in DLI recipients with unexplained hepatitis.
Introduction
Cholestatic liver abnormalities in an allograft recipient with clinical or biopsy evidence of cutaneous or intestinal graft-versus-host disease (GVHD) are usually attributable to liver GVHD.1 Onset usually coincides with myeloid engraftment after transplantation, and progressive jaundice is the most common presenting feature of liver involvement.2 The serum alkaline phosphatase (ALP) level, a sensitive diagnostic marker for liver GVHD,3 rises steadily, as much as 20-fold above normal, with a parallel rise in serum bilirubin level. Serum levels of aspartate aminotransferase (AST or SGOT) and alanine aminotransferase levels (ALT or SGPT) are frequently elevated, especially during the early stages of GVHD, but they almost never are more than 10 times higher than normal.2 Liver biopsy is important to confirm the diagnosis and to exclude other treatable causes of liver dysfunction, such as drug effects, viral infection, or fungal infection. Typical liver GVHD is characterized by lymphocytic infiltration of small bile ducts with nuclear pleomorphism and epithelial cell dropout.4,5 The extent of both apoptosis and dropout cells serves to distinguish acute liver GVHD from the other causes of liver dysfunction.4
Recently, an unusual form of liver GVHD has been described. Strasser et al6 report their observations in 14 patients in whom chronic GVHD of the liver was accompanied by marked elevations of serum aminotransferase levels, clinically resembling acute viral hepatitis.6 Similarly, Fujii et al7 report a patient with liver GVHD, thought to be acute hepatitis, 23 days after allogeneic peripheral blood stem cell transplantation (SCT).7 In another case report, chronic GVHD, also thought to be acute hepatitis, 36 weeks after matched-unrelated allogeneic SCT for chronic myelogenous leukemia was described.8 In the present case series of 22 patients, we report our clinical observations of this hepatitic variant of liver GVHD that occurred after donor lymphocyte infusion (DLI).
Patients, materials, and methods
We retrospectively reviewed the data on 22 patients with clinical and laboratory evidence of liver GVHD that developed after DLI. Three additional patients were not included in this series because of incomplete information. Patients were treated with DLI after obtaining an informed consent approved by The Johns Hopkins University School of Medicine institutional review board. Patients received diagnoses of liver GVHD if they had progressive increases in serum liver enzyme levels after DLI and no other causes could be identified by history, physical examination, and standard screening tests. Patients had to have no history of new drug exposure and no recent change in the dose or schedule of their routine medications. Routine bacterial and fungal cultures were obtained to rule out ongoing subtle infection. The possibility of viral hepatitis caused by hepatitis A (HAV), B (HBV), C (HCV), herpes simplex (HSV), and varicella zoster (VZV) was ruled out by standard serologic tests. In the appropriate hosts, evidence of primary infection or reactivation of HSV, cytomegalovirus (CMV), or adenovirus was sought. Polymerase chain reaction (PCR) analysis was not routinely performed. Radiologic studies, including abdominal ultrasound or computed tomography (CT), were conducted to rule out the presence of an obstructive or intraparenchymal lesion. As a prerequisite for inclusion in this analysis, patients had to be starting a new immunosuppressive treatment or continuing an existing regimen for other manifestations of GVHD that was modified after the liver GVHD diagnosis. GVHD of the skin, gut, eye, or mouth was diagnosed in all patients based on established clinical and histologic criteria before (n = 4) or at (n = 18) the onset of liver GVHD.
