Key Points
The prognosis of patients with advanced HL who achieved CMR after both 2 and 6 ABVD cycles is excellent without consolidation RT.
An additional benefit of consolidation RT of sites >5 cm is likely to be small and could not be proved for this small sample size.
Abstract
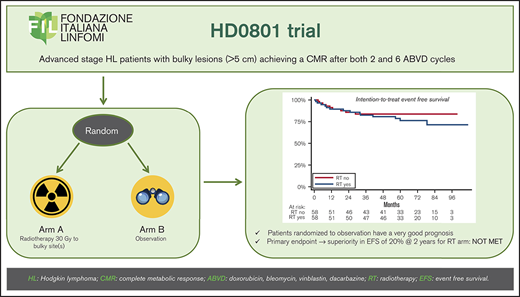
The role of consolidation radiotherapy (RT) for bulky lesions is controversial in patients with advanced-stage Hodgkin lymphoma who achieve complete metabolic response (CMR) after doxorubicin, bleomycin, vinblastine, dacarbazine (ABVD)–based chemotherapy. We present the final results of the Fondazione Italiana Linfomi HD0801 trial, which investigated the potential benefit of RT in that setting. In this phase 3 randomized study, patients with a bulky lesion at baseline (a mass with largest diameter ≥5 cm) who have CMR after 2 and 6 ABVD cycles were randomly assigned 1:1 to RT vs observation (OBS) with a primary endpoint of event-free survival (EFS) at 2 years. The sample size was calculated estimating an EFS improvement for RT of 20% (from 60% to 80%). The secondary end point was progression-free survival (PFS). One hundred sixteen patients met the inclusion criteria and were randomly assigned to RT or OBS. Intention-to-treat (ITT) analysis showed a 2-year EFS of 87.8% vs 85.8% for RT vs OBS (hazard ratio [HR], 1.5; 95% confidence interval [CI], 0.6-3.5; P = .34). At 2 years, ITT-PFS was 91.3% vs 85.8% (HR, 1.2; 95% CI, 0.5-3; P = .7). Patients in CMR randomly assigned to OBS had a good outcome, and the primary end point of a 20% benefit in EFS for RT was not met. However, the sample size was underpowered to detect a benefit of 10% or less, keeping open the question of a potential, more limited role of RT in this setting. This trial was registered at www.clinicaltrials.gov as #NCT00784537.
Introduction
The role of consolidation radiation therapy (RT) in advanced Hodgkin lymphoma (HL) is controversial, primarily because of conflicting results in randomized studies.1-3 Before the advent of functional imaging, the efficacy of consolidation RT was proved only in patient with a bulky mass at baseline4-6 or in those with a partial remission after chemotherapy.5,7 The uncertainty has increased in the modern era, with the more accurate assessment of response to chemotherapy with positron emission tomography (PET)-computed tomography (CT). Concerns for the increase of late effects, particularly secondary malignancies and cardiac diseases,8-10 have also led to a progressive decline in the use of RT. In fact, despite significant technological advances allowing for a meaningful reduction of the dose received by the healthy organs, the RT-related risk of long-term complications may not be completely abolished.11-17 Thus, an end-of-treatment PET-driven strategy has been proposed for advanced-stage HL by many research groups.
In phase 3 of the German Hodgkin Study Group HD15 study,18 consolidation RT was delivered only to patients with a positive PET-computed tomographic (CT) scan (Deauville score, ≥3) and a residual mass >2.5 cm at CT, given that the HD12 trial had shown that the outcome was not inferior for patients who did not receive consolidation RT of bulky lesions and achieved a complete response after 6 to 8 cycles of escalated-dose BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone).19
In the mid-2000s, 2 Italian collaborative research groups (Gruppo Italiano Terapie Innovative Linfomi [GITIL] and Fondazione Italiana Linfomi [FIL]) conducted 2 randomized trials investigating a response-adapted strategy in advanced HL treated with the ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine) regimen. Both trials included an early intensification in phase 2 in patients with PET positivity after 2 ABVD cycles and a second part of phase 3, in which patients with bulky disease at baseline (defined as the presence of a nodal mass >5 cm) and both interim (PET2) and end-of-chemotherapy PET negativity were randomly assigned to RT vs observation (OBS). Results of the early-intensification strategy of these 2 parallel studies have been reported, showing excellent outcomes in progression-free survival (PFS) for patients with early PET positivity who underwent either a BEACOPP-based intensification, per the GITIL HD0607 strategy,20 or autologous stem cell transplantation, per the FIL HD0801 strategy.21
The final results of the HD0607 study of the role of RT have been published recently. After the random assignment of 296 patients with PET negativity to RT (148) and OBS (148), the 6-year PFS was 92% (95% confidence interval [CI], 88-97) for RT vs 90% (95% CI, 85-95) for OBS, showing no benefit for consolidation RT (P = .48).22
We report the final results of the randomized phase 3 FIL HD0801 study.
