Key Points
In patients with IEI, improved EFS and higher donor chimerism may be achieved by targeting a cumulative busulfan AUC of 80 mg × h/L.
The data stress the importance of uniformly using a validated population pharmacokinetic model to estimate the busulfan cumulative exposure.
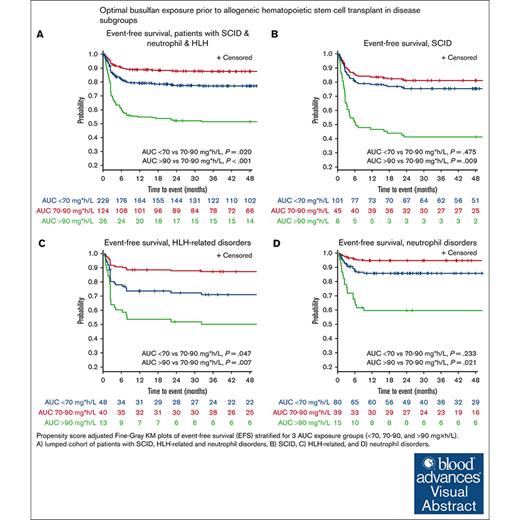
Visual Abstract
Allogeneic hematopoietic cell transplantation (HCT) is a potentially curative treatment strategy for patients with inborn errors of immunities (IEIs). The objective of this study was to assess the optimal busulfan exposure before allogeneic HCT for patients with an IEI who received an IV busulfan–based conditioning regimen. Patients from 17 international centers were included. The main outcome of interest was event-free survival (EFS). Patients were categorized into 4 IEI subgroups: combined immunodeficiency (CID), severe combined immunodeficiency (SCID), neutrophil disorders, and hemophagocytic lymphohistiocytosis (HLH)–related disorders. Busulfan exposure was calculated by individual centers (area under the curve [AUC]CENTER) and re-estimated using a nonlinear mixed–effects model (NONMEM; exposure defined as AUCNONMEM). Overall, 562 patients were included: 173 (30.8%) with CID, 154 (27.4%) with SCID, 101 (18.0%) with HLH-related disorders, and 134 (23.8%) with neutrophil disorders. The median busulfan AUCNONMEM was 69.0 mg × h/L and correlated poorly with the AUCCENTER (r2 = 0.54). In patients with SCID, HLH-related, and neutrophil disorders with a busulfan AUCNONMEM of 70 to 90 mg × h/L, 2-year EFS was superior to <70 mg × h/L, and >90 mg ×h/L. Full donor chimerism increased with higher busulfan AUCNONMEM, plateauing at 90 mg × h/L. For patients with CID, the optimal AUCNONMEM for donor chimerism was found to be >70 mg × h/L. Improved EFS and higher donor chimerism may be achieved by targeting a cumulative busulfan AUCNONMEM of 80 mg × h/L (range, 70-90). Our study stresses the importance of uniformly using a validated population pharmacokinetic model to estimate AUCNONMEM.
Introduction
Inborn errors of immunities (IEIs) arise from inherited abnormalities that affect distinct immune system components. These disorders, such as combined immunodeficiency (CID), severe combined immunodeficiency (SCID), and hemophagocytic lymphohistiocytosis (HLH), increase the risk of inflammation, immune dysregulation, and infections, profoundly impacting the quality of life (eg, increased risk of cancer) and life expectancy.1 Allogeneic hematopoietic cell transplantation (HCT) is a potentially curative treatment strategy for patients with IEI. In this context, busulfan is a widely used conditioning agent. The optimal busulfan dosing regimen remains a challenge given the narrow therapeutic range and significant inter- and intrapatient variability; underexposure has been associated with graft failure (GF) and disease recurrence, whereas overexposure can result in severe toxicity.2,3 Hence, in most pediatric HCT centers, therapeutic drug monitoring (TDM) of busulfan is the standard of care.3
For malignancies undergoing HCT, the optimal busulfan exposure is well defined.2 However, for patients with IEI, consensus is lacking, partly due to the absence of convincing data. Unlike malignant diseases, full myeloablation might not be as crucial for certain IEIs, as the degree of mixed chimerism is sometimes considered acceptable. Studies describe a wide variety of cumulative busulfan exposures (defined as the cumulative area under the curve [AUC]) ranging from 30 to 101 mg × h/L; 30,4 45 to 65,5,6 57.6,7 60 to 75,8 >70,9 and 78 to 101 mg × h/L.2 Moreover, these targets are difficult to interpret because of substantial heterogeneity within and between studies, mainly because centers use different pharmacokinetic (PK) models to estimate exposures.2,10,11 The difficulty in comparing busulfan exposure across centers has been demonstrated in the largest study to date, involving 674 patients, including 172 patients with IEI.2 Busulfan exposure derived from these centers did not align well with that estimated using a validated population PK model. When this model was applied to re-estimate busulfan exposure, it identified an optimal exposure of 78 to 101 mg × h/L in all patients, regardless of underlying disease, including patients with IEI.2 However, sufficient power was not present to make definitive recommendations.
