Key Points
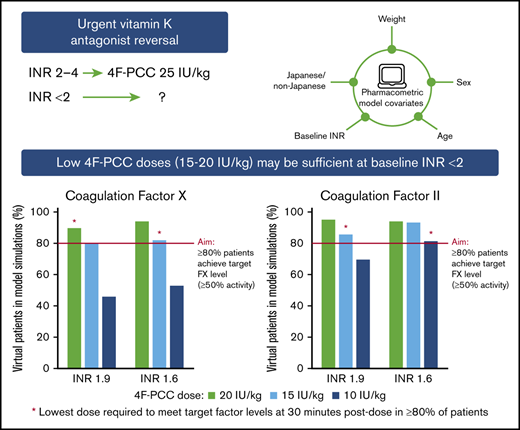
No indicated 4F-PCC dose for VKA reversal exists for INR <2, but 15-20 IU/kg achieves target FX and FII levels for INR <2 in modeling.
Our findings may guide future clinical studies that examine low-dose 4F-PCC at low baseline INRs.
Abstract
The indicated dose of 4-factor prothrombin complex concentrate (4F-PCC) for urgent vitamin K antagonist (VKA) reversal in patients with an international normalized ratio (INR) of 2 to 4 is 25 IU/kg, but there is no indicated dose for INR <2. We explored 4F-PCC dosing strategies for baseline INR <2. Clinical trial data were used to develop pharmacometric models for Factor X (FX) and FII, accounting for covariates including baseline INR. FX and FII levels over time were simulated for mean baseline INR levels of the clinical trial participants plus baseline INRs 3.1, 1.9, and 1.6. For each INR, 200 virtual male patients were simulated to evaluate 4F-PCC doses of 35, 25, 20, 15, 12.5, and 10 IU/kg. Given an elevated bleeding risk with VKA therapy in Japanese vs Western populations, results were stratified by Japanese and non-Japanese patients. Target levels of FX and FII were ≥50% activity at 30 minutes after dosing in ≥80% of patients. FX- and FII-time models were developed with 1088 FX observations from 193 patients and 1074 FII observations from 192 patients. Model-based simulations indicated that at baseline INR 3.1, ≥80% of patients achieved ≥50% FX and FII activity with 25 IU/kg and 20 IU/kg 4F-PCC, respectively; at baseline INR 1.9, corresponding doses were 20 IU/kg and 15 IU/kg 4F-PCC, and at baseline INR 1.6, corresponding doses were 15 IU/kg, and 10 IU/kg 4F-PCC. Trends in Japanese and non-Japanese patients were similar. In conclusion, low 4F-PCC doses (15-20 IU/kg) may be sufficient to achieve hemostatic levels of FX and FII in Japanese and non-Japanese patients with baseline INR <2.
Introduction
Despite increasing use of direct oral anticoagulants,1,2 vitamin K antagonists (VKAs) are still often prescribed for the treatment and prevention of thromboembolic events in various clinical situations.3,4 The use of VKAs is associated with bleeding complications.5,6 VKA reversal is required in cases of major bleeding or before urgent surgical or invasive procedures, with the goal of rapidly increasing the concentration of vitamin K–dependent coagulation factors to restore hemostasis.7
Four-factor prothrombin complex concentrates (4F-PCC) contain vitamin K–dependent coagulation factors (Factor II [FII], FVII, FIX, and FX), as well as natural anticoagulant proteins C and S,5 which enable rapid restoration of hemostasis in patients anticoagulated with VKAs. Along with vitamin K, they have become the preferred agents for urgent VKA reversal for acute major bleeding or before urgent surgery.8-11
In two large, phase 3, multicentre randomized controlled trials that supported the use of 4F-PCC over plasma, Sarode et al12 and Goldstein et al13 found that 4F-PCC led to rapid reversal of the international normalized ratio (INR) and effective hemostasis in patients receiving VKAs and experiencing major bleeding12 or those requiring urgent surgical procedures,13 respectively. More recently, Kushimoto et al14 conducted a phase 3 trial in Japanese patients and showed that 4F-PCC was an effective treatment for VKA reversal in cases of major bleeding or before urgent invasive procedures, leading to the approval of 4F-PCC (Kcentra, CSL Behring) in Japan.
