Key Points
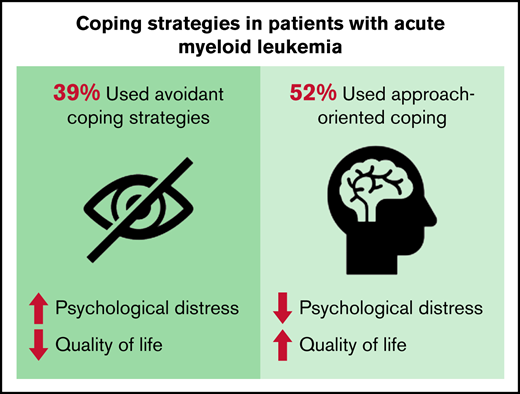
Patients newly diagnosed with high-risk AML are forced to cope with intensive, toxic treatments.
Use of approach-oriented coping strategies was associated with less psychological distress and better QOL.
Abstract
Patients diagnosed with acute myeloid leukemia (AML) face sudden-onset life-threatening disease that requires intensive treatments. Although their early disease trajectory is characterized by significant, toxic side effects, limited data are available describing coping strategies among patients with AML and how these inform patient-reported outcomes. We used cross-sectional secondary data analyses to describe coping in 160 patients with newly diagnosed high-risk AML. The Brief COPE, Hospital Anxiety and Depression Scale, Post-Traumatic Stress Disorder Checklist–Civilian Version, and Functional Assessment of Cancer Therapy–Leukemia were used at time of AML diagnosis to measure coping strategies, psychological distress, and quality of life (QOL), respectively. The median split method for distribution of coping domains and multivariate regression models were used to assess the relationship between coping and patient-reported outcomes. Participants (median age, 64.4 years) were mostly non-Hispanic White (86.3%), male (60.0%), and married (73.8%). Most (51.9%) had high utilization of approach-oriented coping strategies, whereas 38.8% had high utilization of avoidant coping strategies. At time of diagnosis, use of approach-oriented coping was associated with less psychological distress (anxiety, β = –0.262, P = .002; depression symptoms, β = –0.311, P < .001; and posttraumatic distress disorder symptoms, β = –0.596, P = .006) and better QOL (β = 1.491, P = .003). Use of avoidant coping was associated with more psychological distress (anxiety, β = 0.884, P < .001; depression symptoms, β = 0.697, P < .001; and posttraumatic distress disorder symptoms, β = 3.048, P < .001) and worse QOL (β = –5.696, P < .001). Patients with high-risk AML use various approach-oriented and avoidant coping strategies at time of diagnosis. Use of approach-oriented coping strategies was associated with less psychological distress and better QOL, suggesting a possible target for supportive oncology interventions.
Introduction
Patients with acute myeloid leukemia (AML) receiving intensive chemotherapy grapple with many psychological and physical challenges in the setting of an aggressive, sudden-onset disease accompanied by the need for rigorous and immediate treatment initiation.1-6 As part of their intensive treatments, patients with AML often have to endure toxic side effects (eg, mucositis, diarrhea), life-threatening complications (eg, sepsis, bleeding), and a prolonged hospitalization.7-9 In addition, patients with AML may have to cope with a high burden of psychological symptoms4-6 such as depressed mood, hopelessness, isolation, anxiety, and stress reactions that result from their uncertain prognosis, urgent need for treatment, and the abrupt disruption of quality of life (QOL) and physical function.1-3 The psychological distress and QOL deficits also negatively affect a variety of medical outcomes in the AML population.10 Although coping is essential to the management of an AML diagnosis and its treatment, data characterizing coping strategy use and its associations with patient-reported outcomes in the AML population are limited.