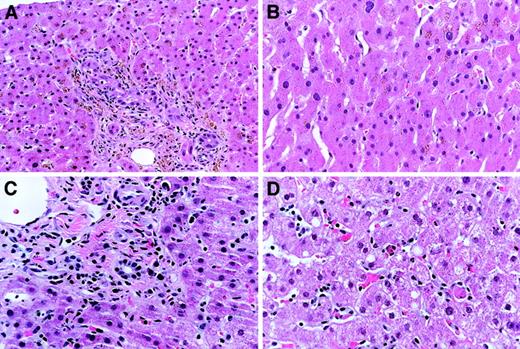
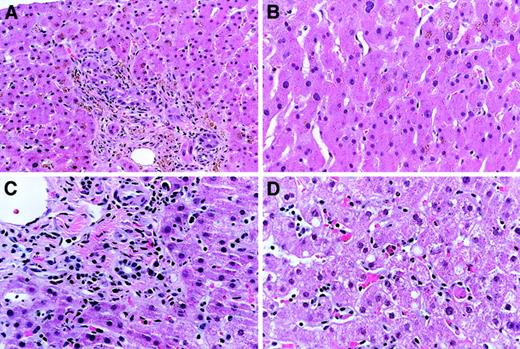
Fifteen (68%) patients underwent liver biopsy to rule out viral hepatitis and to confirm the diagnosis of GVHD. Based on the following histologic criteria, 2 subtypes of liver GVHD were defined. The first subtype was based on features consistent with classical GVHD if bile duct epithelial injury and portal lymphocytic infiltration occurred (Figure 1A). In this subtype, hepatocellular structure had to be relatively preserved with no significant inflammation (Figure 1B). The second subtype was based on features consistent with hepatitic variant of GVHD if bile duct injury was relatively mild (Figure 1C) and lobular hepatitis was the predominant histologic finding (Figure 1D). Liver biopsy specimens were not sent for viral culture. Biopsy specimens showing the histology of lobular hepatitis were evaluated for cytomegalovirus infection by immunohistochemical staining. Immunostaining for HSV and adenovirus was performed when clinically indicated. The diagnosis of hepatitic-variant GVHD was based on the presence of lobular hepatitis or on marked (more than 10 times the upper normal limit [UNL]) elevation of serum aminotransferase (ALT or AST) levels. The Wilcoxon rank sum test was used to compare maximum serum liver enzyme levels that included ALP, ALT, AST, total bilirubin, and direct bilirubin between patients with classical liver GVHD and those with hepatitic-variant GVHD.
Histologic changes of liver GVHD.
Characteristic histology of classical liver GVHD with bile duct lymphocytic infiltrates and injury. (A) Portal lymphocytic inflammation is also present. (B) Lobules show mild hemosiderin accumulation with no significant inflammation. (C) Hepatitic-variant liver GVHD demonstrates only mild chronic inflammation of the portal tracts, with minimal bile duct changes. (D) In contrast, the lobules show definite hepatitis. Original magnification × 25; hemotoxylene-eosine staining.
Histologic changes of liver GVHD.
Characteristic histology of classical liver GVHD with bile duct lymphocytic infiltrates and injury. (A) Portal lymphocytic inflammation is also present. (B) Lobules show mild hemosiderin accumulation with no significant inflammation. (C) Hepatitic-variant liver GVHD demonstrates only mild chronic inflammation of the portal tracts, with minimal bile duct changes. (D) In contrast, the lobules show definite hepatitis. Original magnification × 25; hemotoxylene-eosine staining.
Results
Between April 1998 and September 2001, 73 patients received 94 DLI treatments. Twenty-two (30%) patients (13 men, 9 women; age range, 21 to 61 years; median, 43 years) developed liver GVHD after receiving DLI with (n = 7) or without (n = 15) prior chemotherapy. Patient characteristics are summarized in Table1. Ten (45%) patients had prior acute GVHD after transplantation, and 2 of them had liver involvement. No patients were taking immunosuppressive therapy before DLI. Ten (45%) patients received CD3+ cells at a dose of less than 5 × 107, and in 12 (55%) patients the doses were 108 cells/mm3 or greater. For the entire group, median interval from the time of DLI to the onset of liver dysfunction was 35 days (range, 11 to 406 days). Liver GVHD with (n = 18) or without (n = 4) skin or gut GVHD was diagnosed in a median of 4 days (range, 0 to 25 days) after the onset of liver dysfunction, which was defined by liver function test results greater than 2 times the UNL.