Materials and methods
Study design and procedure
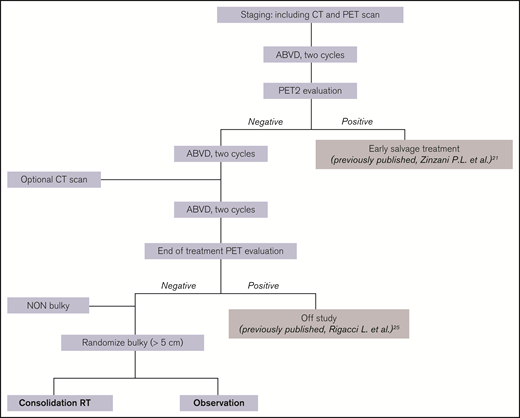
HD0801 was a multicenter study involving patients with newly diagnosed, advanced-stage HL, all receiving first-line ABVD treatment and undergoing an interim PET2 evaluation. This trial was designed to address 2 specific questions: whether an early PET-guided salvage treatment consisting of high-dose chemotherapy with a subsequent autologous bone marrow transplant could be considered safe and effective compared with data in the literature (phase 2) and whether patients with PET2 negativity would benefit from consolidation RT of areas of bulky lesions, provided they maintained PET negativity upon completion of the planned 6 ABVD courses (phase 3; Figure 1). The results of phase 2 of the study have been published.21
Patients
Patients aged 18 to 70 years were considered eligible if they had previously untreated, histologically documented, classic HL (with the exception of the nodular lymphocyte-predominant subtype) in clinical stages IIB to IV, according to Ann Arbor staging and at least 1 measurable target lesion (even if extranodal only). Patients were excluded from the study if they had a severe disease that impaired normal life, presented an active infection, or had inadequate liver or renal function, unless it was a result of the lymphoma. Those with a history of malignancy (except basal cell skin carcinoma and in situ carcinoma of the cervix) were considered ineligible.
Responses were primarily evaluated by centrally reviewed PET scan after 2 cycles of ABVD and at the end of the scheduled treatment plan, provided that all patients had undergone a complete staging workup, including a PET scan, before the start of treatment. The depth of response was graded according to the revised response criteria for malignant lymphomas.23 Details on PET central evaluation in the FIL HD0801 trial have been described.21
All local ethics committees at each participating center approved the study protocol and its amendments, in accordance with the Italian law and in compliance with the Declaration of Helsinki. Patients provided written informed consent before being included in the study.
Randomization and treatment plan
In phase 3 of the study, patients who had complete metabolic response (CMR), both at PET2 and at the end of chemotherapy (6 ABVD cycles) according to the criteria of Juweid et al24 and with at least 1 site of bulky disease at baseline (largest diameter measured on CT scan, ≥5 cm) were stratified according to baseline International Prognostic Score (IPS; ≤2 or ≥3) and then randomly assigned 1:1, using permuted blocks (length, 2 and 4), to either consolidation RT with the dose of 30 Gy in 2-Gy fractions or OBS within each strata.
End points
The primary end point was event-free survival (EFS), calculated from random allocation after PET response at the end of 6 ABVD cycles, until the date of disease progression, late serious treatment-related events, secondary cancers, or death from any cause. Secondary end points were PFS (measured until the date of lymphoma progression or death of any cause) and overall survival (OS; measured until the date of death of any cause).
Statistical methods
The sample size of this phase 3 study was estimated according to EFS difference favoring RT (primary end point). With a 2-sided α error of 0.05, 120 patients (60 in the RT and 60 in the OBS arms) were necessary for a statistical power of 80% to detect a 20% improvement in 2-year EFS (from 60% to 80%) in the group receiving RT compared with those who did not receive RT, assuming an accrual of 4 years and a minimum follow-up of 2 years from the enrollment of the last patient. Assuming that 40% of the total enrolled patients could have a bulky lesion at baseline and achieve a CMR after 2 and 6 ABVD, we initially planned the inclusion of 300 patients. However, after the first 300 enrolled patients, the proportion of bulky lesions achieving a CMR after 6 ABVD was only 23%. After a protocol amendment in January 2013, the total enrollment was increased to 520 cases, to obtain 120 cases that were randomly assigned to consolidation RT or OBS.
Time-to-event end points (EFS, PFS, and OS) were estimated with the Kaplan-Meier product-limit method. The main analysis was performed in the intention-to-treat (ITT) population, which included all randomly assigned patients. Differences between randomization groups were assessed by stratified log-rank test, and hazard ratios (HRs) were estimated with stratified Cox models. A per-protocol analysis (PP) was performed by excluding patients who did not receive the allocated treatment. Preplanned subgroup analyses according to age, disease stage, extranodal involvement, IPS, and Eastern Cooperative Oncology Group performance status were determined with Cox models, with adjustment for the stratification variable. The presence of any interaction was tested by including an interaction term between the randomly assigned group and the subgroup covariate. The size of the bulky lesion was then stratified into 3 subgroups (5-7, 7-10, and >10 cm) to explore any modification for the effect of RT. All reported P-values were 2 sided. Statistical analyses were performed with STATA software, version 13.0.