Coping is crucial to the care of patients with cancer, informs their care decisions, and is an integral part of patients’ experiences in managing challenges that accompany a cancer diagnosis and treatment. Approach-oriented coping strategies (eg, positive framing, problem-solving, utilizing emotional support) are cognitive and behavioral approaches that directly address or aid in the management of stress and the illness experience,11,12 whereas avoidant coping strategies (eg, denial, avoidance, emotional suppression) involve withdrawing from the stress. These coping styles have been associated with patient-reported outcomes, including symptoms of depression and anxiety, among other patient groups.10,11 For example, in patients diagnosed with incurable cancer, use of approach-oriented coping strategies has been associated with better QOL and less psychological distress, whereas use of avoidant coping strategies has been inversely correlated with these outcomes.13-17 Moreover, coping strategies affect patients’ self-efficacy, prognostic awareness, and adjustment to disease and treatment.18,19 Hence, coping plays a key role in multiple aspects of the cancer experience in a heterogenous population of patients. Because data on coping are limited in the vulnerable AML population, understanding coping and its association with patient-reported outcomes is essential.20,21
In the current study, we characterize coping strategy use among patients with AML enrolled in a supportive oncology trial and examine the associations between coping strategy use, psychological distress, and QOL. A comprehensive characterization of coping strategies in this population will enhance our nuanced understanding of the coping strategies patients rely on most during a taxing phase of their illness experience and inform development of future supportive care interventions to improve their QOL and care.
Methods
Study procedure
We conducted cross-sectional secondary analyses of baseline data from 160 hospitalized patients with high-risk AML enrolled in a multisite, randomized palliative care intervention trial (#NCT02207322) at Massachusetts General Hospital (Boston, MA), Duke University Medical Center (Durham, NC), Hospital of the University of Pennsylvania (Philadelphia, PA), and The Ohio State University (Columbus, OH) from January 2017 to July 2019.22 The institutional review boards at all participating sites approved this study. Participants completed baseline assessments within 72 hours of treatment initiation for AML. Only baseline data were used in this secondary analysis, thereby precluding the need to account for random assignment to the palliative care intervention. All participants provided written informed consent.
Participants
Eligible patients were hospitalized adults (≥18 years of age) with high-risk AML receiving intensive chemotherapy, within 72 hours of chemotherapy initiation, and English speaking with the ability to read and complete surveys with minimal assistance. We defined high-risk AML as: (1) newly diagnosed patients ≥60 years old; (2) patients with an antecedent hematologic disorder or therapy-related disease at any age; or (3) patients with a diagnosis of relapsed or primary refractory AML. We considered a combination of anthracycline and cytarabine (the “7 + 3” regimen) or a modification of this regimen in a clinical trial with additional drugs added or other similar intensive chemotherapy regimens requiring a 3- to 6-week hospitalization as intensive chemotherapy. Patients were excluded if they: (1) were diagnosed with acute promyelocytic leukemia; (2) were receiving nonintensive chemotherapy; (3) were already receiving palliative care; or (4) had a history of major psychiatric or comorbid disease that the treating oncologist believed would interfere with their adherence to informed consent and study procedures.
Sociodemographic and clinical data
At enrollment, participants reported demographic information, including age, race, ethnicity, sex, marital status, religious beliefs, education, and income. The electronic health record was used to confirm disease, treatment, and health care utilization information.
Patient-reported measures
We evaluated patients’ use of coping strategies with the Brief COPE, which is a 28-item questionnaire that assesses patients’ use of 14 methods of coping with 2 items for each method.18 To reduce questionnaire burden for participants, we limited our assessment to the following 7 coping strategies, which we felt were most appropriate for patients with AML undergoing intensive chemotherapy: use of emotional support, positive reframing, active coping, acceptance, self-blame, denial, and behavioral disengagement. Scores for each scale range from 2 to 8, with higher scores indicating greater use of that particular coping strategy. Using an aggregate of individual domain scores, coping strategies were grouped into 2 higher order domains of coping based on prior literature: approach-oriented coping (ie, use of emotional support, active coping, positive reframing, acceptance) or avoidant coping (ie, self-blame, denial, behavioral disengagement).16-18,20
Depression and anxiety symptoms were assessed by using the 14-item Hospital Anxiety and Depression Scale (HADS).21 The HADS consists of two 7-item subscales that measure symptoms of depression and anxiety, respectively. Clinically meaningful cutoffs are 1 to 2 points, and scores range from 0 to 21, with higher scores indicating worse mood symptoms.