Treatment guidelines worldwide recommend the use of 4F-PCC for urgent VKA reversal.9,11,15-17 The recommended dose of 4F-PCC for patients who require urgent VKA reversal because of major bleeding is based on INR at baseline, with 50 IU/kg indicated for INR >6, 35 IU/kg for INR 4 to 6, and 25 IU/kg for INR 2 to 4.18,19 However, cases of major bleeding at INR <2 have been observed; bleeding at lower INR values is a particular concern in intracranial or life-threatening hemorrhages and among the Japanese population because of an elevated bleeding risk in patients of Asian ethnicity.20-22 In Japan, guidelines for the management of atrial fibrillation recommend treatment with warfarin to achieve target INR of 1.6 to 2.6 in patients with nonvalvular atrial fibrillation who are age 70 years or older, and INR of 2 to 3 in those younger than age 70 years.23,24 In addition, a Japanese guideline indicates that the INR should be reversed to ≤1.35 as soon as possible in patients who present with intracerebral hemorrhage (ICH) while they are taking warfarin.16 Similarly, US guidelines recommend an INR target <1.4 in patients with VKA-associated ICH.25 Therefore, patients with INR <2 may still need warfarin reversal. However, there is no recommended strategy to guide the reversal of warfarin in patients with an INR <2; the optimal dose of 4F-PCC for patients with an INR <2 is currently unknown.
Although INR is conventionally used to monitor the anticoagulation effect of VKA, it has not been validated for the purpose of assessing the effectiveness of VKA reversal. Anticoagulation status may be more accurately predicted by plasma levels of VKA-dependent coagulation factors, of which FX and FII have been reported as important determinants of the antithrombotic effect of VKAs.26,27 In this study, we investigated optimal dosing of 4F-PCC for VKA reversal in patients with low INR by using statistical modeling and simulation. We used data from 3 key 4F-PCC phase 3 trials to develop pharmacometric models for FX and FII, which accounted for the effect of baseline INR (and other covariates) on response to 4F-PCC therapy. These models were then used to explore possible 4F-PCC dosing strategies for urgent VKA reversal in patients with a baseline INR <2. The results were also stratified by Japanese and non-Japanese patients to investigate any differences in the optimal dosing of 4F-PCC, given the elevated bleeding risk with VKA therapy observed in the Japanese population vs Western patients.20-22
Methods
Summary of model development and simulations
Modeling and simulation were conducted sequentially as follows. First, compartmental models were developed to describe the time course of FX and FII after administration of 4F-PCC by using observed data from clinical studies. Once the structure of the models was established, sources of between-patient variability were evaluated. The covariates tested were baseline INR, body weight, age, sex, and being Japanese or non-Japanese. The models were then validated by comparing simulations from the models with observed data and other previously published studies. Finally, simulations were performed using these models to identify relevant doses in virtual typical Japanese and non-Japanese patients for different baseline INR values.
Analysis of study data
Data for patients who received 1 dose of 4F-PCC (Kcentra/Beriplex; CSL Behring GmbH, Marburg, Germany) in 3 phase 3 clinical trials across >60 sites,12-14 were used to develop population pharmacokinetic models for FX and FII. The models were generated by using original observed data from studies conducted by Sarode et al,12 Goldstein et al,13 and Kushimoto et al.14 In each of the studies, plasma levels of coagulation factors were measured before 4F-PCC infusion (baseline) and at 0.5, 1, 3, 6, and 24 hours after 4F-PCC infusion (as well as at 12 hours after infusion in Sarode et al and Kushimoto et al). For all patients, observed baseline and post-dose FX and FII data for up to 24 hours were used to develop models. Initial evaluations of the models indicated that excluding samples below the lower limit of quantification (LLOQ) caused slight bias in the estimation of baseline factor levels. To ensure accurate characterization of the factor levels, baseline samples below the LLOQ were retained by imputing the LLOQ/2. Likelihood approaches were also attempted, but they led to numerical instability when estimating model parameters. INR values at baseline were incorporated as a covariate in the FX and FII models (INR values after infusion were not included in the models).
Model development for FX and FII
First, a model was developed to describe 4F-PCC dosing-related changes in FX over time, and then a similar model was developed for FII. Candidate structural models for FX and FII included 1-, 2-, and 3-compartment analyses. To improve model stability, a log-transform-both-sides approach was taken. Model parameters were assumed to be log-normally distributed. The model was fitted with a fixed zero-order infusion process, with duration of infusion fixed at the observed population median of 0.28 hours.
On determination of the FX base model, candidate covariates considered for inclusion were baseline INR, weight, age, sex, and Japanese (yes/no). Covariate inclusion and parameterization were guided by clinical and biological plausibility, as well as graphical and statistical assessments of the relationships between patient-specific random effects and the candidate covariates. After the final covariate model was established, the graphical and statistical assessments of the covariate relationships were performed again using the respective patient-specific random effects to ensure that no clinically or statistically significant (P < .01) covariate trends remained. The final covariate model was evaluated further by using standard diagnostic procedures and a standard prediction-corrected visual predictive check (pcVPC).28,29
Because of the similarity between the observed FX- and FII-time profiles, the model for FII was based on the developed FX model. The FII model was evaluated by applying the same methods as described for the FX model; modifications to the model were guided by these evaluations.
