TO THE EDITOR:
The American Society of Hematology (ASH) Guidelines for sickle cell disease (SCD) define chronic pain as reports of ongoing pain present on most days over the past 6 months in either a single location or multiple locations.1 Approximately 30% to 40% of adolescents and adults living with SCD have at least 1 episode of chronic pain.1 Current ASH guidelines for managing chronic pain in individuals with SCD do not include an evaluation for trauma, specifically sexual violence, as a precipitating cause.1
Individuals with SCD and a history of interpersonal violence exposure were almost 5 times more likely to report chronic pain and >6 times more likely to report the use of opiate-based medications daily.2 Works et al established a significant relationship between chronic pain and a history of trauma.3 Despite Works et al categorizing sexual abuse as a common traumatic experience, no study has explicitly evaluated the relationship between sexual violence as a source of trauma and chronic pain in individuals with SCD.3 Guidelines for treating individuals with SCD urge for routine screening of depression and anxiety, but not for sexual violence-related trauma, a risk factor for opioid disorder disease.1
In case 1, in 2015, an 18-year-old individual with hemoglobin SS was the victim of a sexually violent trauma that was not revealed to the SCD team until 2 years after the event when the patient was interviewed about the gradual change in their health care utilization. The individual was seen in the Emergency Department (ED) and hospitalized approximately once and received 2 prescriptions of opioids corresponding to 22.5 morphine equivalents 2 years before the traumatic event. The individual was seen in the ED 1 time and admitted 4 times and received 13 prescriptions of opioids corresponding to 3125 morphine equivalents 1 year before the traumatic event. The patient received 14 prescriptions of opioids corresponding to 3520 morphine equivalents 1 year after the event and 29 prescriptions of opioids corresponding to 8130 morphine equivalents 2 years after the event, a relative increase of 12.6% and 160.1%, respectively (Table 1 part A). All ED visits and hospitalizations were for pain (ED visits were distinct from the hospitalization visits).
Description of hospital visits for the 2 patients with SCD, history of ED visits, and morphine equivalents per year before and after each case
| Year . | Hospital visits . | ED visits . | Morphine equivalents . |
|---|---|---|---|
| (A) Case 1 | |||
| −2 | 1 | 0 | 22.5 |
| −1 | 4 | 1 | 3125 |
| Trauma | 3 | 1 | 2020 |
| +1 | 2 | 3 | 3520 |
| +2 | 6 | 0 | 8130 |
| +3 | 2 | 6 | 3824 |
| (B) Case 2 | |||
| −2 | 0 | 1 | 510 |
| −1 | 1 | 0 | 2760 |
| Trauma | 2 | 0 | 2497.5 |
| +1 | 11 | 0 | 8970 |
| +2 | 5 | 2 | 3105 |
| +3 | 0 | 3 | 2587.5 |
| Year . | Hospital visits . | ED visits . | Morphine equivalents . |
|---|---|---|---|
| (A) Case 1 | |||
| −2 | 1 | 0 | 22.5 |
| −1 | 4 | 1 | 3125 |
| Trauma | 3 | 1 | 2020 |
| +1 | 2 | 3 | 3520 |
| +2 | 6 | 0 | 8130 |
| +3 | 2 | 6 | 3824 |
| (B) Case 2 | |||
| −2 | 0 | 1 | 510 |
| −1 | 1 | 0 | 2760 |
| Trauma | 2 | 0 | 2497.5 |
| +1 | 11 | 0 | 8970 |
| +2 | 5 | 2 | 3105 |
| +3 | 0 | 3 | 2587.5 |
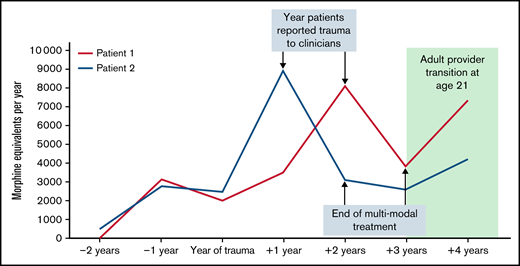
The attending hematologist made the diagnosis of chronic pain based on the established definition by the ASH Guidelines, “…reports of ongoing pain present on most days over the past six months in either a single location or multiple locations.”1 The attending hematologist made the diagnosis because of the patient’s complaint of pain in multiple locations over the past 2 years, including the back, arms, and legs. After a diagnosis of chronic pain syndrome following a traumatic sexual event, multimodal treatment for chronic pain included monthly blood transfusion therapy, oral methadone at a starting dose of 5 mg per day, and counseling. Clinicians concluded the patient experienced suicidal ideation and anxiety surrounding her home life, sexuality, and previous trauma resulting in posttraumatic stress disorder based on Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) criteria. The patient received counseling at an outside site focusing on working through the patient’s anxiety and finding coping strategies for stressors at home through cognitive behavioral therapy. The patient was seen 25 times over 13 months, 19 of which were predominately for transfusions. The patient's baseline hemoglobin S% level was 82.9%. The goal of transfusion therapy was to keep hemoglobin S% level <50%. The mean pretransfusion hemoglobin S level was 38.1% after 13 months of treatment. The patient received 18 opioid prescriptions during the multimodal therapy corresponding to 6534 morphine equivalents, a relative reduction of 19.6% from 1 year after the trauma (Figure 1). The patient remained on 5 mg of methadone throughout treatment and was off methadone at the end of treatment, which is 13 months of multimodal treatment. After completion of the multimodal therapy for 13 months, the patient reported that they were without pain on most days; no longer meeting the definition of chronic pain syndrome.
