Key Points
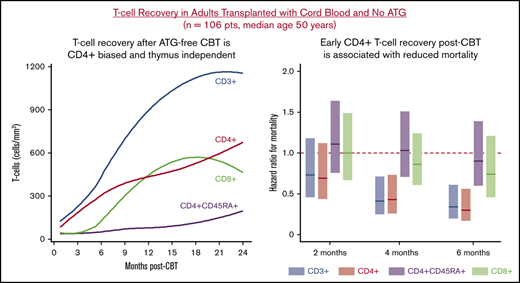
ATG-free CBT in adults is associated with rapid CD4+-biased, thymus-independent, T-cell reconstitution.
Recovery of CD4+ T cells and T-cell function is associated with improved survival in adult CBT recipients.
Abstract
Quality of immune reconstitution after cord blood transplantation (CBT) without antithymocyte globulin (ATG) in adults is not established. We analyzed immune recovery in 106 engrafted adult CBT recipients (median age 50 years [range 22-70]) transplanted for hematologic malignancies with cyclosporine/mycophenolate mofetil immunoprophylaxis and no ATG. Patients were treated predominantly for acute leukemia (66%), and almost all (96%) underwent myeloablation. Recovery of CD4+ T cells was faster than CD8+ T cells with median CD4+ T-cell counts exceeding 200/mm3 at 4 months. Early post-CBT, effector memory (EM), and central memory cells were the most common CD4+ subsets, whereas effector and EM were the most common CD8+ T-cell subsets. Naive T-cell subsets increased gradually after 6 to 9 months post-CBT. A higher engrafting CB unit infused viable CD3+ cell dose was associated with improved CD4+ and CD4+CD45RA+ T-cell recovery. Cytomegalovirus reactivation by day 60 was associated with an expansion of total, EM, and effector CD8+ T cells, but lower CD4+ T-cell counts. Acute graft-versus-host disease (aGVHD) did not significantly compromise T-cell reconstitution. In serial landmark analyses, higher CD4+ T-cell counts and phytohemagglutinin responses were associated with reduced overall mortality. In contrast, CD8+ T-cell counts were not significant. Recovery of natural killer and B cells was prompt, reaching medians of 252/mm3 and 150/mm3 by 4 months, respectively, although B-cell recovery was delayed by aGVHD. Neither subset was significantly associated with mortality. ATG-free adult CBT is associated with robust thymus-independent CD4+ T-cell recovery, and CD4+ recovery reduced mortality risk.
Introduction
Cord blood (CB) is a valuable alternative hematopoietic stem cell (HSC) source for patients who lack suitable adult donors, especially racial and ethnic minorities.1,2 Double-unit CB grafts have successfully extended cord blood transplantation (CBT) to larger children and adults,3 and both single- and double-unit CBT has been associated with potent graft-versus-leukemia (GVL) effects,4,5 low rates of chronic graft-versus-host disease (GVHD),6-8 and high rates of disease-free survival in patients with hematologic malignancies.4-6,8,9 CBT, however, has also been associated with delayed immune reconstitution compared with T-cell replete HLA-matched adult donor allografts with multiple reports of high infection rates early posttransplant.10-13
CB grafts contain low numbers of progenitor stem and immune cells compared with adult donor HSC grafts.14 In addition, CB-derived lymphocyte populations have unique phenotypic and immunological properties, including almost exclusively naive T cells that do not transfer immune memory.15,16 Although these CB graft attributes could contribute to delayed immune reconstitution, many previous CBT series have included antithymocyte globulin (ATG), a platform that has detrimental effects on both immune reconstitution and survival after CBT.17-22 Notably, low ATG exposure or omission of ATG has been associated with rapid thymus-independent T-cell expansion and robust immune reconstitution in pediatric CBT recipients.19,22-25 In contrast to children, however, relatively little is known about immune reconstitution after ATG-free CBT in adults.12,26-30
Herein, we report the kinetics of immune reconstitution in a large cohort of adult CBT recipients transplanted for hematologic malignancies at a single center without ATG. We also analyzed the impact of patient, graft, and early posttransplant factors on immune recovery, as well as the immune variables associated with improved survival. Our hypothesis was that, similar to pediatric series, ATG-free adult CBT is associated with prompt immune reconstitution and that early T-cell recovery improves survival post-CBT.
Methods
Patient and transplant characteristics
All consecutive adult patients ≤70 years old who underwent first allogeneic transplantation using single- or double-unit CB grafts for the treatment of hematologic malignancies at Memorial Sloan Kettering Cancer Center (MSKCC) between April 2012 and May 2016 were eligible for analysis (n = 114). Those who did not achieve CB-derived engraftment (n = 4) or had no immune reconstitution assays performed due to development of fatal early posttransplant complications before day 30 (n = 4) were excluded. Of the 106 evaluable patients, 93 were treated on Institutional Review Board (IRB)–approved protocols (#NCT00739141, #NCT01682226, and #NCT00387959). The remaining 13 patients were treated off protocol due to either protocol ineligibility (n = 8) or insurance denial for clinical trials in otherwise eligible patients (n = 5).
CB units were at least 4/6 HLA-A, -B antigen, -DRB1 allele matched to the recipient, and each unit had a cryopreserved total nucleated cell (TNC) dose ≥1.5 × 107/kg. High-resolution HLA typing, CD34+ cell dose, CB quality, and bank of origin were also considered in unit selection as previously detailed.31 Some patients also received mobilized peripheral blood-derived haploidentical CD34+ cells as a myeloid bridge prior to CB engraftment (#NCT01682226).
Most patients received myeloablative conditioning (outlined in Table 1). GVHD prophylaxis was with cyclosporine-A/mycophenolate mofetil, and no patient received ATG. Granulocyte colony-stimulating factor was given starting day +7. Cytomegalovirus (CMV)-seropositive patients were monitored by quantitative polymerase chain reaction as of day +14 posttransplant. Preemptive antiviral therapy was given upon detection of any level of CMV viremia.
Patient and graft characteristics (n = 106)
| Variable . | Value . |
|---|---|
| Median age (range), y | 50 (22-70) |
| Male, n (%) | 55 (52) |
| Median weight (range), kg | 80 (36-138) |
| Recipient CMV+, n (%) | 59 (56) |
| Diagnosis, n (%) | |
| Acute leukemia (AML/ALL/other) | 70 (66) |
| MDS/MPN | 14 (13) |
| Lymphoma (NHL/HD) | 22 (21) |
| Conditioning, n (%)* | |
| High intensity | 1 (1) |
| Intermediate intensity | 101 (95) |
| Nonmyeloablative | 4 (4) |
| Donor-recipient 8-allele HLA match,† median (range) | 5 (3 to 7) |
| Infused TNC dose × 107/kg,† median (range) | 2.35 (1.23-5.31) |
| Infused viable CD34+ dose × 105/kg,† median (range) | 1.18 (0.18-4.08) |
| Infused viable CD3+ dose × 106/kg,† median (range) | 3.34 (0.45-10.61) |
| Graft composition, n (%)‡ | |
| dCB | 45 (42) |
| dCB-haploCD34+ | 59 (56) |
| sCB-haploCD34+ | 2 (2) |
| Variable . | Value . |
|---|---|
| Median age (range), y | 50 (22-70) |
| Male, n (%) | 55 (52) |
| Median weight (range), kg | 80 (36-138) |
| Recipient CMV+, n (%) | 59 (56) |
| Diagnosis, n (%) | |
| Acute leukemia (AML/ALL/other) | 70 (66) |
| MDS/MPN | 14 (13) |
| Lymphoma (NHL/HD) | 22 (21) |
| Conditioning, n (%)* | |
| High intensity | 1 (1) |
| Intermediate intensity | 101 (95) |
| Nonmyeloablative | 4 (4) |
| Donor-recipient 8-allele HLA match,† median (range) | 5 (3 to 7) |
| Infused TNC dose × 107/kg,† median (range) | 2.35 (1.23-5.31) |
| Infused viable CD34+ dose × 105/kg,† median (range) | 1.18 (0.18-4.08) |
| Infused viable CD3+ dose × 106/kg,† median (range) | 3.34 (0.45-10.61) |
| Graft composition, n (%)‡ | |
| dCB | 45 (42) |
| dCB-haploCD34+ | 59 (56) |
| sCB-haploCD34+ | 2 (2) |
ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; HD, Hodgkin disease; MDS, myelodysplastic syndrome; MPN, myeloproliferative neoplasm; NHL, non-Hodgkin lymphoma.