We used the 17-item Post-Traumatic Stress Disorder Checklist– Civilian Version to assess posttraumatic distress disorder (PTSD) symptoms. The 17 items of this checklist are used to assess 3 categories of PTSD symptoms: intrusion (items 1-5), avoidance (items 6-12), and hypervigilance (items 13-17). The PTSD symptom severity score was obtained by summing the scores from each of the 17 items. Clinically meaningful cutoffs are 1 to 2 points, with higher scores indicating worse clinically significant PTSD symptoms (score range, 17-85).23,24
We evaluated QOL with the 44-item Functional Assessment of Cancer Therapy–Leukemia, which includes 5 subscales assessing physical, functional, emotional, and social well-being, and leukemia-specific concerns during the past week (score range, 0-176). Clinically meaningful cutoffs are 5 to 7 points, with higher scores indicating better QOL.25
Statistical analysis
STATA 16.0 (StataCorp, College Station, TX) was used to perform all statistical analyses. To summarize participants’ baseline characteristics, descriptive statistics (eg, mean, standard deviation) were used for continuous variables and proportions for categorical variables.
To determine the distribution of coping domains in our sample, we used the median split method because there are no validated cutoffs for high vs low coping published in the literature. The median split method entailed calculating the median scores for each of the 7 coping domains, then describing the proportion of patients with a score greater than the median as “high utilization” for each coping strategy.14,16,26 Patients scoring at the median were included in the “low utilizers” group. For the emotional support coping strategy, the median score (8) was considered as the cutoff point for “high utilizers” as the median score was also the highest possible score (8). “Use of multiple approach-oriented coping strategies” was defined as use of ≥3 coping strategies (with a score greater than the median) in the approach-oriented coping domain. “Use of multiple avoidant coping strategies” was defined as use of ≥2 coping strategies (with a score greater than the median) in the avoidant coping domain.
Unadjusted linear regression analyses were conducted to assess the relationship between baseline approach-oriented and avoidant coping strategies and patient-reported psychological distress (anxiety, depression symptoms, and PTSD symptoms) and QOL. We then used multivariate regression models adjusting for sociodemographic and disease factors (ie, age, sex, race, ethnicity, education, marital status, religious beliefs and diagnosis) shown to be associated with coping in other cancer populations.19 Given the potential for collinearity, separate models were built for anxiety, depression symptoms, PTSD symptoms, and QOL. Complete case analyses were conducted without accounting for missing data, based on the overall low rates of missingness. A two-sided P value <.05 was considered statistically significant.
Results
Demographic and patient characteristics
Of 235 eligible patients, 160 (68.1%) were enrolled. Table 1 summarizes participants’ baseline characteristics. Participants were mostly non-Hispanic White (n = 138 [86.3%]), with a median age of 64.4 years (range, 19.7-80.1 years). Forty percent (n = 64) were female, 73.8% (n = 118) were married, and 45.0% (n = 72) were college educated. Although the majority (n = 109 [68.1%]) of the participants were newly diagnosed with AML, 23.1% (n = 37) had relapsed AML, and 8.8% (n = 14) had refractory AML.