We therefore aimed to assess the disease-specific relationship between busulfan exposure and clinical outcomes in a large cohort of patients with IEI. To achieve this, we estimated all cumulative AUCs using a previously internally and externally validated population PK model, based on raw time concentration data. We subsequently conducted a retrospective analysis to relate exposure of busulfan to various allogeneic HCT outcomes, such as event-free survival (EFS), acute graft-versus-host disease (aGVHD), and chronic GVHD (cGVHD), veno-occlusive disease (VOD), and GF/disease recurrence.
Methods
Study design
This study included patients with IEIs from 17 pediatric transplant centers in the Netherlands, the United States, Canada, Switzerland, United Kingdom, Italy, Germany, and Australia who, between 2000 and 2023, underwent their first allogeneic HCT using IV busulfan in the conditioning regimen (supplemental Table 1). Raw time concentration busulfan data were required. The minimum follow-up for surviving patients was 6 months. Although analyzed in retrospect, clinical data were collected prospectively by individual institutes and registered in clinical databases. Written informed consent was obtained from all the patients in accordance with the Declaration of Helsinki. The patients underwent transplantation according to site-specific HCT protocols.
Busulfan exposure
The initial busulfan dosage was determined using the patient's actual body weight or body surface area, depending on center preference. Typically, busulfan was administered for 3 to 5 days once daily or 4 times daily. Plasma samples were analyzed using validated analytical methods12,13 and were modeled using a previously validated population PK model.14 The cumulative AUC was estimated using nonlinear mixed–effects modeling (NONMEM; exposure defined as AUCNONMEM) and the raw concentration-time data provided by each center over the full treatment course.
Outcomes
Our main outcome of interest was EFS, defined as GF, recurrence of disease (if applicable, eg, HLH flare), or death. The follow-up period extended from the date of HCT to an event, last contact, death, or second HCT.
Other outcomes of interest were GF, treatment-related mortality (TRM), grade 2 to 4 aGVHD, cGVHD, acute toxicity (defined as moderate-to-severe VOD, grade 2 to 4 aGVHD, or lung toxicity), overall survival (OS), and moderate-to-severe cGVHD-free EFS (cGEFS). TRM was defined as death from causes unrelated to disease. GF was defined as nonengraftment, rejection (defined as <10% myeloid donor chimerism or the need for a second HCT). aGVHD was determined and classified based on the Glucksberg criteria,15 cGVHD using the Shulman criteria16 (and after 2017 the National Institutes of Health criteria), and VOD using institutional criteria (eg, modified Seattle, Baltimore criteria, or European Society for Blood and Marrow Transplantation criteria [EBMT]).17 Given the wide variation in chimerism practice and type of measurements across different centers, whole blood and myeloid chimerism were analyzed together. For each patient, the most recent (latest follow-up time point) chimerism measurement was used for the analysis.
Statistical analyses and potential confounders and/or effect modifiers
Determinants influencing the outcomes of interest were selected based on biological plausibility and available literature and were considered potential confounders or effect modifiers. An externally validated busulfan PK model was used to obtain post hoc Bayesian estimates of busulfan clearance (supplemental Table 2).14,18 The predictive value of the PK model for this data set was evaluated using goodness of fit plots (specifically the population and individual predictions, vs the observed concentrations stratified from the day of PK analysis, center of inclusion, age, and body weight group) and corrected visual predictive checks. Busulfan cumulative exposure was also calculated by individual centers (AUCCENTER) according to their preferred method. As a sensitivity analysis and to assess concordance, we compared the AUCCENTER with AUCNONMEM. Patients were categorized into 4 subgroups based on IEI subtype: CID, SCID, neutrophil disorders, and HLH-related disorders (including primary immune regulatory disorders). Within the CID group, well-defined CIDs (CD40 ligand deficiency, CD40 deficiency, DOCK8 deficiency, and the Wiskott-Aldrich syndrome) were analyzed separately.
Busulfan AUCNONMEM was modeled as a continuous variable in relation to the outcomes of interest, adjusted for propensity scores. We used adjusted models using the exponential, gamma, log-logistic, log-normal, logistic, normal, and Weibull survival functions. The best-fitting model was identified based on the lowest values of the Akaike information criterion and relative likelihood. Propensity scores were calculated to adjust for confounding using the following determinants: age (continuous), sex, matching status (match/mismatch), disease subgroup (CID/SCID/neutrophil disorder/HLH-related disorder), year of transplantation, and conditioning regimen (1 vs multiple alkylators). In the case of multicollinearity among determinants, the determinants with the most robust predictive effects were used for the propensity score calculation. In case of missing follow-up time data (for toxicity outcomes), the median time to event was imputed. If the event data were missing or unreported, we assumed that the event did not occur. Missing data on the potential determinants were included as dummy variables. Event probability was visualized using Kaplan-Meier plots with underlying propensity score–adjusted Fine-Gray models. Other predefined independent patient-specific characteristics of the outcomes were analyzed using multivariable Cox regression. For data exploration, we used visualization smoothing splines to categorize patients into busulfan exposure groups based on the outcomes of these analyses. The effect of these exposures on EFS was tested in predefined disease groups and the entire cohort of patients. The exposure group with the most pronounced predictive influence on the EFS was used for further analysis. To assess effect modification (indicated by a P <.05 for the interaction term), groups were examined separately. The continuous variables were grouped into predefined categories. Survival analysis was conducted using PROC PHREG and maximum likelihood estimation was conducted using PROC LIFEREG in SAS (version 9.4).