Simulation of 4F-PCC dosing effects on FX and FII levels
Applying the final covariate models for FX and FII, FX and FII levels over time were simulated for 3 baseline INR values of interest: 3.1, 1.9, and 1.6. For completeness, FX and FII levels over time were also simulated for mean baseline INR levels observed in the phase 3 studies (Table 1). For each baseline INR level, profiles for 200 virtual typical male patients were simulated for 5 4F-PCC doses: indicated dose (35 IU/kg for INR 4-6; 25 IU/kg for INR 2-4), 20 IU/kg, 15 IU/kg, 12.5 IU/kg, and 10 IU/kg (currently the lowest indicated dose of Kcentra is 25 IU/kg).18,19 The target level of both FX and FII was set as ≥50% activity (corresponding to ≥0.50 IU/mL; ie, within the normal reference range of 0.5-1.5 IU/mL30 ) at 30 minutes after dosing in at least 80% of the patients. For FII and FX, results were stratified by non-Japanese (male sex, weight 80 kg, age 70 years) and Japanese patients (male sex, weight 55 kg, age 80 years). These demographic characteristics were based on the average male patient enrolled in the phase 3 studies (Table 1). Uncertainty (expressed as a coefficient of variation) was estimated using 100 re-sampled parameter sets for the 200 virtual patients at each baseline INR level and dose.
Patient demographic characteristics for the 3 clinical trials used to develop pharmacometric models for FX and FII
| Characteristic . | Sarode et al12 (n = 98) . | Goldstein et al13 (n = 84)* . | Kushimoto et al14 (n = 11)† . |
|---|---|---|---|
| Sex, male, n (%) | 52 (53) | 48 (57) | 7 (64) |
| Mean age (SD), y | 70.3 (13.6) | 69.5 (13.4) | 79.5 (12.7) |
| Mean weight (SD), kg | 80.3 (26.0) | 80.7 (20.3) | 58.0 (11.8) |
| Mean baseline INR (SD) | 5.03 (3.21) | 3.54 (2.24) | 4.48 (2.74) |
| Characteristic . | Sarode et al12 (n = 98) . | Goldstein et al13 (n = 84)* . | Kushimoto et al14 (n = 11)† . |
|---|---|---|---|
| Sex, male, n (%) | 52 (53) | 48 (57) | 7 (64) |
| Mean age (SD), y | 70.3 (13.6) | 69.5 (13.4) | 79.5 (12.7) |
| Mean weight (SD), kg | 80.3 (26.0) | 80.7 (20.3) | 58.0 (11.8) |
| Mean baseline INR (SD) | 5.03 (3.21) | 3.54 (2.24) | 4.48 (2.74) |
For FX, mean number of samples per patient was 5.64; for FII, mean number of samples per patient was 5.59.
SD, standard deviation.
FX analysis included 84 patients; FII analysis included 83 patients.
Japanese patients.
All data management and post-processing procedures were performed in R version 3.3.1 (R Foundation, Vienna, Austria). Modeling was performed using NONMEM version 7.2 (ICON, Leopardstown, Ireland); simulations were performed in R using the mrgsolve package (Metrum Research Group, Tariffville, CT).
Results
Model development and validation
A total of 202 patients from the studies by Sarode et al,12 Goldstein et al,13 and Kushimoto et al14 received 1 dose of 4F-PCC. Patients with missing baseline INR measurements (n = 6) were excluded. In addition, patients with no FX data (n = 3) or no FII data (n = 4) were excluded from the respective factor analyses. Compromised samples (those that were hemolyzed, clotted, or lipemic) were excluded from the analyses (5.9% of all FX samples; 6.4% of all FII samples). For FX, 4.5% of all samples and 26% of baseline samples were below the LLOQ, and 3% of all FII samples and 15.6% of baseline FII samples were below the LLOQ. A total of 193 patients were included in the FX analysis, contributing 1088 baseline and post-infusion FX observations, and a total of 192 patients were included in the FII analysis, contributing 1074 baseline and post-infusion FII observations.
Patient demographic characteristics are provided in Table 1. Overall, 3 patients had an INR <2 before infusion with 4F-PCC; across all patients, the majority (94.8%) of INR values after infusion were <2. Note that in the 3 clinical trials, vitamin K (mainly IV) was administered to the majority of patients according to American College of Chest Physicians or local guidelines in addition to 4F-PCC.
The FX-time relationship after administration of 4F-PCC was characterized best by a 3-compartment model with zero-order input, with baseline FX incorporated as an intercept. A proportional residual error structure was used. Between-subject variability was estimated for baseline FX level, systemic clearance (CL), and central volume (Vc). In the final covariate model, baseline INR (before 4F-PCC infusion) was included as a covariate on baseline FX and CL, weight was a covariate for CL and Vc, age was incorporated into baseline FX and Vc, sex was a covariate for Vc, and a Japanese effect was apparent for baseline FX. Parameter estimates for the FX and FII models are provided in supplemental Table 1.