Participant baseline characteristics
| Characteristic . | Value (N = 160) . |
|---|---|
| Age, median (range), y | 64.4 (19.7-80.1) |
| Female sex | 64 (40.0%) |
| Race | |
| White | 138 (86.3%) |
| Black | 15 (9.4%) |
| American Indian | 4 (2.5%) |
| Asian | 2 (1.3%) |
| Other | 1 (0.6%) |
| Hispanic | 5 (0.3%) |
| Diagnosis type | |
| Newly diagnosed AML | 109 (68.1%) |
| Relapsed AML | 37 (23.1%) |
| Refractory AML | 14 (8.8%) |
| Relationship status | |
| Married | 118 (73.8%) |
| Divorced | 20 (12.5%) |
| Single | 12 (7.5%) |
| Widowed | 9 (5.6%) |
| Missing | 1 (0.6%) |
| Religion | |
| Catholic | 60 (37.5%) |
| Non-Catholic Christian | 53 (33.1%) |
| None | 22 (13.8%) |
| Jewish | 7 (4.4%) |
| Muslim | 2 (1.3%) |
| Atheist | 2 (1.3%) |
| Other | 13 (8.1%) |
| Missing | 1 (0.6%) |
| Education | |
| High school | 42 (26.3%) |
| College | 72 (45.0%) |
| Postgraduate | 44 (27.5%) |
| Missing | 2 (1.3%) |
| Income, $ | |
| <25 0000 | 21 (14.2%) |
| 25 000-50 000 | 32 (21.6%) |
| 50 000-100 000 | 45 (30.4%) |
| 100 000-150 000 | 23 (15.5%) |
| >150 0000 | 27 (18.2%) |
| Characteristic . | Value (N = 160) . |
|---|---|
| Age, median (range), y | 64.4 (19.7-80.1) |
| Female sex | 64 (40.0%) |
| Race | |
| White | 138 (86.3%) |
| Black | 15 (9.4%) |
| American Indian | 4 (2.5%) |
| Asian | 2 (1.3%) |
| Other | 1 (0.6%) |
| Hispanic | 5 (0.3%) |
| Diagnosis type | |
| Newly diagnosed AML | 109 (68.1%) |
| Relapsed AML | 37 (23.1%) |
| Refractory AML | 14 (8.8%) |
| Relationship status | |
| Married | 118 (73.8%) |
| Divorced | 20 (12.5%) |
| Single | 12 (7.5%) |
| Widowed | 9 (5.6%) |
| Missing | 1 (0.6%) |
| Religion | |
| Catholic | 60 (37.5%) |
| Non-Catholic Christian | 53 (33.1%) |
| None | 22 (13.8%) |
| Jewish | 7 (4.4%) |
| Muslim | 2 (1.3%) |
| Atheist | 2 (1.3%) |
| Other | 13 (8.1%) |
| Missing | 1 (0.6%) |
| Education | |
| High school | 42 (26.3%) |
| College | 72 (45.0%) |
| Postgraduate | 44 (27.5%) |
| Missing | 2 (1.3%) |
| Income, $ | |
| <25 0000 | 21 (14.2%) |
| 25 000-50 000 | 32 (21.6%) |
| 50 000-100 000 | 45 (30.4%) |
| 100 000-150 000 | 23 (15.5%) |
| >150 0000 | 27 (18.2%) |
Distribution of baseline coping strategies
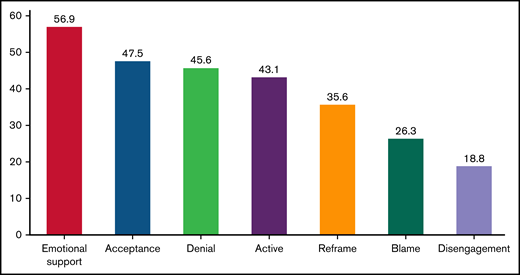
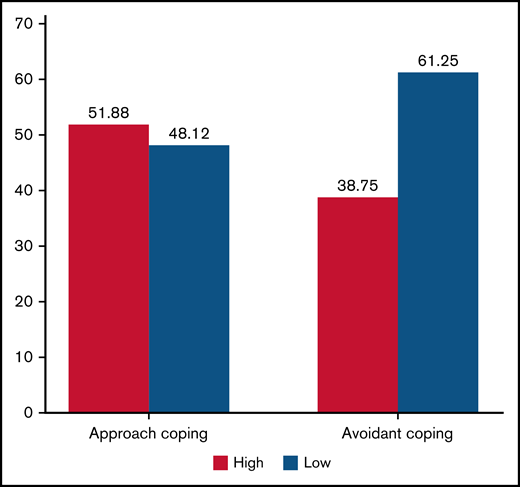
Emotional support, acceptance, and denial coping had the largest proportions of patients scoring above the median with each coping domain, whereas positive reframing, self-blame, and disengagement had the smallest. Figure 1 illustrates the proportion of patients scoring as high utilizers based on the median split method. Although more than one-half (56.9%) of our sample reported high utilization of emotional support coping, many also reported high use of acceptance (47.5%), denial (45.6%), active (43.1%), positive reframing (35.6%), and self-blame (26.3%) coping. Overall, 51.9% of patients scored as high on use of approach-oriented coping, whereas 38.8% scored as high on use of avoidant coping strategies (Figure 2). Notably, only 1 participant reported high use of both approach-oriented and avoidant coping strategies.