Results
Patient characteristics
In total, data from 587 patients were gathered, excluding 25 with a second HCT or no PK data (supplemental Figure 1). Overall, 562 patients were included in the final analysis: 173 (30.8%) with CID, 154 (27.4%) with SCID, 134 (23.8%) with neutrophil disorders, and 101 (18.0%) with HLH-related disorders (including 14 primary immune regulatory disorders). Genotype/phenotype distribution is displayed in supplemental Table 4. Most patients were male (n = 399, 71.0%) and the median age was 1.7 years (range, 0.1-27.0; Table 1). Busulfan combined with fludarabine was the most frequently used conditioning regimen (n = 392, 69.8%). Graft source was bone marrow in 312 (55.5%), cord blood in 153 (27.2%), and peripheral blood stem cells in 97 (17.3%) patients (Table 1).
Characteristics of the study population (N = 562)
| Characteristic . | n . | % . |
|---|---|---|
| Sex | ||
| Female | 163 | 29.0 |
| Male | 399 | 71.0 |
| Age, y | ||
| <0.5 | 114 | 20.3 |
| 0.5-1.5 | 146 | 26.0 |
| 1.5-5 | 131 | 23.3 |
| >5 | 171 | 30.4 |
| Graft source | ||
| Bone marrow | 312 | 55.5 |
| Cord blood | 153 | 27.2 |
| Peripheral blood | 97 | 17.3 |
| Donor | ||
| Family | 158 | 28.1 |
| Unrelated | 404 | 71.9 |
| Matching status | ||
| Matched | 317 | 56.4 |
| Mismatched | 192 | 34.2 |
| Unknown | 53 | 9.4 |
| Disease group | ||
| CIDs | 173 | 30.8 |
| SCID | 154 | 27.4 |
| Neutrophil disorders | 134 | 23.8 |
| HLH-related diseases | 101 | 18.0 |
| Serotherapy | ||
| Antithymocyte globulin | 265 | 47.2 |
| Alemtuzumab | 174 | 31.0 |
| No serotherapy | 87 | 15.5 |
| Unknown | 36 | 6.4 |
| Year of transplantation | ||
| <2013 | 184 | 32.7 |
| 2013 | 157 | 27.9 |
| Unknown | 221 | 39.3 |
| GVHD prophylaxis regimen | ||
| Cyclosporine containing | 392 | 69.8 |
| Tacrolimus containing | 42 | 7.5 |
| Other/unknown | 128 | 22.8 |
| Number of alkylators | ||
| 1 alkylator (busulfan) | 393 | 69.9 |
| 2 alkylators | 155 | 27.6 |
| Busulfan and unknown agent | 14 | 2.5 |
| Conditioning regimen | ||
| Busulfan/cyclophosphamide/fludarabine | 127 | 22.6 |
| Busulfan/fludarabine | 392 | 69.8 |
| Busulfan/cyclophosphamide/etoposide | 19 | 3.4 |
| Busulfan/fludarabine/clofarabine | 1 | 0.2 |
| Busulfan/fludarabine/thiotepa | 4 | 0.7 |
| Busulfan/fludarabine/melphalan | 4 | 0.7 |
| Busulfan/thiotepa | 1 | 0.2 |
| Busulfan/missing | 14 | 2.5 |
| Characteristic . | n . | % . |
|---|---|---|
| Sex | ||
| Female | 163 | 29.0 |
| Male | 399 | 71.0 |
| Age, y | ||
| <0.5 | 114 | 20.3 |
| 0.5-1.5 | 146 | 26.0 |
| 1.5-5 | 131 | 23.3 |
| >5 | 171 | 30.4 |
| Graft source | ||
| Bone marrow | 312 | 55.5 |
| Cord blood | 153 | 27.2 |
| Peripheral blood | 97 | 17.3 |
| Donor | ||
| Family | 158 | 28.1 |
| Unrelated | 404 | 71.9 |
| Matching status | ||
| Matched | 317 | 56.4 |
| Mismatched | 192 | 34.2 |
| Unknown | 53 | 9.4 |
| Disease group | ||
| CIDs | 173 | 30.8 |
| SCID | 154 | 27.4 |
| Neutrophil disorders | 134 | 23.8 |
| HLH-related diseases | 101 | 18.0 |
| Serotherapy | ||
