Abstract
Growing evidence suggests that human microbiota likely influence diverse processes including hematopoiesis, chemotherapy metabolism, and efficacy, as well as overall survival in patients with hematologic malignancies and other cancers. Both host genetic susceptibility and host-microbiota interactions may impact cancer risk and response to treatment; however, microbiota have the potential to be uniquely modifiable and accessible targets for treatment. Here, we focus on strategies to modify microbiota composition and function in patients with cancer. First, we evaluate the use of fecal microbiota transplant to restore microbial equilibrium following perturbation by antibiotics and chemotherapy, and as a treatment of complications of hematopoietic stem cell transplantation (HSCT), such as graft-versus-host disease and colonization with multidrug-resistant organisms. We then address the potential use of both probiotics and dietary prebiotic compounds in targeted modulation of the microbiota intended to improve outcomes in hematologic diseases. With each type of therapy, we highlight the role that abnormal, or dysbiotic, microbiota play in disease, treatment efficacy, and toxicity and evaluate their potential promise as emerging strategies for microbiota manipulation in patients with hematologic malignancies and in those undergoing HSCT.
Clinical case
A 45-year-old woman with BCR-ABL+ acute lymphoblastic leukemia and persistent minimal residual disease underwent peripheral blood allogeneic hematopoietic stem cell transplantation (HSCT) from a mismatched unrelated donor. Forty-two days after transplant, she developed >1.5 L per day of watery diarrhea and abdominal cramping. Infectious studies including Clostridium difficile polymerase chain reaction (PCR) were negative. She underwent colonoscopy, and pathology was consistent with grade IV graft-versus-host disease (GVHD). She was started on methylprednisolone (2 mg/kg per day) and total parenteral nutrition. Her diarrhea continued, and on the fifth day of high-dose steroids, she developed hematochezia. She was started on ruxolitinib with mild improvement of her stool output. After 10 days without further improvement, she underwent a fecal microbiota transplant (FMT) by colonoscopy from a donor screened for bacterial and viral pathogens. The patient’s diarrhea improved within 3 days to <500 mL per day and she was eventually tapered off of steroids.
Introduction
Thousands of species of bacteria, fungi, archaea, and viruses, collectively called the microbiota, colonize humans and interact with the immune system to influence health. Among the many microbial niches that exist in and on the human body, the intestinal microbiota are the most well studied and contain the greatest number of organisms. The microbiota-host dyad appears to have coevolved over the course of human history, likely contributing to the role of human microbes in immune development, homeostasis, and maintenance of normal intestinal epithelial barrier function.
Growing evidence suggests that human microbes likely influence diverse processes including hematopoiesis,1 immune system function,2 chemotherapy and radiation efficacy,3 and toxicity,4 GVHD risk,5 and overall survival in patients with hematologic malignancies and other cancers.6 Strategies to alter microbiota composition and function are being increasingly explored in the treatment of cancer; here, we focus on current therapies that modify the intestinal microbiota in patients with hematologic malignancies. We begin with the use of live microbial therapies including FMT and probiotics and then discuss the potential for dietary fibers known as prebiotics to modify the microbiota. With each therapy, we highlight the role that abnormal, or dysbiotic, microbiota plays in disease, treatment efficacy, and toxicity, and discuss emerging strategies for microbiota manipulation in patients with hematologic malignancies.
Live microbial therapies
Why fecal microbiota transplant? Beyond treatment of recurrent C difficile infection in hematologic malignancy
The transfer of fecal material from a donor to a recipient with the intent of altering the microbiota of the recipient, known as FMT, is a promising treatment of diseases beyond C difficile infection (CDI). Although knowledge regarding the precise mechanisms for FMT’s success in treating CDI remains incomplete, it is thought that the administration of fecal material to reconstitute intestinal microbiota diversity is not only effective due to competition with pathogens for occupation of ecological niches, but also due to microbial modulation of the recipient’s innate and adaptive immune response (as reviewed previously by Khoruts and Sadowsky7 ). For example, commensal microorganisms indirectly compete with pathogens for nutrients and can produce antimicrobial peptides with activity against pathogens.7 Additionally, commensals induce host production of cytokines such as interleukin 22 (IL-22), which serve to maintain intestinal epithelial barrier function and reduce bacterial translocation of pathogens.7 With these mechanisms in mind, novel uses of FMT are being tested and expanded to: (i) abrogate chemotherapy and radiation toxicity, (ii) prevent and treat steroid-refractory GVHD and other complications of HSCT, and (iii) eliminate multidrug-resistant organisms (MDROs).