Distribution of coping strategies. The graphic displays the proportion of patients with a score greater than the median for each coping strategy. Median scores for each coping strategy were: acceptance, 7.0; denial, 2.0; active, 7.0; positive reframing, 6.0; self-blame, 2.0; behavioral disengagement, 2.0; and emotional support, 8.0.
Distribution of coping strategies. The graphic displays the proportion of patients with a score greater than the median for each coping strategy. Median scores for each coping strategy were: acceptance, 7.0; denial, 2.0; active, 7.0; positive reframing, 6.0; self-blame, 2.0; behavioral disengagement, 2.0; and emotional support, 8.0.
Distribution of patients based on approach and avoidant coping strategies. The graphic displays the proportion of patients with approach and avoidant coping strategies based on the median split for each coping strategy. Median scores for each coping strategy are as follows: approach, 19; avoidant, 5.
Distribution of patients based on approach and avoidant coping strategies. The graphic displays the proportion of patients with approach and avoidant coping strategies based on the median split for each coping strategy. Median scores for each coping strategy are as follows: approach, 19; avoidant, 5.
The use of multiple coping strategies
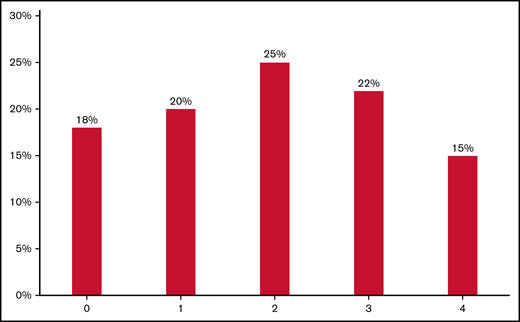
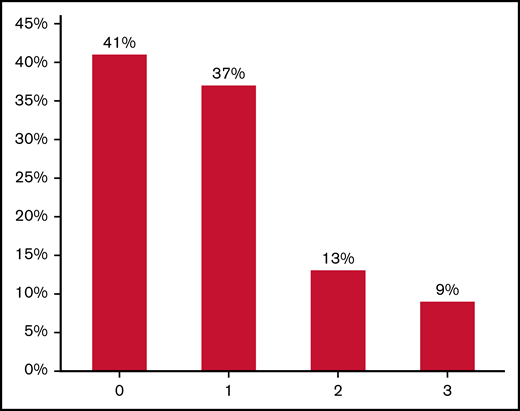
Figures 3 and 4 illustrate the distribution of patients who were high utilizers of approach-oriented and avoidant coping strategies, respectively. Overall, 15% of our sample scored as high utilizers of all 4 approach-oriented coping domains (ie, emotional support, acceptance, active coping, positive reframing), whereas only 9% were categorized as high utilizers of all 3 avoidant coping domains (ie, denial, self-blame, disengagement).
Distribution of patients who were high utilizers of multiple approach-oriented coping domains: emotional support, reframe, active, and acceptance. The graphic displays the distribution of patients who were high utilizers of approach-oriented coping domains defined as patients who scored above the median on a coping domain. For the emotional support coping domain, “high utilizers” were patients who scored the median (8) because the median was the maximum score for that domain. Although 18% of patients scored below the median or median (for emotional support) for all approach-oriented coping domains, 20%, 25%, 22%, and 15% were patients with high approach-oriented coping strategies based on 1, 2, 3, and 4 domains, respectively.
Distribution of patients who were high utilizers of multiple approach-oriented coping domains: emotional support, reframe, active, and acceptance. The graphic displays the distribution of patients who were high utilizers of approach-oriented coping domains defined as patients who scored above the median on a coping domain. For the emotional support coping domain, “high utilizers” were patients who scored the median (8) because the median was the maximum score for that domain. Although 18% of patients scored below the median or median (for emotional support) for all approach-oriented coping domains, 20%, 25%, 22%, and 15% were patients with high approach-oriented coping strategies based on 1, 2, 3, and 4 domains, respectively.