Results
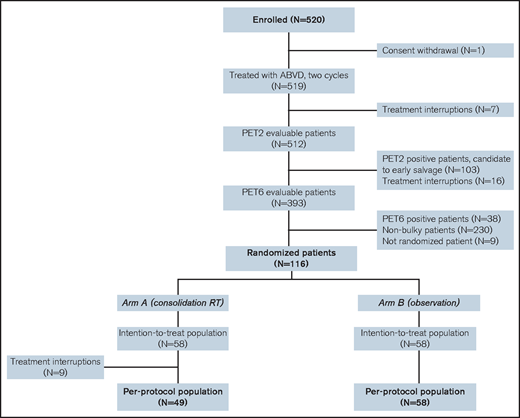
Overall, 520 patients were enrolled in the study and started ABVD treatment between September 2008 and April 2013 in 50 Italian centers. Of those patients, 512 (99%) underwent a PET2 scan, 1 patient withdrew consent before therapy, and 7 patients interrupted the treatment before the end of the second ABVD cycle. Among the 512 patients with an interim PET2 scan evaluated by central review, 409 (80%) were PET negative and 103 (20%) were PET positive. As stated by the protocol, all 409 patients with PET negativity received 4 more ABVD cycles. Among them, 16 patients interrupted therapy, and 393 were assessed for final response after 6 ABVD cycles. Of 393 patients, 38 were judged positive on the end-of-therapy PET scan and salvage therapy was initiated25 ; 355 were screened for entering the phase 3 part of the study; 230 had nonbulky lesions and 125 had bulky masses at baseline (Figure 2); 9 patients with bulky masses were not assigned to a study group (details in supplemental Table 1). Finally, 116 patients were randomly assigned to consolidation (RT arm, 58 patients) or OBS (OBS arm, 58 patients). The demographic and baseline disease characteristics of the randomly assigned patients are listed in Table 1. Nine patients allocated to RT did not receive consolidation therapy (details in supplemental Table 2) and were excluded from the PP analysis. None of the patients allocated to OBS received consolidation RT. The median size of initial bulky lesions was 8.15 cm in the RT arm and 8.25 cm in the OBS arm (range, 5-20 cm). The median RT dose was 30 Gy (range, 25-40 Gy). Overall, a protocol deviation in RT dose was recorded in 6 patients (1 patient treated with 25 Gy, 1 treated with 34 Gy, 2 treated with 36 Gy, and 2 treated with 40 Gy). The majority of the patients had a single bulky site (overall, 86%; 83% in the RT arm and 90% in the OBS arm); the mediastinum was the most frequent site (overall, 69%; 71% in the RT arm and 67% in the OBS arm).
Baseline characteristics of patients randomly assigned to RT vs OBS
| Factors . | RT . | OBS . | Total . |
|---|---|---|---|
| (n = 58) . | (n = 58) . | (n = 116) . | |
| Age, median (IQR) | 31.50 (26.00-39.75) | 29.50 (25.00-37.00) | 31.00 (25.00-39.00) |
| Sex | |||
| Male | 34 (59) | 30 (52) | 64 (55) |
| Female | 24 (41) | 28 (48) | 52 (45) |
| IPS | |||
| 0-2 | 33 (57) | 35 (60) | 68 (59) |
| ≥3 | 25 (43) | 22 (40) | 48 (41) |
| Histology | |||
| NS | 38 (66) | 39 (67) | 77 (66) |
| MC | 11 (19) | 5 (9) | 16 (14) |
| LD | 1 (2) | 3 (5) | 4 (3) |
| LR | 2 (3) | 5 (9) | 7 (6) |
| NA | 6 (10) | 6 (10) | 12 (10) |
| B symptoms | |||
| No | 14 (24) | 21 (36) | 35 (30) |
| Yes | 44 (76) | 37 (64) | 81 (70) |
| ECOG PS | |||
| 0 | 35 (60) | 38 (66) | 73 (63) |
| 1 | 16 (28) | 17 (29) | 33 (28) |
| 2 | 7 (12) | 3 (5) | 10 (9) |
| Stage | |||
| 2 | 19 (33) | 15 (26) | 34 (29) |
| 3 | 21 (36) | 20 (34) | 41 (35) |
| 4 | 18 (31) | 23 (40) | 41 (35) |
| Extranodal lesion sites | |||
| 0 | 39 (67) | 34 (59) | 73 (63) |
| ≥1 | 19 (33) | 24 (41) | 43 (37) |
| Involved nodal sites, median (IQR) | 6.00 (4.00-8.75) | 6.00 (4.00-8.00) | — |
| Number of bulky lesion sites | |||
| 1 | 52 (90) | 48 (83) | 100 (86) |
| 2 | 5 (9) | 6 (10) | 11 (9) |
| 3 | 1 (2) | 3 (5) | 4 (3) |