FMT may alter cancer treatment toxicity and efficacy
Maintenance of an intact gut mucosa barrier and immunologic homeostasis requires continuous interaction between intestinal epithelial cells, mucosal and systemic immune systems, and diverse and healthy gut microbiota. Disruption of the gut microbiota following chemotherapy, radiation, and antibiotics is thought to both shape responses to treatment and impact their toxicity. For example, vancomycin administration diminished the T-helper 17 (Th17)-mediated antitumor response required for cyclophosphamide efficacy in a murine model.3 Additionally, radiation toxicity was exacerbated by enhanced IL-1β and tumor necrosis factor α expression mediated by intestinal microbial dysbiosis.4 FMT has been proposed for the prevention and treatment of therapy-related toxicities in patients receiving chemotherapy, radiation, and immunotherapy. To date, the only published studies to investigate the use of FMT in mitigating the toxicity of chemotherapy or radiation have been performed in murine models.8,9 In these studies, FMT from untreated mice was able to recapitulate the microbial composition of the pretreatment gut microbiota following radiation,8 chemotherapy, and antibiotics9 as well as ameliorate radiation-induced toxicity as measured by intestinal gene-expression profiles.9 A clinical trial using FMT to treat radiation toxicity in patients with hematologic malignancies is ongoing (NCT03516461) (Table 1).
Clinical trials of microbiota therapies in cancer patients
| NCT identifier . | Study type . | Sample size . | Study population . | Study name . | Patient cohorts . | Delivery route . | Primary outcome . | Secondary outcomes . | Current status . |
|---|---|---|---|---|---|---|---|---|---|
| FMT in checkpoint inhibitor therapy | |||||||||
| NCT04038619 | Phase 1 single-arm | 40 | GU malignancy +ICI colitis, age >18 y | FMT for ICI Induced Diarrhea/Colitis in Genitourinary Cancer Patients | Loperamide +FMT | Colonoscopy | 1. FMT safety and tolerability 2. Colitis response | ICI colitis recurrence | Not yet recruiting |
| NCT03772899 | Phase 1 single-arm | 20 | Melanoma + anti-PD-1 immunotherapy, age >18 y | FMT in Combination with Immunotherapy in Melanoma Patients (MIMic) | ICI + FMT | Capsules | Safety, AE | 1. Immunotherapy response rate, 2. gut microbiome changes, 3. immune blood markers, 4. urine metabolomics | Recruiting |
| NCT03353402 | Phase 1 single-arm | 40 | Melanoma stage IV or unresectable stage III, age >18 y | FMT in Metastatic Melanoma Patients Who Failed Immunotherapy | FMT using ICI responder stool | Colonoscopy and capsules | 1. FMT-related AE, 2. FMT engraftment | Changes in: 1. immune cell composition, 2. immune cell activity | Recruiting |
| NCT03341143 | Phase 2 single-arm | 20 | Advanced melanoma + anti-PD-1 nonresponders, age >18 y | Phase 2 Feasibility Study of FMT in Advanced Melanoma Patients Not Responding to PD-1 Blockade | ICI + FMT using ICI responder stool | Colonoscopy | ORR | Changes in: 1. T-cell composition, 2. immune system subsets, 3. T-cell function | Recruiting |
| FMT for the prevention of complications in hematologic malignancies | |||||||||
| NCT02928523 | Phase 1/2 single-arm | 20 | AML, age >18 y | ODYSSEE Study: Prevention of dysbiosis complications with autologous FMT in AML undergoing intensive treatment: A feasibility and safety study | Autologous FMT | Not specified | Auto-FMT efficacy as measured by: 1. microbiota diversity and 2. MDRB eradication | Defining a dysbiosis biosignature | Completed |
| NCT03516461 | Nonrandomized, parallel-assignment, open label | 30 | Radiation enteritis, age >18 y | Efficacy and Safety of SMT and FMT in Radiation Enteritis | SMT or FMT | NGT/NDT or gastroscopy once per day (up to 3 times) | Change of toxicity grade | 1. Scores of GI symptoms, 2. KPS | Recruiting |
| FMT for the prevention of infections in HSCT | |||||||||
| NCT03678493 | Phase 2 RCT | 120 | AML +/− allo-HSCT, age >18 y | A Randomized Placebo-Controlled Clinical Trial of FMT in Patients with AML and Allogeneic HSCT Recipients | Randomized in 2:1 ratio to receive FMT vs placebo: cohort A (AML, induction) and cohort B (Allo-HSCT) | Capsules | Efficacy of FMT measured as incidence of infections | 1. Rate of FMT engraftment, 2. acute grade II-IV GVHD, 3. BSI of suspected gut origin, 4-6. bacterial, viral, and fungal infections | Recruiting |
| NCT02269150 | Phase 2 RCT | 59 | Allo-HSCT, low bacteroidetes abundance, age >18 y | Auto-FMT for Prophylaxis of Clostridium difficile Infection in Recipients of Allo-HSCT | Autologous FMT vs routine management | Retention enema | CDI | NA | Active, not recruiting |