High-intensity myeloablative conditioning was with cyclophosphamide 120 mg/kg, fludarabine 75 mg/m2, and total body irradiation (TBI) 1320 cGy; intermediate-intensity myeloablative was with cyclophosphamide 50 mg/kg, fludarabine 150 mg/m2, thiotepa 5 to 10 mg/kg, and TBI 400 cGy33 ; nonmyeloablative included cyclophosphamide 50 mg/kg, fludarabine 150 mg/m2, and TBI 200 cGy (n = 3), or fludarabine 150 mg/m2 and TBI 400 cGy (n = 1).
Engrafting CB unit.
Fifty-nine double-unit CB (dCB) grafts and 2 single-unit CB (sCB) grafts were supplemented with haploidentical CD34+ cells to provide a myeloid bridge prior to CB engraftment.
This study was performed with MSKCC IRB approval.
Immune reconstitution monitoring
Immune reconstitution monitoring was per standard MSKCC clinical practice and not influenced by protocol enrollment. Flow cytometric immunophenotyping for the monitoring of absolute lymphocyte count (ALC) and lymphocyte subset recovery was performed prospectively on fresh whole blood samples at the MSKCC Clinical Immunology Laboratory using BD FACS Canto II and BD FACS Canto 10 color flow cytometers. Until April 2014, analyzed lymphocyte subsets included total T cells (CD3+), total CD4+, CD4+45RA+, and CD8+ T cells, natural killer (NK; CD3−CD56+CD16+), and B cells (CD19+). Since May 2014, subset analysis of CD4+ and CD8+ naive (CCR7+CD45RA+), central memory (CM; CCR7+CD45RA−), effector memory (EM; CCR7−CD45RA−), effector (CCR7−CD45RA+), and activated (CD38+HLADR+) T cells, and naive (CD27−IgD+), nonswitched memory (CD27+IgD+), switched memory (CD27+IgD−), transitional (CD24+CD38+), and plasmablast (CD27+CD20−CD38+) B cells was performed. T-cell proliferative responses to mitogen phytohemagglutinin (PHA) were assessed by measuring 3H-thymidine incorporation. Assessments were usually performed at days 30, 60, 120, 180, 270, 1 year, 18 months, and 2 years post-CBT. Immune recovery data were censored at the time of second allogeneic transplantation (n = 1) or after infusion of viral-specific cytotoxic T cells (n = 5; 4 CMV specific, 1 Epstein-Barr virus specific).
Statistical analysis
Acute graft-versus-host disease (aGVHD) was diagnosed clinically with histologic confirmation when possible and was graded according to International Bone Marrow Transplant Registry criteria.32 CMV reactivation was defined as detection of CMV DNA by quantitative polymerase chain reaction regardless of the viremia level. Transplant-related mortality (TRM) was defined as death from any cause other than disease relapse or progression. The cumulative incidence of aGVHD, CMV reactivation, relapse, and TRM was calculated in the competing risks framework considering relapse/death without developing aGVHD, death without CMV reactivation, TRM, and relapse as the competing events, respectively. Overall survival (OS) and progression-free survival estimates were calculated using Kaplan-Meier methodology.
Loess-smoothed curves were estimated to visually inspect immune recovery trends over time. The association between baseline or early posttransplant factors and immune variables was investigated with linear mixed effects models. Immune recovery data were natural log transformed before the analysis. The mixed effects models contained linear and quadratic terms for time, as well as random intercepts for each patient and fixed effects for variables of interest. From the mixed effects models, the slopes and the 95% confidence intervals (CIs) of the baseline and early posttransplant factors were estimated. Models for day 60 CMV reactivation and day 100 aGVHD considered only immune recovery data beyond 60 and 100 days, respectively.
Landmark analyses at 2, 4, and 6 months were performed to investigate the association between each of the immune variables and OS. For the 2-, 4-, and 6-month landmark analyses, the most recent immune parameter values prior to day 65, 130, and 195 were used, respectively. Univariable OS analyses were first performed for each immune variable, baseline factors, and early posttransplant factors. Exploratory analyses were also performed to potentially identify an optimal CD4+ T-cell count based on its univariable association with OS at each of the landmark time points. Multivariable Cox regression models were built for each immune variable that was statistically significant controlling for significant baseline and/or posttransplant covariates. Immune variables were highly correlated with each other and therefore could not be included in the same models (correlations were assessed using Spearman’s rank correlation coefficient).
Tests with P < .01 were considered statistically significant, to account for multiple comparisons. All statistical analyses were performed in R version 3.5.3 (The R Foundation for Statistical Computing).
Results
Patient and graft characteristics
The characteristics of the 106 analyzed patients (median 50 years, range 22 to 70) and their grafts are summarized in Table 1. The most common diagnosis was acute leukemia (66%), followed by lymphoma (21%), or myelodysplasia/myeloproliferative disease (13%). The majority of patients (95%) received intermediate-intensity myeloablative conditioning.33
Nearly all patients (n = 104) received double-unit CB grafts. The median infused TNC and infused viable CD34+ cell doses of the engrafting unit were 2.35 (range 1.23-5.31) × 107/kg and 1.18 (range 0.18-4.08) × 105/kg, respectively. The median 8-allele engrafting unit-recipient HLA match was 5/8 (range 3/8-7/8).
Transplant outcomes
In all of the 106 patients (including all 61 recipients of CB grafts supplemented with haploidentical CD34+ cells), long-term hematopoiesis was mediated by 1 CB unit (termed the engrafting unit), with no contribution from the host. Of the 59 CMV-seropositive patients, 44 reactivated CMV by day 60 for a cumulative incidence of 75% (95% CI, 61-84). The cumulative incidence of grade II to IV and III to IV aGVHD by day 100 was 77% (95% CI, 68-84) and 17% (95% CI, 11-25), respectively. Of the 64 patients with grade II day 100 aGVHD, 22 (34%) were treated with systemic corticosteroids by day 100; remaining patients were treated with nonabsorbable oral or topical corticosteroids.