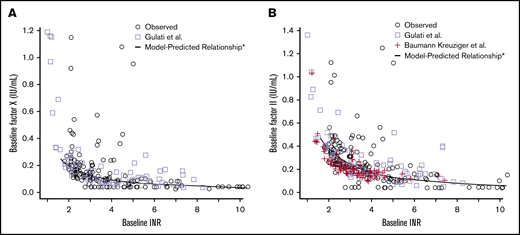
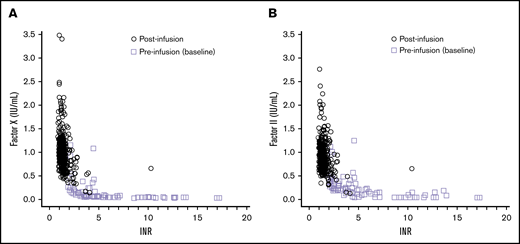
As expected, baseline INR was found to be an important covariate in the model, influencing 4F-PCC–related changes in FX and FII. Because we had only 3 patients with a baseline INR <2 in our analysis data set, we compared model-predicted relationships between a wide range of INR and factor levels at baseline with previously published data. Figure 1 illustrates that observed and model-predicted relationships between INR and factor levels at baseline are consistent with those reported in other clinical studies that investigated patients receiving warfarin therapy, including patients with INR <2.31,32 The prospective study by Baumann Kreuziger et al32 provided 38 FII samples from patients (n = 12) receiving chronic warfarin with unreliable INR testing (as a result of lupus anticoagulants or other conditions that would affect testing). Gulati et al31 analyzed FII levels in 70 samples and FX levels in 71 samples from patients who received VKA therapy. Those data showed a nonlinear relationship between baseline INR and baseline factor levels; a similar relationship is observed between post-infusion factor levels and post-infusion INR values (Figure 2).
Comparison of model prediction of FX and FII relationship with baseline INR vs published data to validate the models. (A-B) The FX relationship is shown in panel A and the FII relationship in panel B. The black line represents the baseline factor level–baseline INR relationship from model simulations. The observed data from the phase 3 trials (used to generate the models) is plotted with black circles. Observed data obtained from published studies, which investigated the FX-INR relationship (Gulati et al31 ) and the FII-INR relationship (Gulati et al31 and Baumann Kreuziger et al32 ) in patients are represented by lavender squares and red crosses, respectively. *Model predictions for baseline INR levels of 1.6 to 10.
Comparison of model prediction of FX and FII relationship with baseline INR vs published data to validate the models. (A-B) The FX relationship is shown in panel A and the FII relationship in panel B. The black line represents the baseline factor level–baseline INR relationship from model simulations. The observed data from the phase 3 trials (used to generate the models) is plotted with black circles. Observed data obtained from published studies, which investigated the FX-INR relationship (Gulati et al31 ) and the FII-INR relationship (Gulati et al31 and Baumann Kreuziger et al32 ) in patients are represented by lavender squares and red crosses, respectively. *Model predictions for baseline INR levels of 1.6 to 10.
Relationship of FX and FII levels with INR levels at baseline and post-4F-PCC. (A-B) FX data are shown in panel A and FII data in panel B. The observed data from the phase 3 trials (used to generate the models) is plotted with lavender squares representing baseline (pre-infusion) data and black circles representing post-infusion data.
Relationship of FX and FII levels with INR levels at baseline and post-4F-PCC. (A-B) FX data are shown in panel A and FII data in panel B. The observed data from the phase 3 trials (used to generate the models) is plotted with lavender squares representing baseline (pre-infusion) data and black circles representing post-infusion data.
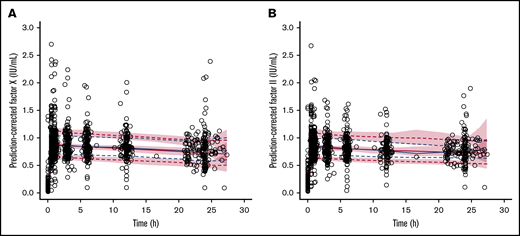
To evaluate whether 4F-PCC–related changes in FX and FII were well described with the developed models, we performed pcVPCs. Figure 3 shows pcVPCs for the FX and FII models, indicating that predicted factor levels are consistent with those observed in patients from the phase 3 trials.12-14 Additional diagnostic plots, including goodness-of-fit plots of developed FX and FII models are provided in supplemental Figures 1 and 2, respectively.
Prediction-corrected visual predictive checks to validate the models: comparison of FX- and FII-time modeled relationships using the final covariate models with observed data from the phase 3 trials. (A-B) FX-time relationship is shown in panel A and FII-time relationship in panel B. The black circles represent observed patient data from the phase 3 trials. The blue solid and dashed lines represent the observed median, 20th, and 80th percentiles, respectively. The red solid and dashed lines indicate the corresponding percentiles from the model simulations. The pink shaded regions are the 95% confidence intervals for the simulated percentiles.