| 4 | 0 (0) | 1 (2) | 1 (1) |
| Bulky lesion site | |||
| Mediastinum | 41 (71) | 39 (67) | 80 (69) |
| Other sites | 17 (29) | 19 (33) | 36 (31) |
| Bulky site size, cm | |||
| <7 | 19 (33) | 18 (31) | 37 (32) |
| 7-10 | 16 (28) | 19 (33) | 35 (30) |
| ≥10 | 23 (40) | 21 (36) | 44 (38) |
| Factors . | RT . | OBS . | Total . |
|---|---|---|---|
| (n = 58) . | (n = 58) . | (n = 116) . | |
| Age, median (IQR) | 31.50 (26.00-39.75) | 29.50 (25.00-37.00) | 31.00 (25.00-39.00) |
| Sex | |||
| Male | 34 (59) | 30 (52) | 64 (55) |
| Female | 24 (41) | 28 (48) | 52 (45) |
| IPS | |||
| 0-2 | 33 (57) | 35 (60) | 68 (59) |
| ≥3 | 25 (43) | 22 (40) | 48 (41) |
| Histology | |||
| NS | 38 (66) | 39 (67) | 77 (66) |
| MC | 11 (19) | 5 (9) | 16 (14) |
| LD | 1 (2) | 3 (5) | 4 (3) |
| LR | 2 (3) | 5 (9) | 7 (6) |
| NA | 6 (10) | 6 (10) | 12 (10) |
| B symptoms | |||
| No | 14 (24) | 21 (36) | 35 (30) |
| Yes | 44 (76) | 37 (64) | 81 (70) |
| ECOG PS | |||
| 0 | 35 (60) | 38 (66) | 73 (63) |
| 1 | 16 (28) | 17 (29) | 33 (28) |
| 2 | 7 (12) | 3 (5) | 10 (9) |
| Stage | |||
| 2 | 19 (33) | 15 (26) | 34 (29) |
| 3 | 21 (36) | 20 (34) | 41 (35) |
| 4 | 18 (31) | 23 (40) | 41 (35) |
| Extranodal lesion sites | |||
| 0 | 39 (67) | 34 (59) | 73 (63) |
| ≥1 | 19 (33) | 24 (41) | 43 (37) |
| Involved nodal sites, median (IQR) | 6.00 (4.00-8.75) | 6.00 (4.00-8.00) | — |
| Number of bulky lesion sites | |||
| 1 | 52 (90) | 48 (83) | 100 (86) |
| 2 | 5 (9) | 6 (10) | 11 (9) |
| 3 | 1 (2) | 3 (5) | 4 (3) |
| 4 | 0 (0) | 1 (2) | 1 (1) |
| Bulky lesion site | |||
| Mediastinum | 41 (71) | 39 (67) | 80 (69) |
| Other sites | 17 (29) | 19 (33) | 36 (31) |
| Bulky site size, cm | |||
| <7 | 19 (33) | 18 (31) | 37 (32) |
| 7-10 | 16 (28) | 19 (33) | 35 (30) |
| ≥10 | 23 (40) | 21 (36) | 44 (38) |
Data are expressed as the number of patients (percentage of subgroup or total), unless otherwise stated. ECOG PS, Eastern Cooperative Oncology Group performance status; LD, lymphocyte depleted; LR, lymphocyte rich; MC, mixed cellularity’ NA, not available; NS, nodular sclerosis.
Survival analysis
Overall, for EFS, at least 1 event was recorded in 23 patients: 14 in the RT arm and 9 in the OBS arm. Seventeen patients experienced disease progression: 9 in the RT arm and 8 in the OBS arm. Table 2 describes in detail the recorded events according to randomization arm. Notably, 5 of 9 disease progressions in the RT arm were recorded among the 9 patients who did not receive the allocated RT treatment.
List of the events recorded in the 2 arms
| Event . | RT . | OBS . |
|---|---|---|
| Progression | 9* | 8 |
| In field/bulky site | 1 | 0 |
| Out of field | 6 | 6 |
| Not specified | 2 | 2 |
| Secondary neoplasm | 2 | 1 |
| Severe cardiac toxicity | 0 | 1 |
| Severe respiratory toxicity | 1 | 0 |
| Other severe toxicity | 2 | 0 |
| Death | 1† | 0 |
| Patients with at least 1 event | 14 | 9 |
| Event . | RT . | OBS . |
|---|---|---|
| Progression | 9* | 8 |
| In field/bulky site | 1 | 0 |
| Out of field | 6 | 6 |
| Not specified | 2 | 2 |
| Secondary neoplasm | 2 | 1 |
| Severe cardiac toxicity | 0 | 1 |
| Severe respiratory toxicity | 1 | 0 |
| Other severe toxicity | 2 | 0 |
| Death | 1† | 0 |
| Patients with at least 1 event | 14 | 9 |
Five of 9 relapsing patients did not receive consolidation RT.