With a median survivor follow-up of 2 years (range 7 months to 4.7 years), the 2-year estimates of OS and progression-free survival for the 106 patients evaluable for immune recovery (8 nonevaluable patients with graft failure or early death excluded) were 73% (95% CI, 62-81) and 69% (95% CI, 58-78), respectively. Two-year TRM was 19% (95% CI, 12-28) and 2-year relapse was 12% (95% CI, 6-20).
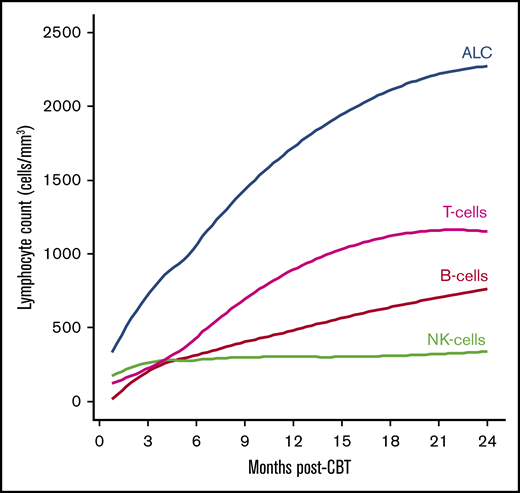
T-, NK-, and B-cell immune reconstitution
The median ALC surpassed 500/mm3 by 2 months. The speed of recovery varied markedly between lymphocyte subsets. NK cells were the most common lymphocyte population early posttransplant, followed by CD3+ T cells, and B cells. However, CD3+ T cells comprised the largest lymphocyte subset beyond 4 months (Table 2; Figure 1).
Recovery of lymphocyte subsets and PHA responses after CBT
| Immune variable, median (range) . | Posttransplant time point . | |||
|---|---|---|---|---|
| 2 mo . | 4 mo . | 6 mo . | 1 y . | |
| ALC, cells/mm3 (NR: 500-5300) | 608 (85-7200) | 745 (145-2025) | 933 (173-6287) | 1554 (384-4774) |
| CD3+ T cells, cells/mm3 (NR: 822-1825) | 171 (7-3024) | 252 (8-1112) | 380 (38-1572) | 669 (148-3246) |
| CD4+ T cells, cells/mm3 (NR: 429-1131) | 120 (5-1584) | 203 (8-912) | 294 (30-1069) | 420 (22-891) |
| CD8+ T cells, cells/mm3 (NR: 209-768) | 22 (0-1440) | 25 (0-761) | 47 (0-909) | 204 (11-2574) |
| B cells, cells/mm3 (NR: 87-441) | 22 (0-3024) | 150 (0-1357) | 201 (0-3960) | 324 (0-1968) |
| NK cells, cells/mm3 (NR: 78-424) | 222 (41-1333) | 252 (29-717) | 221 (65-1519) | 220 (70-896) |
| PHA, CPM (NR: 109 576-256 486) | 66 816 (231-156 128) | 76 319 (667-162 912) | 86 944 (14 590-161 140) | 86 091 (6724-164 435) |
| Immune variable, median (range) . | Posttransplant time point . | |||
|---|---|---|---|---|
| 2 mo . | 4 mo . | 6 mo . | 1 y . | |
| ALC, cells/mm3 (NR: 500-5300) | 608 (85-7200) | 745 (145-2025) | 933 (173-6287) | 1554 (384-4774) |
| CD3+ T cells, cells/mm3 (NR: 822-1825) | 171 (7-3024) | 252 (8-1112) | 380 (38-1572) | 669 (148-3246) |
| CD4+ T cells, cells/mm3 (NR: 429-1131) | 120 (5-1584) | 203 (8-912) | 294 (30-1069) | 420 (22-891) |
| CD8+ T cells, cells/mm3 (NR: 209-768) | 22 (0-1440) | 25 (0-761) | 47 (0-909) | 204 (11-2574) |
| B cells, cells/mm3 (NR: 87-441) | 22 (0-3024) | 150 (0-1357) | 201 (0-3960) | 324 (0-1968) |
| NK cells, cells/mm3 (NR: 78-424) | 222 (41-1333) | 252 (29-717) | 221 (65-1519) | 220 (70-896) |
| PHA, CPM (NR: 109 576-256 486) | 66 816 (231-156 128) | 76 319 (667-162 912) | 86 944 (14 590-161 140) | 86 091 (6724-164 435) |
CPM, counts per minute; NR, normal range.
ALC and lymphocyte subset recovery in adult CBT recipients. ALC, CD3+ cells, NK cells, B cells. Curves are Loess-smoothed averages.
ALC and lymphocyte subset recovery in adult CBT recipients. ALC, CD3+ cells, NK cells, B cells. Curves are Loess-smoothed averages.
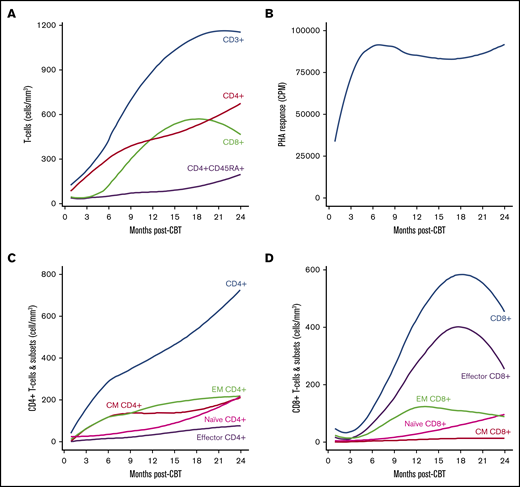
Of CD3+ T-cell subsets, CD4+ lymphocytes recovered faster than CD8+ lymphocytes (Table 2; Figure 2A). The median CD4+ T-cell count surpassed 200/mm3 by 4 months. CD4+CD45RA+ T cells, considered to represent naive CD4+ T cells, remained low in the first 6 to 9 months post-CBT (Figure 2A). CD8+ T cells increased steadily until 15 to 18 months post-CBT, followed by a relative contraction of the CD8+ T-cell compartment (Figure 2A). T-cell function, as assessed by PHA responses, increased rapidly and remained relatively stable beyond 6 months (Figure 2B).
Recovery of T-cell subsets and T-cell function in adult CBT recipients. (A) CD3+, CD4+, CD8+, CD4+CD45RA+ T cells. (B) PHA responses. (C) CD4+ and CD4+ T-cell subsets (naive, CM, EM, effector). (D) CD8+ and CD8+ T-cell subsets (naive, CM, EM, effector). Curves are Loess-smoothed averages. In panels C and D, Loess-smoothed curves for total CD4+ and total CD8+ T cells, respectively, are based on values from the time points of which the extended immunophenotyping panel was also performed.
Recovery of T-cell subsets and T-cell function in adult CBT recipients. (A) CD3+, CD4+, CD8+, CD4+CD45RA+ T cells. (B) PHA responses. (C) CD4+ and CD4+ T-cell subsets (naive, CM, EM, effector). (D) CD8+ and CD8+ T-cell subsets (naive, CM, EM, effector). Curves are Loess-smoothed averages. In panels C and D, Loess-smoothed curves for total CD4+ and total CD8+ T cells, respectively, are based on values from the time points of which the extended immunophenotyping panel was also performed.