| Antithymocyte globulin | 265 | 47.2 |
| Alemtuzumab | 174 | 31.0 |
| No serotherapy | 87 | 15.5 |
| Unknown | 36 | 6.4 |
| Year of transplantation | ||
| <2013 | 184 | 32.7 |
| 2013 | 157 | 27.9 |
| Unknown | 221 | 39.3 |
| GVHD prophylaxis regimen | ||
| Cyclosporine containing | 392 | 69.8 |
| Tacrolimus containing | 42 | 7.5 |
| Other/unknown | 128 | 22.8 |
| Number of alkylators | ||
| 1 alkylator (busulfan) | 393 | 69.9 |
| 2 alkylators | 155 | 27.6 |
| Busulfan and unknown agent | 14 | 2.5 |
| Conditioning regimen | ||
| Busulfan/cyclophosphamide/fludarabine | 127 | 22.6 |
| Busulfan/fludarabine | 392 | 69.8 |
| Busulfan/cyclophosphamide/etoposide | 19 | 3.4 |
| Busulfan/fludarabine/clofarabine | 1 | 0.2 |
| Busulfan/fludarabine/thiotepa | 4 | 0.7 |
| Busulfan/fludarabine/melphalan | 4 | 0.7 |
| Busulfan/thiotepa | 1 | 0.2 |
| Busulfan/missing | 14 | 2.5 |
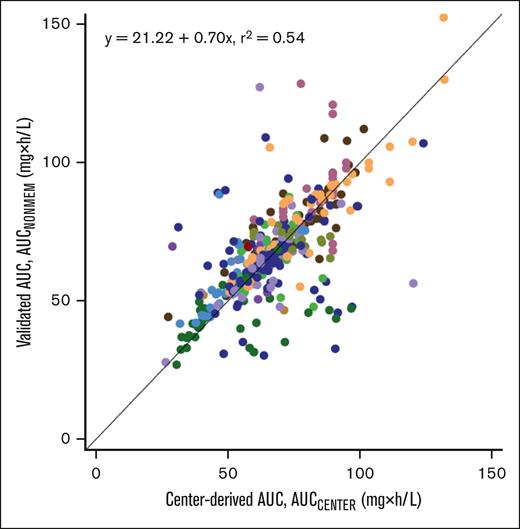
The blood sampling regimen, analytical busulfan measurement method, AUC calculation, target AUC, and dose adjustment strategy varied widely between centers. The median cumulative busulfan AUC (estimated using a validated PK model; AUCNONMEM) was 69.0 mg × h/L (range, 12.2-179.7; supplemental Table 1) and correlated poorly with the AUC that was reported by the individual centers (AUCCENTER, r2 = 0.54; Figure 1). Overall, the participating centers tended to underestimate the AUC (although some overestimated it), as indicated by the regression coefficient of 0.7 (Figure 1). The results of the prediction-corrected visual predictive checks indicated that the model had an adequate predictive performance across all age and weight categories (supplemental Figure 2) and all days of PK sampling in all centers (supplemental Figure 3). Furthermore, the individual PK parameters for all body weights were equally distributed around the population PK parameters (supplemental Figure 4).
Correlation between the center-derived busulfan AUC and the validated AUC. The busulfan exposure calculated using the centers (AUCCENTER) vs the exposure estimation using a validated PK model (AUCNONMEM; centers denoted by color).
Correlation between the center-derived busulfan AUC and the validated AUC. The busulfan exposure calculated using the centers (AUCCENTER) vs the exposure estimation using a validated PK model (AUCNONMEM; centers denoted by color).
Outcomes
The median time to follow-up was 1430 days. The estimated EFS at 1 and 2 years after HCT was 80.6% and 77.9%, respectively. At 3 and 5 years after HCT, the estimated EFS was 77.7% and 77.4%, respectively. At 2 years, the rate of GF was 10.4% and TRM was 12.7%. Independent predictors for EFS were a serotherapy regimen and a busulfan AUCNONMEM of 70 to 90 mg × h/L, whereas for GF AUCNONMEM of 70 to 90 mg × h/L and the conditioning regimen (busulfan + alkylator) were associated with superior outcomes (supplemental Table 3A), which was offset by a nonsignificant increase in TRM in patients who received 2 alkylators.