Graph depicting the trend of morphine equivalents for each case. The year the trauma occurred, the year the trauma was told to clinicians, the end of multimodal treatment (chronic blood transfusions, counseling, and methadone), and the year both patients were transferred to the adult SCD team are listed.
Graph depicting the trend of morphine equivalents for each case. The year the trauma occurred, the year the trauma was told to clinicians, the end of multimodal treatment (chronic blood transfusions, counseling, and methadone), and the year both patients were transferred to the adult SCD team are listed.
In case 2, in 2017, an 18-year-old individual with hemoglobin SC was the victim of a sexually violent trauma that was not revealed to the SCD team until 1 year after the event when the patient was interviewed about the gradual change in their health care utilization. The individual was seen in the ED and hospitalized approximately once and received 3 prescriptions of opioids corresponding to 510 morphine equivalents 2 years before the traumatic event. The individual was seen in the ED 0 times and admitted 1 time and received 12 prescriptions of opioids corresponding to 2760 morphine equivalents 1 year before the traumatic event. The patient received 27 prescriptions of opioids corresponding to 8970 morphine equivalents 1 year after the event and 10 prescriptions of opioids corresponding to 3105 morphine equivalents 2 years after the event, a relative increase of 225% and 12.5%, respectively (Table 1 part B). Only 1 ED visit/hospitalization was not for pain (ED visits were distinct from the hospitalization visits).
The attending hematologist made the diagnosis of chronic pain based on the established definition by the ASH Guidelines, “…reports of ongoing pain present on most days over the past six months in either a single location or multiple locations.”1 The attending hematologist made the diagnosis because of the patient’s complaint of pain in multiple locations over the past year, including the arms and legs. After a diagnosis of chronic pain syndrome following a traumatic sexual event, multimodal treatment for chronic pain included monthly blood transfusion therapy, oral methadone at a starting dose of 10 mg per day, and counseling. The patient was referred to the Behavioral Hematology Oncology Program for diagnosis of anxiety and depression. Clinicians met with the patient for a 75-minute Health Psychology initial consultation/assessment session. The clinicians diagnosed the patient with a history of depression and current significant symptoms, including the patient’s history of traumatic experience resulting in posttraumatic stress disorder based on Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) criteria. The patient was referred for outpatient therapy regarding cognitive behavioral therapy strategies for depression, trauma, and anxiety, which was embraced by the patient. The patient was seen 22 times over 12 months, 13 of which were predominately for transfusions. The patient's baseline hemoglobin S% level was 44.1%. The goal of transfusion therapy was to keep hemoglobin S% at a maximum level of 40%. The mean pretransfusion hemoglobin S level was 36.7% after 12 months of treatment. The patient received 10 opioid prescriptions during the multimodal therapy corresponding to 3105 morphine equivalents, a relative reduction of 65.4% from 1 year after the trauma (Figure 1). The patient was off methadone at the end of treatment, which is 12 months of multimodal therapy. After completing the multimodal therapy for 12 months, the patient reported that they were without pain most days, thus no longer meeting the definition of chronic pain syndrome.
This work was conducted under the approval of the Vanderbilt University Medical Center's Institutional Review Board, Nashville, Tennessee (IRB 220379) and was performed with an approved Waiver of Consent.
For the first time, we demonstrate young adults with SCD who experienced sexual violence have a temporal onset of chronic pain syndrome. The underlying biological mechanisms of acute and chronic pain following a traumatic event are not well documented. However, a reasonable working hypothesis includes mental stress, fear, and anxiety that may trigger vaso-occlusive pain events.4 Khaleel et al demonstrated anticipating a noxious trigger will result in precapillary arteriolar constriction, leading to vasorestriction.5 Presumably, chronic stress associated with sexual violence may continue until addressed with multimodal therapy.
We elected to use a multimodal therapy to manage chronic pain syndrome after acute sexual trauma. Our multimodal treatment was based on the evidence that individuals with chronic pain have an increased prevalence of depression and anxiety and may benefit from counseling.6,7 The ASH guidelines on chronic pain management suggest that when shared decision making is applied, in conjunction with other measures, such as hydroxyurea having failed to control recurrent pain measures, then chronic monthly transfusions are reasonable.1 As a result, we initiated regular blood transfusion therapy to decrease the hemoglobin S level to at least 50% for ∼12 months in patients with hemoglobin SS.1 Last, we converted all morphine equivalent medication to methadone for chronic pain management and weaned the patient off methadone over ∼1 year.8 A limitation in our case series is that we cannot state with any degree of certainty which one of the multimodal interventions decreased the use of morphine equivalents over the treatment period.
In summary, we have presented evidence that sexual trauma is a risk factor for chronic pain syndrome in SCD and is preceded by an annual increase in morphine equivalents. With the automated use of the data warehouse of our electronic health records, we have now elected to improve surveillance of occult traumatic events in our adolescents and adults at our SCD Center.
Contribution: M.C. wrote the paper and analyzed data; J.B. contributed to clinical care of cases and analyzed data; M.R.D.B. wrote the paper, analyzed data, and contributed to the clinical care of cases; and K.W. analyzed data.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Michael R. DeBaun, Vanderbilt University Medical Center, 1211 Medical Center Dr, Nashville, TN 37212; e-mail: m.debaun@vumc.org.
References
Author notes
Contact the author for data sharing (e-mail: m.debaun@vumc.org).