For the entire group, the median peak serum levels of alkaline phosphatase (ALP), total bilirubin, direct bilirubin, ALT, and AST were 372 U/L (range, 106-2910 U/L), 2.7 mg/dL (range, 0.4-32 mg/dL), 1.2 mg/dL (range, 0.1-26.5 mg/dL), 410 U/L (range, 103-1540 U/L), and 245 U/L (range, 61-1256 U/L), respectively (Table2). Maximum levels of ALT or AST were more than 10 times the UNL in 11 patients (Tables 2 and3). Standard serologic test results were negative for HBV (n = 13), HBC (n = 13), HAV (n = 4), HSV (n = 2), VZV (n = 2), CMV (n = 2), as were blood CMV early antigen findings (n = 12). Blood viral cultures for CMV (n = 12), HSV (n = 7), and adenovirus (n = 6) and PCR studies for hepatitis C (n = 3) and adenovirus (n = 1) were also negative (n = number of patients).
Liver biopsy specimens were obtained from 15 patients in a median of 6 days (range, 1-67 days) after the onset of liver dysfunction. Thirteen of 15 (87%) specimens revealed histologic features consistent with liver GVHD and showing varying degrees of bile duct epithelial damage with or without portal lymphocytic infiltration. Histopathologic features of lobular hepatitis were present in 5 (33%) patients in whom immunostain findings for CMV (n = 5), HSV (n = 2), and adenovirus (n = 1) were negative. Of note, the lymphocytes infiltrating the hepatocellular parenchyma were CD3+ T cells in 2 samples studied. Other histopathologic features variably present in liver biopsy specimens included intralobular bile stasis, prominent hepatocellular hemosiderin accumulation, fat accumulation, mild to moderate portal or sinusoidal fibrosis, mild focal cholangitis, venous endothelialis, hepatocellular dropout, atrophy, or swelling, increased hepatocellular and nuclear polymorphism, focal hepatic necrosis, and small nodules of histiocytosis.
After the exclusion of viral infection and drug history, 11 (50%) patients received a diagnosis of hepatitic variant of liver GVHD. Characteristic features of these 11 patients are summarized in Table 3. Median ALP, ALT, AST, total bilirubin levels, and direct bilirubin levels in the hepatitic-variant group were 362 U/L, 825 U/L, 383 U/L, 2.6 mg/dL, and 1.4 mg/dL, respectively. There were significant differences in peak levels of ALT (P = .002) and AST (P = .01) between patients with hepatitic and those with classical liver GVHD as determined by the Wilcoxon rank sum test (Table4). Histologic features of the liver biopsy specimens obtained from 2 patients in this series are shown in Figure 1A-B (classical) and Figure 1C-D (hepatitic variant). Alkaline phosphatase, ALT, AST, and total bilirubin levels were 1980 U/L, 394 U/L, 199U/L, 11 mg/dL for classical and 158 U/L, 411 U/L, 246 U/L, and 1 mg/dL hepatitic-variant GVHD in these 2 patients, respectively. Median time from initial liver dysfunction to liver biopsy was 2 days (range, 1 to 57 days) for 5 patients who had histologic features of lobular hepatitis and 15 days (range, 3-67 days) for 10 patients who did not have this histologic component. Chemotherapy treatment before DLI and T-cell dose was not associated with the occurrence of hepatitic GVHD.
Patients were treated with high-dose combined immunosuppressive therapy that resulted in improvement or resolution of GVHD in 8 (36%) patients. Lichenoid chronic GVHD developed in 15 (68%) patients in a median of 27 days (range, 0 to 324 days) after the diagnosis of acute GVHD after DLI. Four (27%) of these patients had chronic GVHD at the initial presentation. As of the date of analysis, the median follow-up for all patients was 221 days (range, 31-1284 days). Ten (45%) patients died. Progressive GVHD was complicated by systemic bacterial or fungal infection and death in 6 patients. One patient in the classical liver GVHD group died of hepatic failure. Two patients died of relapse of underlying hematologic malignancies, and one died of alveolar hemorrhage. Nine patients in the hepatitic-variant group and 3 patients in the classical liver GVHD group remain alive.