Prediction-corrected visual predictive checks to validate the models: comparison of FX- and FII-time modeled relationships using the final covariate models with observed data from the phase 3 trials. (A-B) FX-time relationship is shown in panel A and FII-time relationship in panel B. The black circles represent observed patient data from the phase 3 trials. The blue solid and dashed lines represent the observed median, 20th, and 80th percentiles, respectively. The red solid and dashed lines indicate the corresponding percentiles from the model simulations. The pink shaded regions are the 95% confidence intervals for the simulated percentiles.
Exploration of dosing levels (simulations)
FX: non-Japanese virtual patients.
In patients with a baseline INR of 4.3 (mean INR in the phase 3 studies), 92% of those who received the indicated dose (35 IU/kg) of 4F-PCC achieved the target level of ≥50% FX activity at 30 minutes post-dose (Table 2). At a baseline INR of 3.1, 85% of patients achieved target FX activity with the indicated dose (25 IU/kg) of 4F-PCC (Table 2). For patients with a baseline INR of 1.9, this target was achieved by 93% who received 25 IU/kg and 89.5% who received 20 IU/kg 4F-PCC (Table 2). Similarly, for patients with a baseline INR of 1.6, the target FX activity was achieved by 97%, 94%, and 82% who received 25 IU/kg, 20 IU/kg, and 15 IU/kg, respectively (Table 2). Doses of 12.5 IU/kg and 10 IU/kg were insufficient to achieve the target of 80% of patients with ≥50% FX activity at any baseline INR.
Percent of virtual patients with simulated FX ≥50% activity at 30 minutes post-dose by baseline INR level and 4F-PCC dose
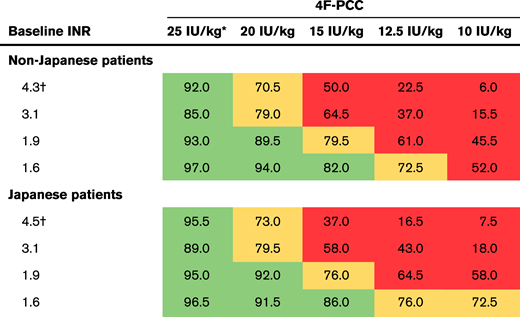 |
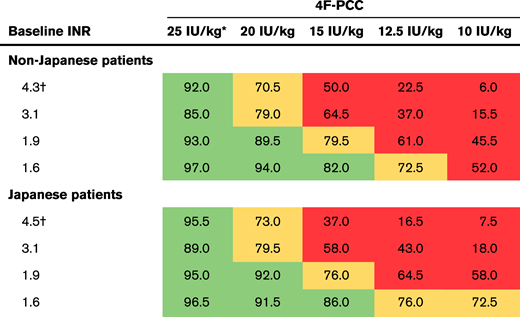 |
For each cell, n = 200. The colors indicate the percent of virtual patients with simulated FX activity of ≥50%: green, at least 80%; orange, 70% to <80%; red, <70%. When the percent of virtual patients with simulated FX activity of ≥50% was <25%, the level of uncertainty ranged from 12% to 24%; when the percent of patients was ≥25%, uncertainty ranged from 1% to 10%. Non-Japanese assumes male sex, weight 80 kg, age 70 years; Japanese assumes male sex, weight 58 kg, age 80 years.
A total of 35 IU/kg was used for the mean baseline INR of the phase 3 studies (4.3 and 4.5), consistent with the dose used in the study protocols (and the indicated 4F-PCC dose for INR 4-6); 25 IU/kg was used for all other baseline INR levels.
Mean baseline INR of patients from the phase 3 studies included in the development of the model.
FX: Japanese virtual patients.
Results for Japanese virtual patients had trends similar to those of non-Japanese virtual patients, but with slightly higher percentages of FX target achievement (Table 2). The target of ≥50% FX activity was achieved by 95.5% of Japanese patients with a baseline INR of 4.5 (phase 3 mean), who received the indicated dose of 35 IU/kg. For patients with an INR of 3.1, the target FX activity was achieved by 89% who received the indicated dose of 25 IU/kg (Table 2). The target FX level was obtained by 95% and 92% of patients with a baseline INR of 1.9 after treatment with 25 IU/kg and 20 IU/kg, respectively. For those with a baseline INR of 1.6, the target FX level was reached by 96.5%, 91.5%, and 86% of patients who received 4F-PCC at doses of 25 IU/kg, 20 IU/kg, and 15 IU/kg, respectively (Table 2). As for non-Japanese patients, 12.5 IU/kg and 10 IU/kg 4F-PCC doses were insufficient for achieving the target of 80% of patients with ≥50% FX activity at any baseline INR.