Distribution of patients who were high utilizers for multiple avoidant coping domains: denial, self-blame, and disengagement. The graphic displays the distribution of patients who were high utilizers of avoidant coping domains defined as patients who scored above the median on a coping domain. Although 41% of patients scored below the median for all 3 avoidant coping domains, 37%, 13%, and 9% were patients with high avoidant coping strategies based on 1, 2, and 3 domains, respectively.
Distribution of patients who were high utilizers for multiple avoidant coping domains: denial, self-blame, and disengagement. The graphic displays the distribution of patients who were high utilizers of avoidant coping domains defined as patients who scored above the median on a coping domain. Although 41% of patients scored below the median for all 3 avoidant coping domains, 37%, 13%, and 9% were patients with high avoidant coping strategies based on 1, 2, and 3 domains, respectively.
Associations of coping strategies with psychological distress and QOL
Based on our multivariate regression models that adjusted for multiple factors, approach-oriented coping was associated with less anxiety (β = −0.262, standard error [SE] = 0.085, P = .002), depression symptoms (β = −0.311, SE = 0.074, P < .001), and PTSD symptoms (β = −0.596, SE = 0.212, P = .006). In contrast, avoidant coping was associated with more anxiety (β = 0.884, SE = 0.134, P < .001), depression symptoms (β = 0.697, SE = 0.122, P < .001), and PTSD symptoms (β = 3.048, SE = 0.293, P < .001) (Table 2). Approach-oriented coping was associated with better QOL (β = 1.491, SE = 0.501, P = .003), and avoidant coping was associated with worse QOL (β = −5.696, SE = 0.768, P < .001).
Association between avoidant and approach coping strategies, psychological distress, and QOL
| Coping strategy . | QOL . | Depression . | Anxiety . | PTSD . | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B . | SE . | P . | B . | SE . | P . | B . | SE . | P . | B . | SE . | P . | |
| Approach | 1.491 | 0.501 | .003 | −0.311 | 0.074 | <.001 | −0.262 | 0.085 | .002 | −0.596 | 0.212 | .006 |
| Avoidant | −5.696 | 0.768 | <.001 | 0.697 | 0.122 | <.001 | 0.884 | 0.134 | <.001 | 3.048 | 0.293 | <.001 |
| Coping strategy . | QOL . | Depression . | Anxiety . | PTSD . | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B . | SE . | P . | B . | SE . | P . | B . | SE . | P . | B . | SE . | P . | |
| Approach | 1.491 | 0.501 | .003 | −0.311 | 0.074 | <.001 | −0.262 | 0.085 | .002 | −0.596 | 0.212 | .006 |
| Avoidant | −5.696 | 0.768 | <.001 | 0.697 | 0.122 | <.001 | 0.884 | 0.134 | <.001 | 3.048 | 0.293 | <.001 |
Linear regression models adjusted for patients’ age, sex, race, ethnicity, education, marital status, religious beliefs, and diagnosis.
Associations of the use of multiple coping strategies with psychological distress and QOL
Table 3 depicts the association between patients’ use of multiple coping strategies and patient-reported outcomes based on multivariate regression models adjusting for relevant factors. Patients who used multiple approach-oriented coping strategies had lower psychological distress (anxiety [β = −1.887, SE = 0.666, P = .005], depression symptoms [β = −2.140, SE = 0.589, P = .001], and PTSD symptoms [β = −3.995, SE = 1.673, P = .020]) and better QOL (β = 11.585, SE = 3.930, P = .004). In contrast, patients who used multiple avoidant coping strategies had higher psychological distress (anxiety [β = 4.522, SE = 0.755, P < .001], depression symptoms [β = 3.322, SE = 0.692, P < .001], and PTSD symptoms [β = 13.830, SE = 1.801, P < .001]) and worse QOL (β = −28.545, SE = 4.369, P < .001).