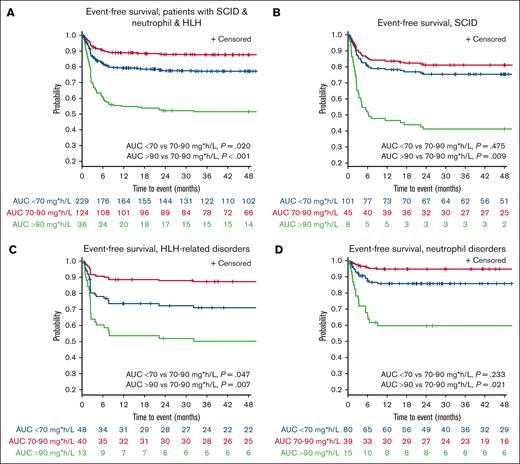
The CID disease subtype was an effect modifier (P = .03); therefore, these patients were analyzed separately. In the lumped group of patients with SCID, HLH-related, and neutrophil disorders (n = 389), the 2-year EFS was 78.5% (Figure 2; supplemental Figure 5). For this group, an optimal cumulative AUCNONMEM of 80 mg × h/L (range, 70-90) was found, corresponding to a 2-year EFS of 87.9% (95% confidence interval [CI], 80.3-92.6), superior to <70 mg × h/L (2-year EFS of 77.6%, adjusted hazard ratio [adj-HR], 1.97; 95% CI, 1.11-3.49; P = .02), and >90 mg × h/L (2-year EFS of 52.1%, adj-HR, 5.05; 95% CI, 2.43-10.49; P < .0001). The effect of exposure on EFS was analyzed separately in the disease groups (Figure 2B; supplemental Figure 5). In contrast, for patients with CID, no obvious optimal AUCNONMEM was found for EFS (supplemental Figure 6A), but GF incidence increased considerably if AUCNONMEM was <50 mg × h/L. For the well-defined CID subgroup (CD40 ligand deficiency, CD40 deficiency, DOCK8 deficiency, and Wiskott-Aldrich syndrome), patients with an AUCNONMEM >90 mg × h/L exhibited a modest improvement in EFS compared with those with lower exposures (supplemental Figure 6). However, this difference was not statistically significant.
Propensity score–adjusted Fine-Gray Kaplan-Meier plots of event-free survival stratified for 3 AUC busulfan exposure groups (<70, 70-90, and >90 mg × h/L). Patients with (A) SCID, HLH-related, and neutrophil disorders, (B) SCID, (C) HLH-related, and (D) neutrophil disorders.
Propensity score–adjusted Fine-Gray Kaplan-Meier plots of event-free survival stratified for 3 AUC busulfan exposure groups (<70, 70-90, and >90 mg × h/L). Patients with (A) SCID, HLH-related, and neutrophil disorders, (B) SCID, (C) HLH-related, and (D) neutrophil disorders.
For all patients with AUCNONMEM <70 mg × h/L, the events were primarily due to GF, whereas those with AUCNONMEM >90 mg × h/L predominantly experienced toxicity and TRM (supplemental Figures 7 and 8; supplemental Table 3A-D). The incidence of GF increased with AUCNONMEM <70 mg × h/L (adj-HR, 1.97; 95% CI, 1.12-3.48), with a greater impact in patients with AUCNONMEM <50 mg × h/L (adj-HR, 2.51; 95% CI, 1.26-5.03; supplemental Figure 7). TRM incidence was elevated with higher AUCNONMEM, with a notable rise in patients with AUCNONMEM >80 mg × h/L (adj-HR, 1.64; 95% CI, 1.00-2.68; supplemental Figure 7), which was primarily driven by elevated TRM in those exceeding 90 mg × h/L (adj-HR, 2.64; 95% CI, 1.43-4.87; supplemental Figures 7 and 8).
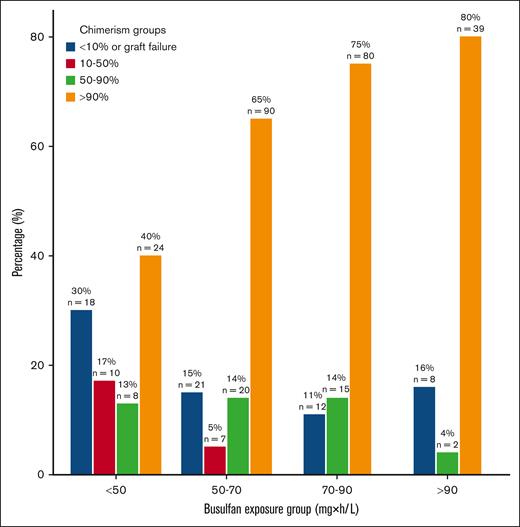
Chimerism
The chimerism data (whole blood and myeloid) were collected from 354 patients. Overall, donor chimerism levels (at the latest follow-up time point) increased with higher busulfan AUCNONMEM, plateauing at 90 mg × h/L (Figure 3). There was lower full donor chimerism (40.0%) in patients with AUCNONMEM <50, and a moderate increase (10.0%) in donor chimerism was observed from 50 to 70 mg × h/L to 70 to 90 mg × h/L. It was not feasible to analyze the chimerism data for each group of IEIs individually. Additionally, limited T-cell chimerism data were available, as routine testing is not a standard practice across many centers. Testing was typically conducted in some centers only when whole-blood donor chimerism levels fell below 95%.