The deceased patient did not receive consolidation RT (cause of death: myocardial infarction).
Overall, after a median follow-up of 71 months from the end-of-chemotherapy PET scan, only 1 death was recorded (a patient randomly assigned to the RT arm who did not receive consolidation RT).
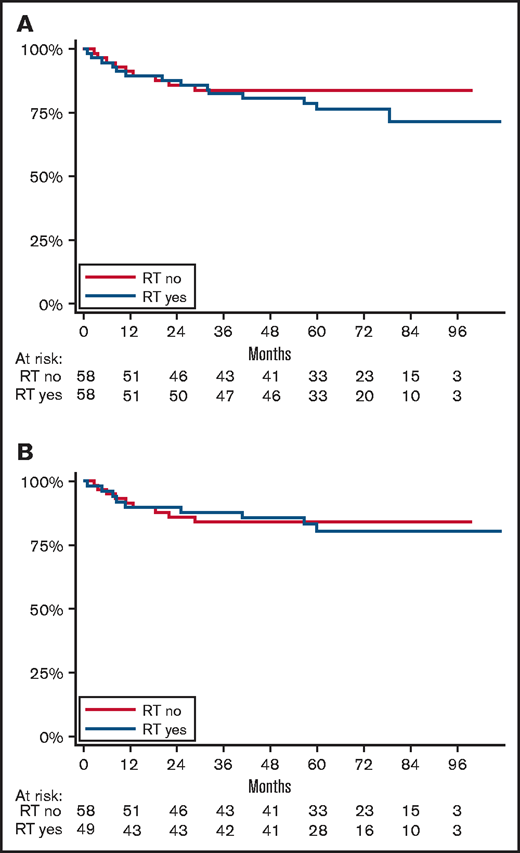
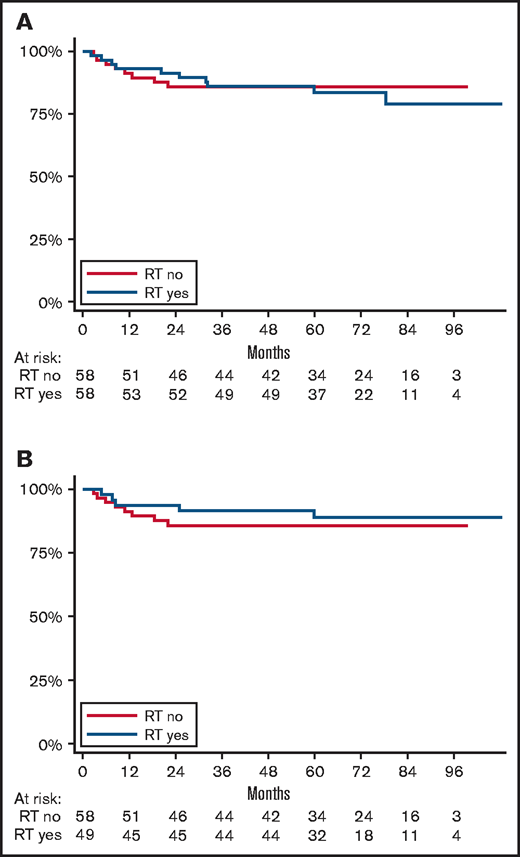
In an ITT analysis, 2-year EFS was 87.8% (95% CI, 76.0-94.0) in the RT arm vs 85.8% (95% CI, 73.6- 92.6) in the OBS arm. The HR was 1.5 (95% CI, 0.6-3.5; stratified log-rank test P = .34; Figure 3A).
EFS from the time of randomization. Determined according to ITT (A) or PP (B) analysis.
EFS from the time of randomization. Determined according to ITT (A) or PP (B) analysis.
The PP analysis showed a 2-year EFS of 89.6% (95% CI, 76.8-95.6) in the RT arm vs 85.8% (95% CI, 73.6% to 92.6%) in the OBS arm. The HR was 1.1 (95% CI, 0.4-2.8; stratified log rank test P = .7; Figure 3B).
In an ITT analysis, PFS at 2 years was 91.3% (95% CI, 80.3-96.3) in the RT arm vs 85.8% (95% CI, 73.6-92.6) in the OBS arm. The HR was 1.2 (95% CI, 0.5-3; stratified log rank-test P = .7; Figure 4A).
PFS from the time of randomization. Determined according to ITT (A) or PP (B) analysis.