Association between the use of multiple avoidant or approach-oriented coping strategies, psychological distress, and QOL
| Use of multiple coping strategies . | QOL . | Depression . | Anxiety . | PTSD . | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B . | SE . | P . | B . | SE . | P . | B . | SE . | P . | B . | SE . | P . | |
| Use of multiple approach-oriented coping strategies | 11.585 | 3.930 | .004 | −2.140 | 0.589 | .001 | −1.887 | 0.666 | .005 | −3.995 | 1.673 | .020 |
| Use of multiple avoidant coping strategies | −28.545 | 4.369 | <.001 | 3.322 | 0.692 | <.001 | 4.522 | 0.755 | <.001 | 13.830 | 1.801 | <.001 |
| Use of multiple coping strategies . | QOL . | Depression . | Anxiety . | PTSD . | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B . | SE . | P . | B . | SE . | P . | B . | SE . | P . | B . | SE . | P . | |
| Use of multiple approach-oriented coping strategies | 11.585 | 3.930 | .004 | −2.140 | 0.589 | .001 | −1.887 | 0.666 | .005 | −3.995 | 1.673 | .020 |
| Use of multiple avoidant coping strategies | −28.545 | 4.369 | <.001 | 3.322 | 0.692 | <.001 | 4.522 | 0.755 | <.001 | 13.830 | 1.801 | <.001 |
Linear regression models adjusted for patients’ age, sex, race, ethnicity, education, marital status, religious beliefs, and diagnosis.
Discussion
In this secondary analysis of baseline data from a randomized controlled trial, we characterized the use of coping strategies employed by patients newly diagnosed with high-risk AML and found an association between patients’ use of coping strategies and their psychological distress and QOL. More than one-half (51.9%) of our sample were high utilizers of approach-oriented coping, with the 3 most commonly used coping strategies being emotional support (56.9%), acceptance (47.5%), and active coping (43.1%). However, more than one-third (38.8%) of our sample were high utilizers of avoidant coping strategies such as denial (45.6%) and self-blame (26.3%). Furthermore, 1 participant reported high use of discordant coping strategies (ie, both approach-oriented and avoidant coping strategies). We also showed that the use of approach-oriented coping shortly after diagnosis is associated with less psychological distress and better QOL. In contrast, avoidant coping was associated with more psychological distress and worse QOL. These findings underscore the critical role of coping in the lived experiences of patients newly diagnosed with AML who are hospitalized for high-dose therapy.
Despite the importance of coping in helping patients withstand the high psychological and physical symptom burden that accompanies a cancer diagnosis, data describing the nature of coping in patients with hematologic malignancies, especially those with high-risk AML, are lacking. Our findings provide valuable insights into the nature of coping strategies during a critical time in their disease trajectory. Unlike patients with solid tumors for which approach-oriented coping strategies are more frequently reported by patients (ie, emotional support coping [77.0%], positive reframing coping [49.1%], active coping [48.5%], acceptance coping [44.8%]),19 we found that a substantial proportion of patients with AML use both approach-oriented (emotional support, 56.9%) and avoidant (denial, 45.6%) coping at the time of diagnosis. This is likely a consequence of the abrupt onset of illness and the need for urgent hospitalization to initiate therapy, which may result in more avoidant coping techniques such as denial. Nonetheless, these findings underscore the need for oncology clinicians to systematically assess coping in this population to better inform their approach in addressing the psychological burden of the diagnosis and treatment.22
Data on how coping strategies affect illness experience and patient-reported outcomes in AML are also inadequate.17 Although a few studies have examined the association between individual coping strategies and clinical outcomes in other cancer populations,18,19 we found that the use of one or multiple approach-oriented coping strategies was associated with less psychological distress and better QOL in patients with high-risk AML. In contrast, the use of one or multiple avoidant coping strategies was associated with more psychological distress and worse QOL. Prior studies in patients with solid tumors have also shown that the use of approach-oriented coping is associated with better QOL.19,20,27-30 By assessing coping earlier in their disease and treatment trajectories, we can identify and intervene with patients at particular risk of poor patient-reported outcomes. Interestingly, recent studies have shown that supportive care interventions such as the integration of palliative care for patients with cancer can facilitate approach-oriented coping and mediate the impact of the intervention on patient-reported QOL and mood.10 Thus, future interventions (eg, palliative care–based,31 positive psychology–based,32,33 resilience-based34 ) should focus on fostering approach-oriented coping as a strategy to lessen psychological distress, promote treatment adherence, and improve QOL of patients with AML. Specifically, supportive interventions could educate patients about coping strategies and their observed associations with clinical outcomes while using specific positive psychology–based activities (eg, journaling daily blessings) and cognitive behavior skills training (eg, reframing negative events) to cultivate individual coping strategies.