OS and cGEFS
The overall estimated probabilities of OS 1 and 2 years after HCT were 85.7% and 83.3%, respectively. For patients with SCID, HLH, and neutrophil disorders, estimated cGEFS 1- and 2-year cGEFS were 73.5% and 72.3%, respectively, and appeared optimal in patients with AUCNONMEM 70 to 90 mg × h/L, slightly better but not significant <70 mg × h/L (adj-HR, 1.16; 95% CI, 0.74-1.80; P = .52), and significantly different from those with AUCNONMEM >90 mg × h/L (adj-HR, 2.63; 95% CI, 1.46-4.77; P = .001). For patients with CID, no optimum could be defined, given the comparable cGEFS incidence rates between the AUCNONMEM groups.
Toxicity
Generally, toxicities in this international cohort were very acceptable. The TRM rates at 1 and 2 years after HCT were 10.5% and 12.7%, respectively. The incidence of TRM was similar between patients with AUCNONMEM of <50 and those with AUCNONMEM of 70 to 90 mg × h/L (9.5% vs 11.9%; adj-HR, 0.98; 95% CI, 0.58-1.75; supplemental Table 3B). However, TRM rates significantly increased in patients with AUCNONMEM >90 mg × h/L (25.8%; adj-HR, 2.69; 95% CI, 1.24-5.83; supplemental Table 3B). The estimated probability of acute toxicity on day 100 (as a composite; moderate-to-severe VOD, grade 2 to 4 aGVHD, and lung toxicity) was 31.0%. The incidence of VOD was 19.9% in patients under 1 year old and 10.1% in those >1 year. Pulmonary toxicity was higher in patients receiving 2 alkylators than in those receiving only busulfan as alkylator (13.6% vs 7.1%; adj-HR, 2.09; 95% CI, 1.07-4.08; supplemental Table 3E). The estimated probability of fcGVHD (mild, moderate, and severe) at 2 years was 10.6%. Acute toxicity and aGVHD incidence increased with higher AUCNONMEM (supplemental Figure 8; supplemental Table 3A-D). Those receiving multiple alkylating agents also had a higher risk of acute toxicity (adj-HR, 1.66; 95% CI, 1.12-2.46) and VOD (adj-HR, 2.77; 95% CI, 1.47-5.20) than those receiving busulfan as only alkylating agent (supplemental Table 3D). In addition, patients with neutrophil disorders had a lower incidence of acute toxicity (adj-HR, 0.46; 95% CI, 0.27- 0.76; supplemental Table 3D). Lower age was associated with decreased aGVHD incidence (supplemental Table 3C).
Discussion
To our knowledge, this is the largest pharmacokinetic-pharmacodynamic (PK-PD) analysis in children and young adults with IEI to investigate the association between busulfan exposure and clinical outcomes. For each of the 4 distinctly different IEI groups, the optimum AUCNONMEM was found to be between 70 to 90 mg × h/L. For patients with AUCNONMEM <70 mg × h/L, negative events were primarily because of GF, whereas those with AUCNONMEM >90 mg × h/L predominantly experienced TRM. The analyses also showed that the center-derived AUC (AUCCENTER) and validated re-estimated AUC (AUCNONMEM) correlate poorly. This poor correlation makes the interpretation and comparison of study results in the literature nearly impossible and underscores the need to establish a consensus on which validated population PK model should be used. Uniform use of a validated population PK model to estimate busulfan exposure will improve day-to-day clinical practice and multicenter clinical trials.
Variation between centers in AUC estimation, including heterogeneity in the timing of blood sampling, was also demonstrated previously.2 Some centers use specialized PK software that varies in the structural model selected (1 vs 2 compartment), whereas others use a nonmodel-based trapezoidal methodology for exposure estimation. This results in substantially different AUC exposure estimates, as shown in the current analyses. Using a validated PK model to estimate the AUC limits the need to plan very specific sampling strategies and better approximates the “actual AUC,” as it considers the exact time of infusion, accounts for errors in sampling and analysis, and uses individual PK parameters to calculate exposures. In addition, most models capture the increased exposure on days 2 to 4 (or 5), which is needed to subsequently calculate the TDM-based individualized next dose to reach the optimal cumulative target exposure. Although many PK models exist (currently 44),19 only a few have been externally validated20 and can therefore reliably estimate busulfan exposure. The findings from these analyses highlight the urgent need for standardized procedures to estimate the AUC. After the consensus statement on the harmonization of busulfan plasma exposure units,21 a consensus statement on busulfan PK model harmonization/standardization might be beneficial.