Eighty-eight patients had 1 or more time points assayed with the extended lymphocyte subset immunophenotyping panel. EM and CM cells were the most prevalent CD4+ subsets post-CBT, followed by naive and effector subsets (Figure 2C). EM and CM CD4+ T-cell numbers increased rapidly in the first 6 months and remained relatively stable between 9 and 24 months. Naive CD4+ T cells increased steadily beyond 6 months. In contrast to CD4+ T-cell subsets, effector CD8+ T cells comprised the majority of CD8+ T cells post-CBT, followed by the EM CD8+ subset (Figure 2D). Following their marked initial increase, effector CD8+ T cells decreased beyond 18 months posttransplant. Recovery of naive CD8+ T cells paralleled that of naive CD4+ T cells beyond 6 months post-CBT (Figure 2D).
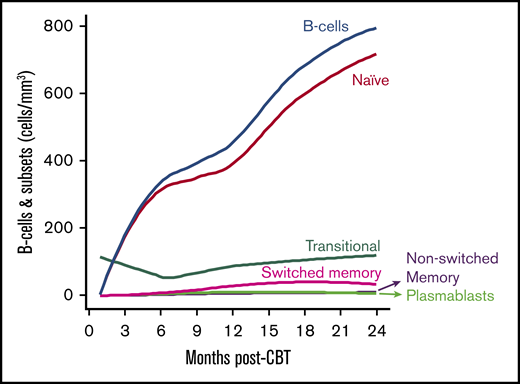
NK cells increased rapidly in the first 2 months post-CBT and remained stable thereafter (Table 2; Figure 1). B cells also rose rapidly with the median B-cell count reaching normal range by 4 months posttransplant (Table 2; Figure 1). This was explained by a marked increase of naive B cells in the first 6 months post-CBT. Naive B cells continued to be the most prevalent B-cell subset through 2 years post-CBT (Figure 3). Transitional B cells were the next most common B-cell subset, whereas nonswitched memory, switched memory, and plasmablast B-cell subsets remained low (Figure 3).
Recovery of B cells and subsets in adult CBT recipients. Curves are Loess-smoothed averages. Loess-smoothed curves for total B-cell counts are based on values from the time points of which the extended immunophenotyping panel was also performed.
Recovery of B cells and subsets in adult CBT recipients. Curves are Loess-smoothed averages. Loess-smoothed curves for total B-cell counts are based on values from the time points of which the extended immunophenotyping panel was also performed.
Association of patient, graft, and posttransplant variables with immune reconstitution
The association of baseline and early posttransplant variables with recovery of lymphocyte subsets and PHA responses is shown in Tables 3 and 4. No patient, graft (including the addition of haploidentical CD34+ cells), or early posttransplant variables were significantly associated with ALC or CD3+ T-cell recovery (Table 3).
Association of transplant variables with the recovery of ALC and total T, NK, and B cells
| . | ALC . | CD3+ T cells . | NK cells . | B cells . | ||||
|---|---|---|---|---|---|---|---|---|
| Variable . | Slope (95% CI) . | P . | Slope (95% CI) . | P . | Slope (95% CI) . | P . | Slope (95% CI) . | P . |
| Age (10 y) | 0.01 (−0.08, 0.09) | .897 | −0.06 (−0.16, 0.04) | .260 | 0.15 (0.07, 0.23) | .001 | −0.20 (−0.46, 0.07) | .146 |
| 8-allele HLA-match* | .135 | .733 | .327 | .465 | ||||
| <5/8 | reference | reference | reference | reference | ||||
| ≥5/8 | 0.17 (−0.05, 0.39) | 0.05 (−0.22, 0.31) | 0.12 (−0.12, 0.35) | 0.26 (−0.44, 0.96) | ||||
| Infused viable CD34+cell dose* | .099 | .840 | .018 | .245 | ||||
| <1.18 × 105/kg | reference | reference | reference | reference | ||||
| ≥1.18 × 105/kg | 0.17 (−0.03, 0.37) | 0.03 (−0.22, 0.27) | 0.25 (0.05, 0.46) | 0.38 (−0.25, 1.01) | ||||
| Infused viable CD3+cell dose* | .727 | .185 | .093 | .612 | ||||
| <3.34 × 106/kg | reference | reference | reference | reference | ||||
| ≥3.34 × 106/kg | 0.04 (−0.16, 0.24) | 0.16 (−0.08, 0.40) | −0.18 (−0.39, 0.03) | 0.164 (−0.47, 0.80) | ||||
| CMV reactivation by day 60 | .783 | .391 | .577 | .488 | ||||
| No CMV reactivation | reference | reference | reference | reference | ||||
| CMV reactivation | −0.03 (−0.23, 0.17) | 0.12 (−0.15, 0.38) | 0.06 (−0.15, 0.27) | −0.26 (−1.01, 0.48) | ||||
| Day 100 aGVHD grade | .313 | .960 | .708 | <.001 | ||||
| 0-I | reference | reference | reference | reference | ||||
| II | −0.16 (−0.43, 0.11) | −0.05 (−0.41, 0.31) | 0.09 (−0.19, 0.38) | −1.15 (−2.04, −0.26) | ||||
| III-IV | −0.26 (−0.60, 0.08) | −0.02 (−0.47, 0.43) | −0.01 (−0.37, 0.35) | −2.38 (−3.50, −1.25) | ||||
| . | ALC . | CD3+ T cells . | NK cells . | B cells . | ||||
|---|---|---|---|---|---|---|---|---|
| Variable . | Slope (95% CI) . | P . | Slope (95% CI) . | P . | Slope (95% CI) . | P . | Slope (95% CI) . | P . |
| Age (10 y) | 0.01 (−0.08, 0.09) | .897 | −0.06 (−0.16, 0.04) | .260 | 0.15 (0.07, 0.23) | .001 | −0.20 (−0.46, 0.07) | .146 |
| 8-allele HLA-match* | .135 | .733 | .327 | .465 | ||||
| <5/8 | reference | reference | reference | reference | ||||
| ≥5/8 | 0.17 (−0.05, 0.39) | 0.05 (−0.22, 0.31) | 0.12 (−0.12, 0.35) | 0.26 (−0.44, 0.96) | ||||
| Infused viable CD34+cell dose* | .099 | .840 | .018 | .245 | ||||
| <1.18 × 105/kg | reference | reference | reference | reference | ||||
| ≥1.18 × 105/kg | 0.17 (−0.03, 0.37) | 0.03 (−0.22, 0.27) | 0.25 (0.05, 0.46) | 0.38 (−0.25, 1.01) | ||||
| Infused viable CD3+cell dose* | .727 | .185 | .093 | .612 | ||||
| <3.34 × 106/kg | reference | reference | reference | reference | ||||
| ≥3.34 × 106/kg | 0.04 (−0.16, 0.24) | 0.16 (−0.08, 0.40) | −0.18 (−0.39, 0.03) | 0.164 (−0.47, 0.80) | ||||
| CMV reactivation by day 60 | .783 | .391 | .577 | .488 | ||||
| No CMV reactivation | reference | reference | reference | reference | ||||
| CMV reactivation | −0.03 (−0.23, 0.17) | 0.12 (−0.15, 0.38) | 0.06 (−0.15, 0.27) | −0.26 (−1.01, 0.48) | ||||
| Day 100 aGVHD grade | .313 | .960 | .708 | <.001 | ||||
| 0-I | reference | reference | reference | reference | ||||
| II | −0.16 (−0.43, 0.11) | −0.05 (−0.41, 0.31) | 0.09 (−0.19, 0.38) | −1.15 (−2.04, −0.26) | ||||
| III-IV | −0.26 (−0.60, 0.08) | −0.02 (−0.47, 0.43) | −0.01 (−0.37, 0.35) | −2.38 (−3.50, −1.25) | ||||
There was no association with the variables of recipient sex, diagnosis (acute leukemia vs MDS/MPD vs lymphoma), or the addition of haploidentical CD34+ cells (data not shown). P values significant at the .01 level are indicated in bold.