FII: non-Japanese virtual patients.
In patients with a baseline INR of 4.3 (phase 3 mean), 93.5% of those who received the indicated dose (35 IU/kg) of 4F-PCC achieved the target of ≥50% FII activity at 30 minutes post-dose (Table 3). In patients with a baseline INR of 3.1, 91% achieved target FII levels with the indicated dose of 25 IU/kg (Table 3). For patients with a baseline INR of 1.9, this target was achieved by 95.5%, 95.5%, and 86% who received 25 IU/kg, 20 IU/kg, and 15 IU/kg 4F-PCC, respectively (Table 3). Similarly, for patients with a baseline INR of 1.6, the target FII level was reached by 98.5%, 94%, 93.5%, 87.5%, and 82% of patients who received 4F-PCC at doses of 25 IU/kg, 20 IU/kg, 15 IU/kg, 12.5 IU/kg, and 10 IU/kg, respectively (Table 3).
Percent of virtual patients with simulated FII ≥50% activity at 30 minutes post-dose by baseline INR level and 4F-PCC dose
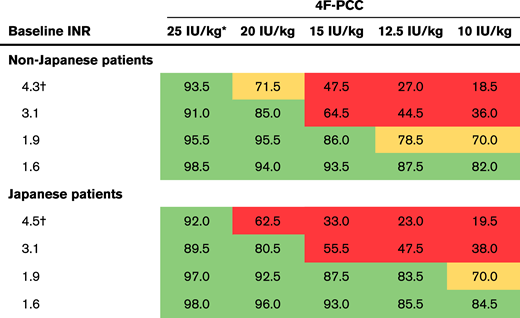 |
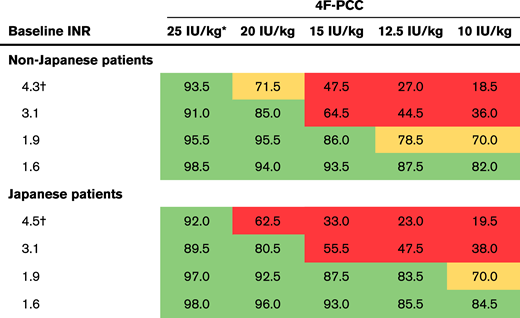 |
For each cell, n = 200. The colors indicate the percent of virtual patients with simulated FII activity of ≥50%: green, at least 80%; orange, 70% to <80%; red, <70%. When the percentage of virtual patients with simulated FII activity of ≥50% was <25%, the level of uncertainty ranged from 12% to 24%; when the percentage of patients was ≥25%, uncertainty ranged from 1 to 10%. Non-Japanese assumes male sex, weight 80 kg, age 70 years; Japanese assumes male sex, weight 55 kg, age 80 years.
35 IU/kg was used for the average baseline INR of the phase 3 studies (4.3 and 4.5), consistent with the dose used in the study protocols (and the indicated 4F-PCC dose for INR 4-6); 25 IU/kg was used for all other baseline INR levels.
Mean baseline INR of patients from the phase 3 studies included in the development of the model.
FII: Japanese virtual patients.
Trends in the Japanese virtual patients were similar to those observed in non-Japanese virtual patients, but with slightly higher rates of target achievement (Table 3). For patients with a baseline INR of 4.5 (phase 3 mean), 92% achieved the target FII activity level with the indicated dose (35 IU/kg) of 4F-PCC. The target of ≥50% FII activity was achieved by 89.5% of Japanese patients with a baseline INR of 3.1 who received 4F-PCC at a dose of 25 IU/kg. The target was reached by 97%, 92.5%, 87.5%, and 83.5% of patients with a baseline INR of 1.9 after treatment with 25 IU/kg, 20 IU/kg, 15 IU/kg, and 12.5 IU/kg 4F-PCC, respectively. In patients with a baseline INR of 1.6, the target FII level was reached by 98%, 96%, 93%, 85.5%, and 84.5% of patients who received 4F-PCC at doses of 25 IU/kg, 20 IU/kg, 15 IU/kg, 12.5 IU/kg, and 10 IU/kg, respectively (Table 3).
Discussion
We observed a dose-dependent relationship between 4F-PCC, INR, and achievement of target activity levels of FX and FII. Our results showed that the indicated dose of 25 IU/kg (for INR 2-4) is effective in achieving target FX and FII levels of ≥50% at 30 minutes post-dose in ≥80% of patients. Model-based simulations showed that in patients with baseline INRs of 1.6 to 1.9, 15 to 20 IU/kg 4F-PCC may be sufficient to reach the target FX levels, and 10 to 15 IU/kg may be sufficient to achieve the FII target levels. The findings of this analysis also show similar trends between non-Japanese and Japanese patients, with only a marginal difference in the relationship between 4F-PCC dose, INR, and achievement of the target levels of FX and FII.