Patients with SCID, HLH-related, and neutrophil disorder with an AUCNONMEM of 70 to 90 mg × h/L had the highest EFS. Consistent with the findings of previous studies, we found that increased AUCNONMEM resulted in lower GF incidence2,9 at the expense of higher TRM.2,9 For patients with HLH, there is a consensus that reducing the toxicity of conditioning is associated with improved outcomes, although the best approach to achieve this remains uncertain. A BMT-CTN trial (using alemtuzumab, fludarabine, and melphalan) showed high OS rates after the first HCT but low GF-free survival (∼40%).22 Two contemporary larger multicenter European studies showed better GF-free survival (70%-85%) after the first myeloablative HCT (with reduced toxicity achieved through TDM-guided busulfan exposure and treosulfan-based conditioning).23,24 The latter reports are in line with the results of our analyses, suggesting that myeloablative exposure (80 mg × h/L) is associated with the highest GF-free survival (∼90%) and full donor chimerism rates. Another report from Europe showed higher mixed-chimerism rates with lower busulfan exposure,5 which is in line with our analyses. For neutrophil disorders, there are some studies suggesting that nonmyeloablative exposure to busulfan (45-65 mg × h/L) is sufficient for high GF-free survival.6 The method used to estimate the busulfan AUC (eg, PK model or trapezoidal method) is unclear, making it uncertain whether the estimated AUC aligns with the “true” AUC, which was calculated using our validated PK model. In a recent large registry analysis (N = 712), mainly myeloablative regimens were used, and no impact of the regimen on outcomes was found.25 Our analyses suggest that myeloablative busulfan exposure is associated with the highest probability of GF-free survival (∼95%).
Although busulfan exposure of 70 to 90 mg × h/L resulted in the highest overall EFS in our study population, it can be debated whether this relatively high exposure target should be pursued in all patients. For example, patients with a low-performance score and more comorbidities may be more susceptible to increased toxicity (eg, GVHD and VOD) and subsequently TRM. In addition, although we were allowed to statistically combine the patients with SCID with HLH and neutrophil disorders in the analyses, it is important to realize that patients with SCID are distinctly different from the other 3 IEI groups. In addition, SCID itself is a heterogeneous set of disorders. A PIDTC cohort study including patients who underwent transplantation in the 1980s26 demonstrated the impact of genotype. In a more contemporary EBMT cohort (>2006), there was no impact of genotype on outcome27; however, it is likely that the known higher toxicity in certain genotypes (eg, DCLRE1C) may have been integrated into decision-making in this more contemporary cohort. In some but not all forms of SCID, minimal or even no conditioning is adequate to allow donor T-cell engraftment, fixing T-cell immune deficiency. However, various large cohort analyses have shown that patients who received either reduced-intensity or myeloablative conditioning (allowing for better myeloid engraftment) have better long-term immunity; for example, a more diverse T-cell repertoire, B-cell engraftment, and more likely to be immunoglobulin independent, and subsequently had a better long-term survival probability.26,27 The “optimal” busulfan exposure (using a uniform PK model to achieve this) remains to be determined. Due to the lack of granular genotype and phenotype data in this data set, we were unable to determine genotype-specific optimum exposures. However, we did not expect to find significant differences between genotypes, except for certain cases such as DCLRE1C. This expectation is supported by our current analysis and previous findings,2 which showed no differences between malignant and nonmalignant patients or within IEI subgroups.
Because the CID group is more heterogeneous than the other 3 groups, encompassing a wide range of clinical IEI phenotypes (associated with a wide range of genotypes), this may have complicated the analyses. When applying a stricter definition of confirmed genotypes for CID, we observed a trend toward higher EFS in patients with an exposure target of >90 mg × h/L, although the sample size was limited (n = 102; supplemental Figure 6). The latter is however consistent with previous findings, showing that patients with Wiskott-Aldrich syndrome and CD40L deficiency (busulfan-based) myeloablative conditioning appear to offer advantages over submyeloablative regimens, reducing GF incidence, mixed chimerism, and the need for secondary cellular rescue therapies.28,29 Based on these studies and our observation of higher donor chimerism in patients with an AUC >70 mg × h/L, it might be considered optimal for patients with CID to aim for a busulfan AUC of 80 mg × h/L (range, 70-90), although our analysis does not provide definitive proof of this, underscoring the need for further research.
Our findings indicate that dual alkylation therapies (eg, busulfan combined with a second alkylator), irrespective of busulfan exposure, are associated with a higher incidence of VOD and overall acute toxicity. This aligns with some recent large PK-PD analyses.2,3 Conversely, conditioning regimens with busulfan as the only alkylating agent at exposures up to 90 mg × h/L resulted in a significantly lower incidence of VOD compared with dual alkylation therapies, regardless of exposure levels.3
Overall, our results suggest that higher busulfan exposure increases the level of myeloid/whole-blood donor chimerism, plateauing at 90 mg × h/L, in which most patients obtained levels of >90%. Achieving high and stable donor chimerism may improve treatment outcomes because low mixed-chimerism levels have been associated with complications such as residual disease activity. Additionally, it can be hard to predict the stability of mixed chimerism. Those with mixed chimerism in the stem cell compartment may be at ongoing risk for (late) GF either by myeloid out-competition, immune rejection, or other immune complications. Mixed chimerism triggers some practitioners to proceed with donor lymphocyte infusion or a second HCT.30,31 To minimize this risk, targeting busulfan AUCNONMEM of 80 mg × h/L (range, 70-90) may be beneficial. Unfortunately, due to the relatively small sample size in the predefined disease groups and some missing data, we were unable to investigate the association between busulfan exposure and chimerism levels in a disease-specific manner.