Engrafting CB unit.
Association of transplant variables with the recovery of T-cell subsets and function
| Variable . | CD4+ T cells . | CD4+CD45RA+ T cells . | CD8+ T cells . | PHA . | ||||
|---|---|---|---|---|---|---|---|---|
| Slope (95% CI) . | P . | Slope (95% CI) . | P . | Slope (95% CI) . | P . | Slope (95% CI) . | P . | |
| Age (10 y) | −0.09 (−0.20, 0.01) | .087 | −0.05 (−0.22, 0.12) | .539 | 0.01 (−0.15, 0.16) | .924 | −0.08 (−0.21, 0.04) | .205 |
| 8-allele HLA-match* | .200 | .545 | .105 | .565 | ||||
| <5/8 | reference | reference | reference | reference | ||||
| ≥5/8 | 0.19 (−0.10, 0.47) | 0.14 (−0.30, 0.58) | −0.33 (−0.73, 0.07) | 0.09 (−0.22, 0.41) | ||||
| Infused viable CD34+cell dose* | .646 | .333 | .245 | .574 | ||||
| <1.18 × 105/kg | reference | reference | reference | reference | ||||
| ≥1.18 × 105/kg | −0.06 (−0.32, 0.20) | −0.20 (−0.60, 0.20) | 0.22 (−0.15, 0.58) | 0.08 (−0.21, 0.37) | ||||
| Infused viable CD3+cell dose* | .045 | .020 | .893 | .065 | ||||
| <3.34 × 106/kg | reference | reference | reference | reference | ||||
| ≥3.34 × 106/kg | 0.26 (0.01, 0.52) | 0.47 (0.08, 0.87) | 0.03 (−0.34, 0.39) | 0.27 (−0.01, 0.56) | ||||
| CMV reactivation by day 60 | .005 | .171 | <.001 | <.001 | ||||
| No CMV reactivation | reference | Reference | reference | reference | ||||
| CMV reactivation | −0.39 (−0.66, −0.13) | −0.31 (−0.75, 0.13) | 1.15 (0.77, 1.52) | −0.58 (−0.86, −0.29) | ||||
| Day 100 aGVHD grade | .651 | .386 | .630 | .435 | ||||
| 0-I | reference | reference | reference | reference | ||||
| II | −0.16 (−0.52, 0.20) | −0.05 (−0.62, 0.51) | 0.29 (−0.32, 0.90) | −0.20 (−0.61, 0.21) | ||||
| III-IV | −0.19 (−0.65, 0.27) | 0.37 (0.36, 1.10) | 0.30 (−0.48, 1.07) | −0.33 (−0.83, 0.17) | ||||
| Variable . | CD4+ T cells . | CD4+CD45RA+ T cells . | CD8+ T cells . | PHA . | ||||
|---|---|---|---|---|---|---|---|---|
| Slope (95% CI) . | P . | Slope (95% CI) . | P . | Slope (95% CI) . | P . | Slope (95% CI) . | P . | |
| Age (10 y) | −0.09 (−0.20, 0.01) | .087 | −0.05 (−0.22, 0.12) | .539 | 0.01 (−0.15, 0.16) | .924 | −0.08 (−0.21, 0.04) | .205 |
| 8-allele HLA-match* | .200 | .545 | .105 | .565 | ||||
| <5/8 | reference | reference | reference | reference | ||||
| ≥5/8 | 0.19 (−0.10, 0.47) | 0.14 (−0.30, 0.58) | −0.33 (−0.73, 0.07) | 0.09 (−0.22, 0.41) | ||||
| Infused viable CD34+cell dose* | .646 | .333 | .245 | .574 | ||||
| <1.18 × 105/kg | reference | reference | reference | reference | ||||
| ≥1.18 × 105/kg | −0.06 (−0.32, 0.20) | −0.20 (−0.60, 0.20) | 0.22 (−0.15, 0.58) | 0.08 (−0.21, 0.37) | ||||
| Infused viable CD3+cell dose* | .045 | .020 | .893 | .065 | ||||
| <3.34 × 106/kg | reference | reference | reference | reference | ||||
| ≥3.34 × 106/kg | 0.26 (0.01, 0.52) | 0.47 (0.08, 0.87) | 0.03 (−0.34, 0.39) | 0.27 (−0.01, 0.56) | ||||
| CMV reactivation by day 60 | .005 | .171 | <.001 | <.001 | ||||
| No CMV reactivation | reference | Reference | reference | reference | ||||
| CMV reactivation | −0.39 (−0.66, −0.13) | −0.31 (−0.75, 0.13) | 1.15 (0.77, 1.52) | −0.58 (−0.86, −0.29) | ||||
| Day 100 aGVHD grade | .651 | .386 | .630 | .435 | ||||
| 0-I | reference | reference | reference | reference | ||||
| II | −0.16 (−0.52, 0.20) | −0.05 (−0.62, 0.51) | 0.29 (−0.32, 0.90) | −0.20 (−0.61, 0.21) | ||||
| III-IV | −0.19 (−0.65, 0.27) | 0.37 (0.36, 1.10) | 0.30 (−0.48, 1.07) | −0.33 (−0.83, 0.17) | ||||
Engrafting CB unit.
There was no association with the variables of recipient sex, diagnosis (acute leukemia vs MDS/MPD vs lymphoma), or the addition of haploidentical CD34+ cells (data not shown). P values significant at the .01 level are indicated in bold.
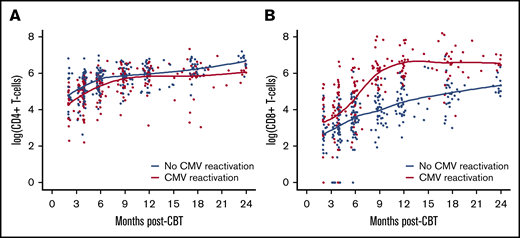
Patient characteristics, including age, sex, or diagnosis, were not significantly associated with CD4+ or CD8+ T-cell recovery. A higher engrafting unit infused viable CD3+ cell dose was associated with higher CD4+ and CD4+CD45RA+ T-cell counts after CBT, although these associations were not significant at the 0.01 level (Table 4). Conversely, CMV reactivation was associated with lower CD4+ T cells (Figure 4A) and PHA responses post-CBT (Table 4). In contrast, CMV reactivation was the only factor significantly associated with higher CD8+ T-cell counts posttransplant (Table 4; Figure 4B).
Association of CMV reactivation with CD4+and CD8+T-cell recovery in adult CBT recipients. (A) CD4+ T-cell recovery according to CMV reactivation by day 60 post-CBT. (B) CD8+ T-cell recovery according to CMV reactivation by day 60 post-CBT. Individual patient time points are color coded according to CMV reactivation. Curves are Loess-smoothed averages.