Discussion
Although DLI may provide curative therapy through a graft-versus-tumor effect, complications result in significant morbidity and mortality. Prominent among these complications is acute and chronic GVHD, major factors affecting the outcome in these patients. In general, approximately 60% of the patients have acute (grade 2 or higher) or chronic GVHD, and half of these patients die of GVHD-related complications.9-11 Besides its high incidence and severity, DLI-GVHD appears to have distinct clinical features. In a recent case report, post-DLI chronic GVHD associated with polymyositis, polyserositis with a large pericardial effusion, and constrictive pericarditis was described.12 We have seen numerous DLI patients who have symptoms of acute and chronic GVHD or who experience rapid transition from acute to chronic GVHD (G.B.V., G.A., unpublished, 1997-2002). Although de novo chronic GVHD developed in some patients shortly after DLI, others had an unusual presentation without skin involvement. The clinical course of DLI-GVHD seems more complicated and prolonged, possibly because of its refractoriness to the standard treatments compared with SCT-GVHD. DLI patients also can have advanced-stage GVHD resulting in high mortality (G.B.V., unpublished observation, June 2001). Other groups have begun to recognize unusual presentations of DLI-GVHD with predominant gastrointestinal involvement.
In the present study, we report an unusual presentation of liver GVHD (hepatitic variant) in DLI recipients. Given the similar presentations reported after marrow or blood stem cell transplantation, it does not appear to be unique to DLI. However, hepatitic-variant GVHD seems more prevalent among DLI recipients. Because of the limitations of serologic studies in immunosuppressed patients, the low diagnostic yield of viral cultures, and the long turnaround time, liver biopsy specimens were obtained from 15 patients to rule out viral hepatitis and to confirm the diagnosis of liver GVHD. Although liver biopsy is useful for diagnosis, 2 patients had markedly elevated ALT and AST levels but did not show the histology of lobular hepatitis, likely reflecting the imperfect correlation between liver biopsy and serum ALT and AST levels.4 5 Therefore, we included marked (more than 10 times UNL) elevation of serum aminotransferase levels in the definition of hepatitic GVHD.
One possible limitation of the present study is the lack of a uniform evaluation using more sensitive molecular methods to rule out the viral etiology. Although it would be complementary, evaluating the liver biopsy specimens for HBV or HCV by PCR is not routine in our institution for the diagnosis of viral hepatitis. Culture of liver tissue is not a sensitive way to identify other viral infections either. These are probably best eliminated by histologic examination (eg, CMV, HSV), immunostaining of liver tissue (eg, adenovirus), and serologic testing. Despite the absence of a relevant history, drug-induced liver damage cannot be completely ruled out because all patients were taking their routine medications. Nonetheless, overall clinical and laboratory features of this cohort of patients were more consistent with liver GVHD than viral or drug-induced hepatitis.
It is difficult to explain why some of the DLI recipients had this unusual hepatitis presentation. The sample size was too small to identify any clinical or laboratory correlate with this presentation. It has been suggested that the duration of GVHD preceding biopsy influences the histologic features. Shulman et al4 studied the liver histology from patients with GVHD at different intervals after allogeneic bone marrow transplantation (BMT). Although biopsy specimens obtained before day 35 showed frequent acidophilic bodies and infrequent bile duct changes, biopsy specimens from days 35 to 90 after transplantation had more frequent bile duct lymphocytic infiltration and disruption, and biopsy specimens from patients with chronic GVHD (beyond day 90) showed more frequent portal fibrosis and bile duct atrophy and loss. In the present study, the interval between the onset of liver dysfunction and the time of liver biopsy was shorter in patients who had the hepatitic variant of GVHD than in those who did not. However, the presence of lobular hepatitis did not appear to be related to the timing of liver biopsy. Although lobular hepatitis accompanied by mononuclear cells and eosinophils into the portal triads can be seen during the early stage of liver GVHD, bile duct injury is not a typical histologic feature of this stage.5 13 Bile duct injury with or without portal inflammation was already visible in varying degrees in 4 of the 5 patients reported here. In addition, the degree of lobular hepatitis was far greater than typically seen in early stages of liver GVHD. Serum ALT and AST levels were more than 10 times the UNL in 3 of these patients. Finally, GVHD of skin or gut was present before liver biopsy was performed.