Our study has some limitations. First, HCT treatment protocols likely improved over the 20-year period during which the patients were included. Although we adjusted for the year of HCT in our multivariate analysis, newer therapies (eg, antimicrobials) and ongoing improvements in supportive care likely had a positive impact on outcomes over time. Second, the criteria to define toxicity (eg, VOD) differed among centers, and the criteria have evolved over time. Third, the lack of a validated tool for accurate ranking of comorbidities in pediatric patients makes it difficult to assign pretransplant risk uniformly to the cohort. Fourth, we were not able to capture chimerism data uniformly because of the absence of a standardized approach and changes in measuring techniques over time. Given that myeloid chimerism is typically indicative of stem cell engraftment, we adopted our approach acknowledging its imperfections. Finally, although our study population was heterogeneous in terms of disease subtype and treatment protocols, the large number of patients allowed us to investigate exposure in particular disease groups given the large overall sample size. This is a major strength of this study, in which data from 17 international centers were analyzed using a standardized approach for estimating busulfan exposure, using the raw busulfan concentration-time profile of each patient. The current analyses provide a relatively broad AUC window for multiple indications. Expanding the number of patients would enable further subgroup analysis to define the optimum AUC for each pathology and refine the current recommendations.
In conclusion, in patients with IEI, improved EFS and higher donor chimerism may be achieved by targeting a cumulative busulfan AUCNONMEM of 80 mg × h/L (range, 70-90) and avoiding regimens that use >1 alkylator. These data stress the importance of uniformly using a validated population PK model to estimate the busulfan cumulative exposure. For patients with a low-performance score and more comorbidities, targeting a busulfan AUC of 60 mg × h/L (range, 50-70) may reduce toxicity (also a current recommendation of the EBMT guideline28) at the potential risk of increased mixed chimerism and GF. Prospective clinical trials are needed to confirm these findings.
Acknowledgments
J.-J.B. acknowledges support by the National Institutes of Health (NIH)/National Cancer Institute (NCI) Cancer Center Support Grant (P30 CA008748). C.L.E. was supported by the NIH’s National Center for Advancing Translational Sciences (grants KL2TR002492 and UL1TR002494). I.H.B. receives support from Gardenia (Amsterdam University Medical Center) and the NIH (grant R34AI155318). This work was supported by funding from the Intramural Research Program, NIH, NCI, Center for Cancer Research (S.-Y.P.).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH’s National Center for Advancing Translational Sciences.
Authorship
Contribution: T.B., M.G.-R., I.H.B., J.-J.B., A.L., and T.C.G.E. contributed to conceptualization, data curation, formal analysis, investigation, methodology, project administration, resources, software, supervision, validation, visualization, writing the original draft, and reviewing and editing of the manuscript; and T.G., M.H.-H., S.P., L.O., S.-Y.P., J.B., R.M.S., C.C.D., J.R.L.-B., M.K., H.B., A.-C.T., Y.T., C.M., E.M., M.S., G.D.E.C., R.C., R.F.W., M.C., M.P.C., M.A., S.E.L., C.L.E., H.L., S.C., C.E.N., P.J.S., S.J.K., M.Y.E.C.v.d.S., R.B., and C.A.L. contributed to data curation, methodology, writing the original draft, and reviewing and editing of the manuscript.
Conflict-of-interest disclosure: S.P. receives support for the conduct of sponsored trials through DFCI/BCH from Atara, AlloVir, and Jasper Therapeutics; consults for Cellevolve and Pierre Fabre; receives honorarium from Regeneron; and reports an IP license to Atara Biotherapeutics with all rights assigned to the Memorial Sloan Kettering Cancer Center. J.-J.B. received honoraria from Sobi, Sanofi, CTI, Smart Immune, Merck, and Advanced Clinical (all not related to this study). C.C.D. is a consultant for Jazz Pharmaceuticals and Alexion, Inc. The remaining authors declare no competing financial interests.
Correspondence: Jaap-Jan Boelens, Pediatrics Stem Cell Transplant and Cellular, Memorial Sloan Kettering Cancer Center, 1275 York Ave, Scholar 421, New York, NY 10065; email: boelensj@mskcc.org; and Imke H. Bartelink, Amsterdam University Medical Center, Location VUmc, De Boelelaan 1117, 1081 HV, Amsterdam, The Netherlands; email: i.bartelink@amsterdamumc.nl.
References
Author notes
T.B. and M.G. contributed equally to this study.
J.-J.B. and I.H.B. contributed equally to this study.
The data that support the findings of this study are available on request from the corresponding authors, Jaap-Jan Boelens (boelensj@mskcc.org) and Imke H. Bartelink (i.bartelink@amsterdamumc.nl).
The full-text version of this article contains a data supplement.