Association of CMV reactivation with CD4+and CD8+T-cell recovery in adult CBT recipients. (A) CD4+ T-cell recovery according to CMV reactivation by day 60 post-CBT. (B) CD8+ T-cell recovery according to CMV reactivation by day 60 post-CBT. Individual patient time points are color coded according to CMV reactivation. Curves are Loess-smoothed averages.
The association of transplant variables with the recovery of CD4+ T-cell subsets is shown in supplemental Table 1. A higher engrafting unit CD34+ cell dose was associated with higher EM CD4+ T-cell counts, whereas a higher engrafting unit CD3+ dose was associated with higher naive CD4+ T-cell counts post-CBT, although these associations did not reach significance at the 0.01 level. CMV reactivation was associated with lower CM and, to a lesser extent, naive CD4+ T-cell counts (supplemental Figure 1). No transplant factors were associated with effector CD4+ T-cell reconstitution. Increased numbers of activated CD4+ T cells were observed in association with a higher engrafting unit CD34+ cell dose, whereas lower activated CD4+ T-cell counts were seen in patients with aGVHD, especially corticosteroid-requiring aGVHD (data not shown). These associations, however, did not reach the prespecified level of statistical significance.
The association of transplant variables with the recovery of CD8+ T-cell subsets is shown in supplemental Table 2. A higher engrafting unit CD34+ cell dose was associated with higher EM and, to a lesser extent, effector CD8+ T-cell counts after CBT. In addition, a marked expansion of EM and effector CD8+ T cells was observed in patients with CMV reactivation (supplemental Figure 2). No transplant factors were significantly associated with CM or naive CD8+ T-cell reconstitution. A higher number of activated CD8+ T cells were observed in association with higher CD34+ dose of the engrafting CB unit and CMV reactivation.
Older recipient age and higher CD34+ cell dose of the engrafting CB unit were associated with NK-cell recovery early posttransplant (Table 3). B-cell reconstitution was adversely affected by the development of grade II to IV aGVHD (Table 3), especially aGVHD requiring systemic corticosteroids (data not shown). The negative effect of aGVHD was also observed in naive, transitional, nonswitched memory, and to a lesser extent, switched memory and plasmablast B-cell subset recovery (data not shown). No other transplant factors were associated with B-cell recovery.
Association of immune variables with OS
Next, we investigated the association of immune reconstitution with OS in serial landmark analyses. At 2 months, recipient age was the only baseline factor associated with OS (Table 5). A higher PHA response was the only immune variable associated with improved OS in univariable and multivariable analysis controlling for age. This was due to decreased TRM in patients with higher PHA responses, whereas relapse risk was unaffected (data not shown).
Two-month landmark analysis for OS
| Immune variable* . | n . | HR (95% CI) . | P . |
|---|---|---|---|
| ALC | 90 | 0.67 (0.34-1.31) | .246 |
| CD3+ T cells | 90 | 0.73 (0.45-1.18) | .219 |
| CD4+ T cells | 90 | 0.69 (0.43-1.12) | .150 |
| CD4+CD45RA+ T cells | 90 | 1.11 (0.75-1.64) | .587 |
| CD8+ T cells | 90 | 1.00 (0.66-1.49) | .984 |
| NK cells | 78 | 1.34 (0.63-2.84) | .439 |
| B cells | 90 | 0.85 (0.68-1.07) | .163 |
| PHA | 88 | 0.56 (0.40-0.78)† | .009 |
| Immune variable* . | n . | HR (95% CI) . | P . |
|---|---|---|---|
| ALC | 90 | 0.67 (0.34-1.31) | .246 |
| CD3+ T cells | 90 | 0.73 (0.45-1.18) | .219 |
| CD4+ T cells | 90 | 0.69 (0.43-1.12) | .150 |
| CD4+CD45RA+ T cells | 90 | 1.11 (0.75-1.64) | .587 |
| CD8+ T cells | 90 | 1.00 (0.66-1.49) | .984 |
| NK cells | 78 | 1.34 (0.63-2.84) | .439 |
| B cells | 90 | 0.85 (0.68-1.07) | .163 |
| PHA | 88 | 0.56 (0.40-0.78)† | .009 |
P values significant at the .01 level are indicated in bold.
In univariable analysis of patient and graft variables, only recipient age was significantly associated with OS (hazard ratio [HR], 2.11 [95% CI, 1.30-3.43] per decade, P = .001). Patient sex, diagnosis, CMV seropositivity, engrafting CB unit–recipient HLA-match, engrafting CB unit infused viable CD34+ and CD3+ cell doses, addition of haploidentical CD34+ cells were not significant.
HR adjusted for age.
In the 4-month landmark analysis (Table 6), recipient age was again the only baseline factor impacting OS. In addition, there was no association of day 100 aGVHD grade with OS. In univariable analysis, 4-month ALC, total CD3+ and CD4+ T cells, and PHA responses were significantly associated with OS beyond 4 months. Although an association of higher B-cell counts with improved OS was also observed, it was not significant at the 0.01 level. In multivariable analyses controlling for age, each of the variables of ALC, CD3+ and CD4+ T cells, and PHA remained significant. As expected, CD4+ T-cell counts and PHA responses at 4 months were highly correlated (r = 0.35). Therefore, they could not be concurrently included in a multivariable model.
Four-month landmark analysis for OS
| Immune variable* . | n . | HR (95% CI) . | P . |
|---|---|---|---|
| ALC | 93 | 0.20 (0.08-0.51)† | .004 |
| CD3+ T cells | 93 | 0.41 (0.24-0.71)† | .006 |
| CD4+ T cells | 93 | 0.43 (0.25-0.73)† | .006 |
| CD4+CD45RA+ T cells | 93 | 1.03 (0.70-1.51) | .887 |
| CD8+ T cells | 93 | 0.86 (0.60-1.24) | .434 |
| NK cells | 91 | 0.71 (0.32-1.60) | .420 |
| B cells | 93 | 0.80 (0.66-0.97) | .029 |
| PHA | 89 | 0.43 (0.26-0.71)† | .008 |
| Immune variable* . | n . | HR (95% CI) . | P . |
|---|---|---|---|
| ALC | 93 | 0.20 (0.08-0.51)† | .004 |
| CD3+ T cells | 93 | 0.41 (0.24-0.71)† | .006 |
| CD4+ T cells | 93 | 0.43 (0.25-0.73)† | .006 |
| CD4+CD45RA+ T cells | 93 | 1.03 (0.70-1.51) | .887 |
| CD8+ T cells | 93 | 0.86 (0.60-1.24) | .434 |
| NK cells | 91 | 0.71 (0.32-1.60) | .420 |
| B cells | 93 | 0.80 (0.66-0.97) | .029 |
| PHA | 89 | 0.43 (0.26-0.71)† | .008 |
P values significant at the .01 level are indicated in bold.
In univariable analysis of patient, graft, and posttransplant variables, only recipient age was significantly associated with OS (HR, 2.21 [95% CI, 1.31-3.75] per decade, P = .001). Patient sex, diagnosis, CMV seropositivity, engrafting CB unit–recipient HLA match, engrafted CB unit infused viable CD34+ and CD3+ cell doses, addition of haploidentical CD34+ cells, and day 100 aGVHD grade were not significant.
HR adjusted for age.