PFS from the time of randomization. Determined according to ITT (A) or PP (B) analysis.
The PP analysis showed a 2-year PFS of 93.8% (95% CI, 81.9-98.0) in the RT arm vs 85.8% (95% CI, 73.6-92.6) in the OBS arm. The HR was 0.7 (95% CI, 0.2-2.1; stratified log rank test P = .5; Figure 4B).
In an ITT analysis, the unplanned 6-year estimates were similar in the RT and OBS arms for both EFS (76.4% vs 83.9%) and PFS (83.8% vs 85.8%).
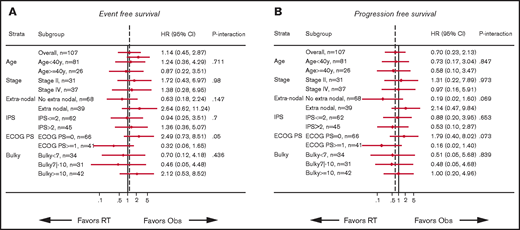
The subgroup analysis showed no modification of effects on EFS and PFS for any of the preplanned factors (Figure 5). The stratified analysis for the size of the bulky mass size showed no significant differences in the effect of RT that was related to different tumor burden (supplemental Figure 1).
By multivariable analysis (supplemental Table 3), age at diagnosis ≥50 years was significantly associated with a reduced EFS (HR, 5.45; 95% CI, 2.00-14.90; P < .001). No other factors showed a statistically significant association with the clinical outcomes.
Toxicity
Acute chemotherapy-related toxicity has been described in detail.21 Regarding RT, no acute toxicity events were detected, according to severe adverse event/suspected unexpected serious adverse reaction reporting.
Regarding late toxicity, only 7 events were recorded among the 116 randomly assigned patients. In details, 3 patients (2 in the RT arm and 1 in the OBS arm) had a second cancer (1 breast cancer, 1 follicular lymphoma, and 1 not specified), 1 patient (OBS arm) experienced a myocardial infarction, 1 patient (RT arm) had an inconclusive diagnosis of myelodysplastic syndrome and developed severe respiratory failure, 1 patient (RT arm) had persistent severe neutropenia (inconclusive for myelodysplastic syndrome), and 1 (RT arm) had severe neutropenia and thrombocytopenia.
Only 1 patient died of a myocardial infarction (the one who did not receive RT despite random assignment to the RT arm).
Discussion
Survival rates for advanced HL have substantially increased over the past 2 decades. Early response evaluation with PET2 proved to be an effective strategy in guiding the intensification of systemic agents in several prospective studies.20,21,26,27,28 Therefore, we could use a similar strategy for assessing the need for consolidation RT in advanced HL, based on the metabolic response at the end of chemotherapy.
Phase 3 of 2 similar (both Italian) studies20,21 was an investigation of the role of consolidation RT in patients with a bulky mass at baseline, who achieved CMR after the end of chemotherapy (6 ABVD cycles). The role of RT is debated because of concerns about late toxicity, as most of the bulky sites at diagnosis are in the mediastinum. In fact, the combination of anthracyclines and radiation is a known risk factor for late cardiac toxicity (especially coronary artery disease and chronic heart failure),29-31 and the risk of developing a secondary cancer (especially breast cancer in younger female patients).10,32 Although modern RT (doses and volume reduction, conformal treatment delivery) favors a better sparing of healthy tissues located in proximity to the target volume,11-16 the risk of long-term complications cannot be completely removed. Thus, the rationale for both studies was to investigate the possible omission of RT, maintaining the same tumor control probability with a reduced therapeutic burden.
The phase 3 GITIL HD0607 study of consolidation RT22 was designed with PFS as the primary end point. The results showed no differences between the RT and OBS arms in patients who had nodal masses larger than 5 cm at baseline and PET negativity at the end of ABVD chemotherapy, with a PFS at 6 years of 92% for RT vs 90% for OBS. The phase 3 FIL HD0801 study also failed to demonstrate a meaningful improvement in 2-year PFS, as well as in 2-year EFS, between patients in the RT arm vs the OBS arm.