In addition to its impact on psychological distress and QOL, coping has been associated with decision-making and illness perception among patients with cancer.14-16,26 Because patients with high-risk AML have to make multiple immediate decisions about their treatment, the utilization of certain coping strategies could affect their treatment options, trajectory of treatment, and their end-of-life outcomes. Hence, future longitudinal research on coping may inform the development of behavioral interventions and decision-making tools that could fill a gap in the care of patients with hematologic malignancies, thereby improving prognostic awareness and adaptation to aggressive disease burden.
There are several limitations to our study. First, the patient populations from the tertiary academic cancer centers were predominantly married, educated, and non-Hispanic White, which affects the generalizability of our findings to patients from minority and lower socioeconomic backgrounds. Prior work on coping in patients from minority ethnic and racial backgrounds have shown variations in their coping strategies (eg, more utilization of self-distraction,35 venting, positive reappraisal,36 emotional suppression37 ) compared with White patients.38 Second, although we assessed coping during a critical and finite period of time (ie, within 72 hours of chemotherapy initiation), coping strategies may evolve over time in this population; future research should examine coping and its association with medical and patient-reported outcomes longitudinally. Also, the dose–response relationship between use of coping strategies and patient-reported outcomes would be useful and should be explored in future studies. Third, although the Brief COPE is a valid and reliable measure of coping, it is limited in the scope and number of coping strategies assessed; this is the first time we are characterizing coping according to the number of coping strategies in each domain. Also, the Brief COPE may not capture the full spectrum of coping strategies used by patients with AML and their impact with serious illness. Furthermore, although our models examining the effect of utilization of multiple coping strategies show clinically meaningful differences in QOL and symptoms of anxiety, depression, and PTSD, it is challenging to estimate whether differences in these patient-reported outcomes based on changes in coping strategies are clinically meaningful, given the lack of clinically meaningful cutoffs for the Brief COPE. Further qualitative assessments of coping, including ethnographic fieldwork and in-depth interviews, could further elucidate the nuances of coping strategies in the lived experiences of patients with high-risk AML to inform supportive oncology interventions.
In conclusion, our study shows that most patients with high-risk AML use both approach-oriented and avoidant coping strategies. Importantly, our results reveal links between approach-oriented coping strategies and improved patient-reported outcomes such as decreased symptoms of anxiety, depression, and PTSD, and better QOL. These findings highlight the need for early integration of supportive oncology interventions that help patients foster approach-oriented coping strategies. Finally, by characterizing the use of coping strategies in patients with high-risk AML, we have identified opportunities to alleviate the burden of suffering in this vulnerable population.
Acknowledgments
A.E.-J. is a scholar in clinical research for the Leukemia & Lymphoma Society. T.W.L. is a Cambia Sojourns Scholar. Time for data analysis and manuscript preparation was supported by the National Institutes of Health, National Cancer Institute (grant K08CA251654, H.L.A.).
Authorship
Contribution: All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; all were involved in drafting the article or revising it critically for important intellectual content; and all provided final approval of the manuscript and agree to be accountable for all aspects of the work.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Hermioni L. Amonoo, Department of Psychiatry, Brigham and Women’s Hospital, 60 Fenwood Rd, Boston, MA 02115; e-mail: hermioni_amonoo@dfci.harvard.edu.
References
Author notes
T.W.L. and A.E.-J. are joint senior authors and joint last authors.
Requests for original data may be made by contacting Hermioni L. Amonoo (e-mail: hermioni_amonoo@dfci.harvard.edu).