At 6 months (Table 7), the association of recipient age with OS was no longer significant at the 0.01 level (P = .025), but was retained in multivariable modeling because it is a clinically important factor. Of the immune variables, higher ALC, total CD3+ and CD4+ T cells, and PHA responses were significantly associated with subsequent improved OS in univariable and age-adjusted analyses. As with the 4-month landmark, CD4+ T-cell counts and PHA responses at 6 months were highly correlated (r = 0.39); therefore, their independent prognostic significance could not be examined.
Six-month landmark analysis for OS
| Immune variable* . | n . | HR (95% CI) . | P . |
|---|---|---|---|
| ALC | 92 | 0.20 (0.07-0.54)† | .003 |
| CD3+ T cells | 93 | 0.34 (0.19-0.61)† | .001 |
| CD4+ T cells | 93 | 0.30 (0.16-0.56)† | <.001 |
| CD4+CD45RA+ T cells | 93 | 0.90 (0.59-1.39) | .651 |
| CD8+ T cells | 93 | 0.74 (0.45-1.21) | .221 |
| NK cells | 93 | 0.85 (0.31-2.34) | .757 |
| B cells | 93 | 0.80 (0.64-0.99) | .054 |
| PHA | 89 | 0.34 (0.17-0.68)† | .004 |
| Immune variable* . | n . | HR (95% CI) . | P . |
|---|---|---|---|
| ALC | 92 | 0.20 (0.07-0.54)† | .003 |
| CD3+ T cells | 93 | 0.34 (0.19-0.61)† | .001 |
| CD4+ T cells | 93 | 0.30 (0.16-0.56)† | <.001 |
| CD4+CD45RA+ T cells | 93 | 0.90 (0.59-1.39) | .651 |
| CD8+ T cells | 93 | 0.74 (0.45-1.21) | .221 |
| NK cells | 93 | 0.85 (0.31-2.34) | .757 |
| B cells | 93 | 0.80 (0.64-0.99) | .054 |
| PHA | 89 | 0.34 (0.17-0.68)† | .004 |
P values significant at the .01 level are indicated in bold.
In univariable analysis of patient, graft, and posttransplant variables, only recipient age was associated with OS, although not at the 0.01 significance level (HR, 1.78 [95% CI, 1.04-3.03] per decade, P = .025). Patient sex, diagnosis, CMV seropositivity, engrafting CB unit–recipient HLA-match, engrafting CB unit infused viable CD34+ and CD3+ cell doses, addition of haploidentical CD34+ cells, and day 100 aGVHD grade were not significant.
HR adjusted for age.
CD4+CD45RA+ T-cell, CD8+ T-cell, or NK-cell counts were not associated with OS at any time point post-CBT (Tables 5-7). In addition, due to the limited number of events in assayed patients, the prognostic value of specific CD4+ and CD8+ T-cell subsets could not be evaluated. Finally, in exploratory analyses, no optimal CD4+ T-cell count cutoff for OS could be identified at any time point post-CBT.
Discussion
This study represents the largest analysis of immune reconstitution after ATG-free CBT in adults to date. In contrast to the protracted T-cell lymphopenia reported after ATG-based CBT, we show rapid early thymus-independent CD4+ T-cell recovery consistent with that reported in pediatric ATG-free CBT.23,24 In this adult population with a median age of 50 years, the median CD4+ T-cell count already exceeded 200/mm3 by 4 months and increased steadily through 2 years posttransplant. EM and CM T cells were the most prevalent CD4+ subsets early post-CBT,11,34 whereas naive CD4+ T-cell counts gradually increased beyond 6 to 9 months post-CBT.
Recovery of CD8+ T cells was initially slow, but marked CD8+ T-cell expansion was noted beyond 6 months post-CBT.28 Effector and EM were the most common CD8+ T-cell subsets early post-CBT.11,34 As with naive CD4+ T cells, naive CD8+ T-cell counts increased steadily beyond 6 to 9 months, suggesting thymus-dependent recovery from this time point, even despite the relatively advanced age of this patient cohort.15 Recovery of T-cell function, as assayed by PHA responses, was also prompt.
Of factors associated with T-cell reconstitution, a notable finding was the lack of an adverse effect of recipient age on total, CD4+, CD8+, and subset T-cell recovery. It is possible that the relatively older age of this patient cohort did not allow the detection of such an effect. Alternatively, early thymus-independent T-cell recovery after ATG-free CBT may not be significantly influenced by advanced recipient age, in contrast to the thymus-dependent pathway of T-cell reconstitution.15 Data concerning the potential impact of CB graft characteristics on T-cell recovery after CBT are limited.23,35,36 We observed a notable trend for a higher engrafting CB unit infused viable CD3+ cell dose being associated with higher total and naive CD4+ T cells post-CBT. In addition, higher engrafting CB unit infused viable CD34+ cell dose was associated with higher EM and activated CD8+ T-cell counts, and a similar trend was observed for the same CD4+ T-cell subsets. Interestingly, despite high levels of engrafting CB unit-recipient HLA-mismatch, such mismatch had no discernible effect on total T-cell and subset recovery. In addition, despite concerns that aGVHD may hamper immune reconstitution,36-38 overall grade II to IV aGVHD did not significantly affect T-cell recovery in our series, with the exception of activated CD4+ T-cell counts.
CMV reactivation significantly impacts quantitative and qualitative T-cell recovery after HSC transplantation (HSCT).39,40 CMV reactivation after HSCT has been associated with a rapid increase of CD8+ T cells due to EM and effector CD8+ subset expansion.39-45 The impact on total CD4+ T-cell and subset recovery, however, is less clear,39-43 with a previous report suggesting that CMV reactivation may compromise thymopoiesis.39 These effects lead to contraction of the naive T-cell compartment and TCR repertoire diversity.39,43,46 In our analysis, a marked expansion of total CD8+, EM and effector CD8+ T-cell subsets, and activated CD8+ T cells44 was observed in patients with CMV reactivation post-CBT. Because CB T cells are exclusively naive,47 this CMV-driven CD8+ T-cell expansion reflects the emergence of CMV effectors from naive CB-derived T cells. Although T-cell specificity was not examined, our findings are supported by reports that CMV effectors with memory phenotype are generated from naive CB-derived T cells early post-CBT48-50 and after CMV infection in neonates.51 We also observed that CMV reactivation was associated with lower total and CM CD4+ T-cell counts. Although naive CD4+ T cells were also numerically lower, this difference was not significant at the prespecified significance threshold. Therefore, although we demonstrate a negative impact of CMV reactivation on CD4+ T-cell recovery after CBT, whether thymopoiesis is impaired is uncertain.39
A critical finding of this analysis is that early T-cell recovery, especially CD4+ counts and T-cell function, was associated with improved survival. Although an association of CD4+ counts with OS was not observed at 2 months, >75% of assayed patients already had CD4+ T cells >50/mm3 by that time, a threshold previously associated with protection against infections and improved survival in pediatric CBT.19,22,52,53 Importantly, we observed a continuous reduction in overall mortality with increasing CD4+ T-cell counts at 4 and 6 months post-CBT. Because CD4+ T cells were the most prevalent CD3+ subset at these time points, this lymphocyte population likely also accounted for the prognostic significance of CD3+ T-cell counts and ALC on survival. In contrast, CD8+ T-cell counts were not associated with survival, as previously reported after adult donor HSCT.38,54 Early recovery of T-cell function as assessed by PHA responses was also associated with improved survival, as has previously been reported in CD34+ selected HSCT recipients,55 and was highly correlated with CD4+ T-cell counts.