A first consideration of the difference between the GITIL HD0607 study and the present study is the sample size and the frequency of bulky lesions. GITIL HD0607 investigators randomly assigned 296 patients of the 580 with bulky sites who had PET negativity at the end of chemotherapy (51%). In the FIL HD0801 study, we assigned 116 patients of the 355 with bulky sites who had PET negativity at the end of chemotherapy (32.6%). Despite the use of centralized PET imaging review and the same cutoff for the definition of bulky lesions in both studies, the proportion of bulky lesions among patients with PET negativity was significantly lower in the FIL HD0801 study. This difference in the prevalence of bulky presentations among patients with PET negativity is challenging to explain, given the same frontline therapeutic strategy and the proportion of patients achieving a CMR at the end of chemotherapy, slightly lower in our study (580 of 783 [74%], in the GITIL HD0607 study and 355 of 520 [68%], in the FIL HD0801 study). Second, the overall outcome was inferior in patients enrolled in the HD0801 trial, with an ITT 6-year PFS of 83.8% for RT and 85.8% for OBS, in comparison with 92% for RT and 90% for OBS in the GITIL HD0607 trial.22 The results could be caused partially by the higher proportion of patients with stage IIB disease randomly assigned in GITIL HD0607 compared with HD0801 (47% vs 29%, respectively). Last, the 2 studies had a different design: the primary end point of FIL HD0801 was EFS (not PFS, as it was in the GITIL trial), with the hypothesis of achieving a superior 2-year EFS with consolidation RT (80% vs 60%). The choice of EFS as the primary end point was justified by the consideration that all clinically relevant events, including toxicity, should be accounted for when comparing an additional treatment with potential toxicity, such as RT, to OBS. Moreover, EFS was the primary end point of several studies investigating the role of RT in advanced HL in the pre-PET era.4,6,7 Nevertheless, the assumptions underlying our study had at least 3 limitations: (1) the expected EFS for the OBS arm in patients in CMR, even in those with bulky lesions, was too low, compared with that in previous studies reporting that EFS rates were always >70%4 ; (2) in previous studies, the addition of RT provided a maximum benefit in EFS and PFS of 12% to 15%.4,6 (Therefore, our expectation of an absolute difference between RT vs no RT of 20% was too high.); and (3) RT-induced toxicity cannot be reliably estimated before 2 to 3 decades have passed since treatment. These limitations led to a small sample size, and made the study underpowered to detect (or exclude) differences in EFS and PFS <10%.
Despite these limitations, our trial showed that patients achieving CMR after ABVD cycles 2 and 6 had a good outcome (EFS and PFS at 2 years were 85.8%) without the addition of consolidation RT to bulky sites, confirming 2 previous studies in which the omission of RT was considered safe in the context of ABVD-based chemotherapy.22,27 Moreover, almost all relapses occurred outside the bulky sites, not just in the RT arm, but also in the OBS arm, and we did not detect any significant difference in RT impact across the different bulky lesion sizes (5-7, 7-10, or >10 cm) or in the pattern of relapse between irradiated vs nonirradiated areas. In contrast, the RT arm had a slightly superior outcome at 2 years, ranging from 2% (ITT EFS) to 8% (ITT PFS); however, any potential benefit of adding RT could not be proved by our study, because the small numbers did not confer enough power to detect a difference in such a limited entity. As an example, the randomized controlled trials that proved a significant PFS benefit with the addition of RT in early-stage HL included several hundred patients and achieved a small superiority, ranging from 6% to 12%.33-35 Therefore, considering the good outcome of patients who did not receive RT in our study, approaching the same rates as those in early-stage HL, any potential benefit of adding RT would probably be small and, to be demonstrated, would require a larger number of patients. Nevertheless, our study included only patients with a CMR after both 2 and 6 cycles. Therefore, we cannot provide any information on the role of RT in patients continuing ABVD with a positive finding after either 2 or 6 cycles.
Moreover, it should be noted that 9 patients assigned to RT did not receive the consolidation treatment, mostly for medical reasons, and 5 of them relapsed. It is well known that the size of the bulky lesion site affects the prognosis of patients with HL in both the early and the advanced setting.20,36 In the first GITIL HD0607 report,20 the researchers found bulky lesions larger than 7 cm to be predictive of worse PFS in multivariable analysis, regardless of treatment with consolidation RT or no treatment. The same cutoff was also identified in patients with early-stage HL in a collaborative study from American institutions, showing mitigation of the prognostic role of bulky masses >7 cm with the addition of RT (PFS at 4 years, >90% vs 55% for chemotherapy alone; P < .001).36 In the HD0801 trial, we were not able to demonstrate any beneficial role for RT in patients with bulky lesions >7 cm. Again, the study was considerably underpowered to address this question. (Overall, only 33 of 73 patients with a bulky mass >7 cm received consolidation RT).
A recent study from the collaborative International Lymphoma Radiation Oncology Group37 further highlighted the complex association between bulk (size and site) and clinical outcomes. The data showed a better OS in patients with mediastinal bulky lesion than in patients without bulky lesions. Moreover, the location of the bulky mass had a significant prognostic role. In fact, OS was higher in patients with a mediastinal location compared with those with a nonmediastinal location (92% vs 86% at 5 years; P < .01). This finding may be supported, at least partially, by several confounding factors. In fact, patients with advanced nonbulky lesions and those with bulky nonmediastinal sites are generally older and have associated bone involvement.