In this analysis, we developed novel models of FX and FII kinetics after administration of 4F-PCC, which used baseline and post-infusion coagulation factor levels and incorporated baseline INR as a covariate. The model predictions were in agreement with both our observed data and other published data for a wide range of FX and FII levels vs INR values at baseline. The models exhibited acceptable goodness-of-fit properties, which enabled exploration of dosing via simulation. Furthermore, results from our simulations indicated that the currently recommended 4F-PCC doses for INR 4 to 6 (35 IU/kg) and INR 2 to 4 (25 IU/kg), as demonstrated in this analysis by the baseline INR of 3.1,18,19 would be sufficient to achieve target levels of both FX and FII, thereby providing further support for the developed models.
The key 4F-PCC clinical trials studied patients with baseline INR ≥2; however, cases of major bleeding at baseline INR <2 have been observed. There is a lack of data on PCC dosing for patients treated with VKAs who experience bleeding or require urgent reversal before surgery or urgent procedure with INR <2. Our results suggest that doses <25 IU/kg may be sufficient to provide hemostatic factor levels in patients with baseline INR <2 who experience bleeding. Similarly, a study investigating a low-dose 4F-PCC strategy (15 IU/kg) for warfarin reversal in patients with baseline INR 1.6 to 1.9 who experienced ICH found that none of these patients experienced hematoma expansion, and 85% of patients achieved a target INR of ≤1.3, suggesting that low-dose 4F-PCC may be effective in patients with baseline INR <2.33 Moreover, lower doses may provide the advantage of reduced treatment costs and potentially lower thrombotic events in high-risk patients.
Because VKAs influence the concentrations of coagulation FII, FVII, FXI, and FX, it has been suggested that direct measurement of these factors could provide an additional benefit to INR in assessing the extent of anticoagulation. Our analysis shows a nonlinear relationship between levels of FX and FII and INR values, not only at baseline but also after 4F-PCC treatment. It should be noted that post-infusion INR values stay within a small range (<2), whereas factor levels show considerable variability between patients. These findings are consistent with previous studies that found levels of coagulation FII, FVII, and FX vary in patients with similar INRs who are receiving warfarin therapy, and that there is a nonlinear relationship between FII and FX levels and INR.34,35
Depletion of both FX and FII is important for the clinical efficacy of VKAs.26 FII concentration was shown to be the greatest determinant of thrombin generation in plasma obtained from patients who are receiving a VKA, which suggests that the anticoagulant effect of VKA therapy is primarily mediated by influencing the FII level.36 Similarly, a rabbit study showed that the decline in levels of FII, and to a lesser extent FX, drives the antithrombotic effect of VKAs.26 Studies have also shown that bleeding and thromboembolic complications in VKA-treated patients correlate well with the FII level, and this correlation is stronger than with prothrombin time, which is mainly driven by FVII levels.37,38 Along with FII, FX is also an important determinant of VKA anticoagulation. A ROTEM study using platelet-poor and platelet-rich plasma found that during deficiency of vitamin K–dependent factors, the concentrations of FII and FX may be more critical for hemostasis than concentrations of FVII or FIX.39 Similarly, a ROTEM study using patients who were taking warfarin found that FX and FII are more important for clot formation than FVII or FIX, and their levels better reflect the anticoagulant effect of VKAs.40 Notably, a dose of only 10 IU/kg was needed for >80% of patients with INR 1.6 to reach the FII target level compared with 15 IU/kg for FX; however, this finding should be considered with caution to avoid overinterpretation of modeling analysis.
The target level of ≥50% was based on our clinical experience and is consistent with published studies showing factor activity levels after successful VKA reversal30 and the levels necessary to avoid bleeding episodes in patients with congenital factor deficiencies.41,42 However, higher factor activity (>80%) may be more appropriate in some surgical situations or with intracranial bleeding.
Several studies have suggested that Japanese patients receiving VKAs are at greater risk of bleeding than Western patients,20-22 and hemorrhagic events have been observed at INR <2 in Japanese patients who were taking warfarin.43 Our results suggest that 4F-PCC at 15 IU/kg and 20 IU/kg may be effective for VKA reversal in most Japanese patients with baseline INR 1.6 and 1.9, respectively. There was a marginal population effect (Japanese patients vs non-Japanese patients) in the covariate model. However, because only 11 Japanese patients were included in the analyses, there was insufficient information to suggest different dosing regimens for Japanese and non-Japanese patients with respect to FX and FII.