Notably, in contrast to previous reports supporting an important role of thymopoiesis on CBT outcomes,15,30,48 we did not observe an association of CD4+CD45RA+ T-cell count recovery with improved survival. A possible explanation is that ATG omission may decrease reliance on thymopoiesis for CD4+ T-cell reconstitution due to early thymus-independent T-cell recovery.
Previous CBT studies have reported prompt posttransplant NK- and B-cell recovery, regardless of ATG use.12,28,29,56 Similarly, we observed early NK-cell recovery in our cohort. Unexpectedly, advanced recipient age was associated with higher NK-cell counts, as has previously been suggested in some HSCT studies,36,55 and may represent a compensatory mechanism as recovery of adaptive immunity may be delayed in older HSCT recipients. We also observed an association of a higher engrafting unit infused viable CD34+ cell dose with higher NK-cell counts post-CBT. In contrast, NK-cell counts tended to be lower in recipients of a higher engrafting unit infused viable CD3+ cell dose, a finding possibly explained by NK- and T-cell competition for homeostatic cytokines.57 Similar findings have been reported in adult donor HSCT.58,59 Importantly, in contrast to multiple HSCT series,54,58,60-62 we found no association between NK-cell counts and CBT outcomes.
B-cell counts normalized by 4 months and were primarily characterized by naive immunophenotype. Development of grade II to IV aGVHD by day 100, and especially corticosteroid-requiring GVHD, was the only factor that adversely affected B-cell and subset recovery. Whether B-cell recovery has any prognostic value for CBT outcomes remains unclear, as the prespecified statistical significance threshold in our analysis was not achieved.
A striking finding of our study is that T-cell recovery after ATG-free CBT in adults is robust, thymus independent, and CD4+ biased. These results add to the growing literature supporting an underappreciated prompt T-cell recovery after T-replete CBT.19,22-24,28 They suggest that the reconstituting neonatal immune system in adult CBT recipients has unique biology as previously demonstrated in children.24 The observed CD4+ bias is in contrast to the inversion of the CD4+/CD8+ T-cell ratio after adult donor HSCT. Moreover, our study demonstrates that early CD4+ T-cell recovery after adult CBT, as well as T-cell function, is associated with reduction in overall mortality, corroborating previous HSCT and primarily pediatric CBT studies.22,28,38,53-55,63,64
We acknowledge that not all patients had early T-cell recovery. Therefore, as with adult donor HSCT, strategies to further augment immune reconstitution are needed. Notably, we found that increased cell dose improved T-cell recovery, whereas HLA mismatch was not detrimental. If these findings are confirmed, they would support prioritizing cell dose over HLA match in CB unit selection as a potentially modifiable factor to promote both myeloid engraftment and T-cell recovery. In addition, although grade II to IV aGVHD did not significantly affect overall T-cell recovery or mortality, severe aGVHD is often associated with significant morbidity and opportunistic infections. Moreover, mitigation of aGVHD burden may further speed thymus-dependent T-cell recovery due to the deleterious effect of aGVHD on thymopoiesis.37,65 Therefore, based on the promising results reported in adult donor HSCT,66,67 our center is now investigating enhanced aGVHD prophylaxis with the addition of tocilizumab (#NCT03434730) as a nonlymphodepleting strategy. Finally, although CMV-specific immunity ultimately develops, most seropositive CBT recipients reactivate CMV early posttransplant.68 Therefore, our center has adopted letermovir prophylaxis starting day +7 for all adult CMV-seropositive CBT recipients.69 It is possible that reduction in CMV reactivation could in turn improve CD4+ T-cell recovery in these patients.
Our study could have benefited from an even larger patient sample size and more frequent lymphocyte subset immunophenotyping assessments. In addition, detailed evaluation of thymopoiesis, including T-cell receptor excision circles15 and T-cell repertoire diversity,43,46 virus-specific T-cell responses,29,39,48-50 and analysis of phenotypic or functional NK-cell reconstitution,62,70,71 were not routinely performed. These should be investigated in the future to further elucidate the biology of immune recovery after CBT. Future correlation of quantitative and qualitative T-cell reconstitution with functional immune competence, as evidenced by protection against viral infections,52,72 will also be critically important. Such studies could identify immune milestones that may inform the duration of needed viral monitoring and the safe cessation of antiviral prophylaxis, including letermovir. Correlation of B-cell recovery with vaccine responses73 will also be of great interest. Finally, CBT has been associated with robust GVL effects,4,5,74 and early CD4+ T-cell recovery has been associated with reduction in relapse risk in patients with myeloid malignancies.22,53 Thus, further research should focus on the impact of T-cell recovery on TRM and relapse risk separately, as well as the unique immune biology of CB-mediated GVL.
Acknowledgments
The authors thank Theodore and Laura Hromadka for their generous support.
This research was supported in part by the National Institutes of Health, National Cancer Institute grants P01 CA23766 and P30 CA008748.
Authorship
Contribution: I.P., M.-A.P., and J.N.B. designed the study and assembled and analyzed the data; I.P. and J.N.B. wrote the manuscript; J.A.L. and P.H. performed the statistical analysis; T.B. and M.A.M. maintained the patient database and procured data for the study; I.P., J.A.L., P.H., C.C., S.A.G., M.R.M.v.d.B., M.-A.P., and J.N.B. interpreted the data and reviewed and edited the manuscript; and all authors have approved the final version of the manuscript.
Conflict-of-interest disclosure: I.P. serves on a data and safety monitoring board for ExcellThera. S.A.G. has served as a consultant for Amgen, Actinium, Celgene, Johnson & Johnson, Jazz Pharmaceutical, Takeda, Novartis, Kite, and Spectrum Pharma and has received research funding from Amgen, Actinium, Celgene, Johnson & Johnson, Miltenyi, and Takeda. M.R.M.v.d.B. has received research support from Seres Therapeutics; has consulted, received honorarium from or participated in advisory boards for Seres Therapeutics, Flagship Ventures, Novartis, Evelo, Jazz Pharmaceuticals, Therakos, Amgen, Magenta Therapeutics, Merck & Co, Inc, Acute Leukemia Forum, and DKMS Medical Council (Board); has IP Licensing with Seres Therapeutics, Juno Therapeutics, and has stock options from Smart Immune. M.-A.P. has received honoraria from AbbVie, Bellicum, Bristol-Myers Squibb, Incyte, Merck, Novartis, Nektar Therapeutics, and Takeda; serves on data and safety monitoring boards for Servier and Medigene and the scientific advisory boards of MolMed and NexImmune; and has received research support for clinical trials from Incyte, Kite (Gilead), and Miltenyi Biotec. J.N.B. has received clinical trial funding from Angiocrine Bioscience and unrestricted educational grants from Gamida Cell and Merck. The remaining authors declare no competing financial interests.
The current affiliation for P.H. is RWJ Barnabas Health, St. Barnabas Medical Center, Livingston, NJ.
Correspondence: Ioannis Politikos, Adult Bone Marrow Transplantation Service, Department of Medicine, Memorial Sloan Kettering Cancer Center, 1275 York Ave, Box 259, New York, NY 10065; e-mail: politiki@mskcc.org.
References
Author notes
The full-text version of this article contains a data supplement.
M.-A.P. and J.N.B. contributed equally to this study.
To request original data, contact corresponding author, Ioannis Politikos (politiki@mskcc.org).