Looking at the results in detail, we cannot exclude that some patients would benefit from consolidation RT, and the next research step could be to merge similar studies with updated follow-up to perform a meta-analysis of individual patient data, with the goal of achieving more robust evidence on the role of consolidation RT among different risk subgroups.
In summary, phase 3 of the FIL HD0801 study did not meet its primary end point, failing to show a difference in EFS and PFS in patients receiving or not receiving consolidation RT of bulky sites at baseline. Moreover, the study showed that patients in CMR after 6 cycles of ABVD have a good prognosis without the addition of consolidation RT. However, these results are still not definitive and cannot directly demonstrate the noninferiority of OBS. In the future, the combination of clinical, radiological, and biological factors could better identify patients at higher risk of relapse. This strategy may better define upfront those who are included in future randomized trials with the goal of clarifying the potential role of consolidation RT, eventually with a dose deescalation, as has already been tested in early-stage HL38 and diffuse large B-cell lymphoma.39
Acknowledgments
The authors thank all the patients who participated in the study and their supportive families; the referring physicians and the supporting staff at all the participating clinical sites; all of the principal investigators in the other sites in Italy involved in this study: Michele Spina (Aviano), Vincenzo Liso (Bari), Giorgio Reguzzoni (Busto Arsizio), Emanuele Angelucci (Cagliari), Pier Paolo Fattori (Meldola), Giancarlo Latte (Nuoro), Caterina Stelitano (Reggio Calabria), Anna Lia Molinari (Rimini), Alteda Romano (Rome), Alberto Fabbri (Siena), Anna Marina Liberati (Terni), and Annalisa Luraschi (Verbania); and all of the nuclear medicine physicians in Italy who made a great effort toward the optimal conduct of this study: Alberto Pupi (Florence), Manuela Englaro (Udine), Manjola Dona (Prato), Arturo Chiti (Rozzano, Milan), Marilena Bello (Turin), Pierluigi Rossini (Brescia), and Giulia Montelatici and Enrico Pesciullesi (Arezzo).
Authorship
Contribution: U.R. and P.L.Z. conceived of and designed the study; all authors provided study material and collected and assembled the data; U.R., M.L., A.E., G.C., A.R.F., and P.L.Z. analyzed and interpreted the data; U.R., M.L., A.E., and A.R.F. wrote the manuscript; and all authors approved the final version of the manuscript.
Conflict-of-interest disclosure: U.R. served as a consultant to and was on the advisory board and the speakers bureau of AstraZeneca and served on the speakers bureau of Accuray. A.R. was a consultant to or was on the advisory board of Takeda, Italfarmaco, and Clinigen Healthcare. L.N. served as a consultant to or was on the advisory board of Takeda and Janssen-Cilag. A.P. served as a consultant to or was on the advisory board of Roche, MSD, Pfizer, and Sandoz and served on the speakers bureau of Roche, Gilead, and Bristol Myers Squibb. A.S. served as a consultant to or was on the advisory board of Arqule, Bayer, Bristol Myers Squibb, Eisai, Gilead, MSD, Pfizer, Sanofi, and Servier and was on the speakers bureau of AbbVie, Amgen, AstraZeneca, Arqule, Bayer, Bristol Myers Squibb, Celgene, Eisai, Gilead, Lilly, MSD, Novartis, Pfizer, Roche, Sandoz, Sanofi, Servier, and Takeda. M.T. served as a consultant to or was on the advisory board of Janssen-Cilag, Incyte, and AstraZeneca. F.Z. served as a consultant to or was on the advisory board of and received honoraria from AbbVie, Takeda, Roche, Amgen, Novartis, Gilead, Grifols, Celgene, and Janssen Cilag. E.A. served as a consultant to or was on the advisory board of Bristol, Incyte, Novartis, Pfizer, and Takeda. A.R.F. served as a consultant to or was on the advisory board of AstraZeneca and Roche and was on the speakers bureau of AstraZeneca, Roche, MSD, and Ipsen. P.L.Z. served as a consultant to or was on the advisory board of Verastem, Celltrion, Gilead, Janssen-Cilag, BMS, Servier, Sandoz, MSD, Immune Design, Celgene, Portola, Roche, Eusapharma, Kyowa Kirin, and Sanofi and was on the speakers bureau of Verastem, Celltrion, Gilead, Janssen-Cilag, BMS, Servier, MSD, Immune Design, Celgene, Portola, Roche, Eusapharma, and Kyowa Kirin. The remaining authors declare no competing financial interests.
Correspondence: Mario Levis, Department of Oncology, University of Torino, Via Genova 3, 10126 Torino, Italy; e-mail; mario.levis@unito.it.
References
Author notes
An oral presentation at the 38th ESTRO (European Society of Radiotherapy and Oncology) annual meeting, Milan, Italy, 26-30 April 2019.
For any request, please send an e-mail to the corresponding author (mario.levis@unito.it).
The full-text version of this article contains a data supplement.