A limitation of our analysis was that the lowest observed baseline INR in the phase 3 trials was 1.8; thus, the simulations for patients with baseline INR between 1.6 and 1.8 were extrapolations, and appropriate caution should be used when drawing conclusions from these results. However, our model-predicted relationship between INR and factor levels is consistent with data from previously reported studies, which included patients with INR <2 at baseline. Although the findings from this study may be used to gain insight on dosing considerations for patients requiring urgent VKA reversal, they may not necessarily be suitable for individualizing doses because developed models may not account for disease indication, severity of disease and/or bleeding, comorbidities, and concomitant medications. Thus, although our results may be used as a general guide for dosing considerations, clinical judgment needs to be used when considering appropriate treatment for individual patients. Additional clinical studies in patients with INR <2 are needed. In addition, to examine the FX and FII response levels stratified by 4F-PCC dose, baseline INR, and Japanese or non-Japanese patients, all other covariates such as sex and age were fixed. Using only males age 70 or 80 years in the simulations may limit extrapolation of the results to women and different age groups.
In conclusion, we developed novel pharmacometric models that were used to explore effective 4F-PCC dosing strategies for urgent VKA reversal in patients with baseline INR <2. Model-based simulations revealed that low doses of 4F-PCC (15-20 IU/kg) may be sufficient to achieve target levels of coagulation FX and FII at 30 minutes after infusion in both Japanese and non-Japanese patients with baseline INR <2. This study, in conjunction with previously published studies, offers an innovative, model-informed segue into future studies that aim to examine the safety and efficacy of low-dose 4F-PCC for VKA reversal in patients with baseline INR <2 in a clinical setting.
CSL will only consider requests to share individual patient data (IPD) received from systematic review groups or bona fide researchers. CSL will not process or act on IPD requests until 12 months after article publication on a public website. An IPD request will not be considered by CSL unless the proposed research question seeks to answer a significant and unknown medical science or patient care question. Applicable country-specific privacy and other laws and regulations will be considered and may prevent sharing of IPD. Requests for use of the IPD will be reviewed by an internal CSL review committee. If the request is approved and the researcher agrees to the applicable terms and conditions in a data sharing agreement, IPD that has been appropriately anonymized will be made available. Supporting documents including the study protocol and the statistical analysis plan will also be provided if available. For information on the process and requirements for submitting a voluntary data sharing request for IPD, please contact CSL at clinicaltrials@cslbehring.com.
Acknowledgments
The authors thank Helen Kastrissios and Kris Jamsen of Certara for their help with analyses in the study and for their contributions to writing this manuscript. Leigh O’Connor-Jones (Fishawack Communications Ltd.) provided medical writing support by helping to develop the initial draft with direction from the authors, assemble tables and figures, collate authors’ comments, and provide grammatical editing and reference expertise.
This study was funded by CSL Behring.
Authorship
Contribution: A.M. and M.P. helped conceive and design the study; A.M., M.A.T., and M.P. acquired the data; and R.S., K.F., M.Y., M.A.T., A.M., M.P., and A.C. analyzed and/or interpreted data and approved the final version of the manuscript before it was submitted.
Conflict-of-interest disclosure: R.S. served as a consultant for CSL Behring, Octapharma, and Portola and received institutional research funding from Siemens. M.A.T. and A.M. are employees of CSL Behring. M.P. is an employee of Certara. A.C. reports that his institution has received research funding on his behalf from Alexion, Bayer, Bioverativ, Novo Nordisk, Pfizer, Shire, Spark, and Syntimmune and that he has served as a consultant for Genzyme, Kedrion, and Synergy. M.Y. has received lecture fees from Bayer, Bristol-Myers Squibb, and Daiichi-Sankyo. K.F. reports that his institution has received research funding on his behalf from Baxalta/Shire, Bayer, Pfizer, CSL Behring, Novo Nordisk, Biogen/Bioverativ, Kaketsuken/KM Biologics, Japan Blood Products Organization, and Chugai Pharmaceutical; he has served as a consultant for Baxalta/Shire, Bayer, CSL Behring, Novo Nordisk, Biogen/Bioverativ, Kaketsuken/KM Biologics, Chugai Pharmaceutical, SRL Inc., LSI Medience, Sekisui Medical, and Sysmex; and he has served as a speaker for Baxalta/Shire, Bayer, Pfizer, CSL Behring, Novo Nordisk, Biogen/Bioverativ, Kaketsuken/KM Biologics, Chugai Pharmaceutical, Siemens, Sekisui Medical, Fujirebio Inc., Torii Parmaceutical, MSD, Sysmex, Ortho Clinical Diagnostics, and Daiichi Sankyo.
Correspondence: Ravi Sarode, Department of Pathology and Internal Medicine (Hematology/Oncology), The University of Texas Southwestern Medical Center, 5323 Harry Hines Blvd, Dallas, TX 75390; e-mail: ravi.sarode@utsouthwestern.edu.
References
Author notes
The full-text version of this article contains a data supplement.