Unfortunately, the outcome for patients with liver GVHD was poor in this series of 22 DLI recipients. Approximately half the patients died after a median follow-up of less than 1 year. The major cause of death was progressive GVHD complicated by infections or hepatic failure. Of note, 3 of the 5 patients with lobular hepatitis had progression of liver GVHD. Although fewer patients with hepatitic-variant GVHD died than without the variant, the numbers are too small to draw any conclusion in terms of prognostic effect of the variant. In general, the treatment options for advanced liver GVHD are limited. In a large retrospective series, only 30% of patients with liver GVHD had resolution of liver abnormalities after initial treatment.14 Of patients with liver GVHD who do not respond to initial treatment, secondary treatment results in improvement or resolution of liver disease in 25% of patients.15 Ursodeoxycholic acid, in conjunction with standard immunosuppression therapy, may be useful in treating these patients. It has been suggested that UDCA reduces the class 1 human leukocyte antigen (HLA) expression, target for CD8+T cells, on hepatocytes.16
The molecular events leading to apoptosis in liver GVHD after stem cell transplantation are not well understood, but they involve donor T-cell activation and proliferation leading to tissue injury, in part by direct cytotoxicity through the Fas/Fas-ligand pathway. Cytotoxic T cells and natural killer cells damage target tissue by release of Fas-ligand and tumor necrosis factor–α (TNF-α).17,18A recent report suggests that the release of preformed FasL by infiltrating donor T cells may contribute to recipient tissue damage during the pathogenesis of acute GVHD.19 Lately, there has been a great deal of interest in using neutralizing anti-FasL monoclonal antibodies (mAbs) alone or in combination with anti–TNF-α in the treatment of acute GVHD in mice models.20 21
Other studies in murine transplantation models suggest that macrophage inflammatory protein-1 (MIP-1)–induced migration of CCR5-expressing CD8+ T cells into portal areas may have a role in GVHD-associated liver injury.22 Serody et al23 also noted the increased expression of MIP-1α associated with the transfer of allogeneic T cells, leading to enhanced recruitment of CD8+, but not CD4+ donor T cells in liver. Some evidence indicates that liver injury in chronic GVHD may result from the participation of donor CD4+ and CD8+ T cells.24
Data on the pathogenesis of GVHD occurring after DLI is even more limited. The often distinct presentation and the rapid clinical course of GVHD after DLI suggest that the immunopathophysiologic mechanisms of DLI-GVHD may be different from those of SCT-GVHD. This difference might be caused by the absence of initial inflammatory reactions to the conditioning treatment in DLI-GVHD. Preliminary data suggest that the ratio of Th1/Th2 cytokine expression is progressively shifted toward a Th2 cytokine (interleukin-10) predominance, similar to that for autologous GVHD. On the other hand, murine studies also showed that alloreactive T-cell proliferation after DLI was delayed (A. Hess, L. Luznik, unpublished data, June 2002).
Based on these clinical observations, we conclude that hepatitic-variant GVHD can be seen after DLI; therefore, it should be considered in the differential diagnosis in DLI recipients with unexplained hepatitis. The unusual manifestations and the relatively rapid clinical course of GVHD after DLI may result from distinct pathogenetic mechanism(s) that warrants study.
Prepublished online as Blood First Edition Paper, July 18, 2002; DOI 10.1182/blood-2002-03-0857.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Georgia B. Vogelsang, Sidney Kimmel Comprehensive Cancer Center, Bunting and Blaustein Cancer Research Bldg, 2M02G, The Johns Hopkins University School of Medicine, 1650 Orleans St, Baltimore, MD 21231-1000; e-mail:vogelge@jhmi.edu.