| FMT for the prevention of GVHD in HSCT | |||||||||
| NCT03862079 | Phase 2 RCT | 120 | Allo-HSCT, age 16-75 y | Randomized Phase 2 Trial of TGD followed by FMT, FMT-Alone, or Standard of Care for Reduction in Acute Graft-Versus-Host Disease of the Gastrointestinal Tract in Patients Given Broad-Spectrum Antibiotics | Arm A (TGD + FMT): TGD Oral piperacillin-tazobactam and nystatin until FMT; Arm B (FMT): FMT via enema within 3 wk after HSCT; Arm C (SOC): standard of care | Enema | 1. Acute GI GVHD; 2. RFS | 1.Microbiome diversity, 2. maximum stage lower GI GVHD, 3. acute GVHD, 4. AE and SAE, 5. BSI, 6. hematologic recovery, 7. characterization of the intestinal microbiota, 8. NRM, 9. OS | Not yet recruiting |
| NCT03720392 | Phase 2 double-blind RCT | 48 | Allo-HSCT, age 18-80 y | A Phase 2 Study of FMT in Recipients After Allogeneic Hematopoietic Cell Transplantation | Cohort A: FMT; cohort B: placebo capsule | Capsules | Proportion who achieve gut microbiome diversity at 1 mo | 1. Acute GVHD, 2. NRM , 3. Infection , 4. PFS, 5. OS , 6. GVHD / RFS | Recruiting |
| Other microbiota-related therapies in HSCT | |||||||||
| NCT02763033 | Phase 2 RCT | 70 | Allo-HSCT, age >9 y | Modification of the Intestinal Microbiome by Diet Intervention to Mitigate Acute Graft-Versus-Host Disease | Cohort A: potato starch; cohort B: placebo starch | Oral | Grade II-IV GVHD | NA | Recruiting |
| NCT02805075 | Phase 1 single-arm, dose escalation | 15 | Allo-HSCT, age >18 y | Single-arm Dose-Escalation Trial of Fructo-Oligosaccharides (FOS) in Patients Undergoing Allo-HSCT | FOS | Oral | Maximum tolerated dose | NA | Completed |
| NCT03039257 | Single-arm, dose escalation | 12 | Any HSCT, age >1 y | Single, High-Dose Vitamin A Replacement in Patients Undergoing HSCT and its Role on MBI-LCBI Rates | Single-dose vitamin A supplementation | Oral | Vitamin A level | MBI-LCBI | Completed |
| NCT02406651 | Phase 2a, single-arm | 27 | HSCT with grade II-IV lower GI-aGVHD, age 18-80 y | A Phase 2a Study of Recombinant Human Interleukin-22 IgG2-Fc (F652) in Combination with Systemic Corticosteroids for the Treatment of Newly Diagnosed Grade II-IV Lower GI a GVHD in HSCT | IL-22 IgG2-Fc, once per week for 4 wk + systemic corticosteroids | Intravenous (IV) | AE | 1. aGVHD response, 2.discontinuation of immunosuppressive medications, 3. OS | Active, not recruiting |
| NCT identifier . | Study type . | Sample size . | Study population . | Study name . | Patient cohorts . | Delivery route . | Primary outcome . | Secondary outcomes . | Current status . |
|---|---|---|---|---|---|---|---|---|---|
| FMT in checkpoint inhibitor therapy | |||||||||
| NCT04038619 | Phase 1 single-arm | 40 | GU malignancy +ICI colitis, age >18 y | FMT for ICI Induced Diarrhea/Colitis in Genitourinary Cancer Patients | Loperamide +FMT | Colonoscopy | 1. FMT safety and tolerability 2. Colitis response | ICI colitis recurrence | Not yet recruiting |
| NCT03772899 | Phase 1 single-arm | 20 | Melanoma + anti-PD-1 immunotherapy, age >18 y | FMT in Combination with Immunotherapy in Melanoma Patients (MIMic) | ICI + FMT | Capsules | Safety, AE | 1. Immunotherapy response rate, 2. gut microbiome changes, 3. immune blood markers, 4. urine metabolomics | Recruiting |
| NCT03353402 | Phase 1 single-arm | 40 | Melanoma stage IV or unresectable stage III, age >18 y | FMT in Metastatic Melanoma Patients Who Failed Immunotherapy | FMT using ICI responder stool | Colonoscopy and capsules | 1. FMT-related AE, 2. FMT engraftment | Changes in: 1. immune cell composition, 2. immune cell activity | Recruiting |
| NCT03341143 | Phase 2 single-arm | 20 | Advanced melanoma + anti-PD-1 nonresponders, age >18 y | Phase 2 Feasibility Study of FMT in Advanced Melanoma Patients Not Responding to PD-1 Blockade | ICI + FMT using ICI responder stool | Colonoscopy | ORR | Changes in: 1. T-cell composition, 2. immune system subsets, 3. T-cell function | Recruiting |
| FMT for the prevention of complications in hematologic malignancies | |||||||||
| NCT02928523 | Phase 1/2 single-arm | 20 | AML, age >18 y | ODYSSEE Study: Prevention of dysbiosis complications with autologous FMT in AML undergoing intensive treatment: A feasibility and safety study | Autologous FMT | Not specified | Auto-FMT efficacy as measured by: 1. microbiota diversity and 2. MDRB eradication | Defining a dysbiosis biosignature | Completed |
| NCT03516461 | Nonrandomized, parallel-assignment, open label | 30 | Radiation enteritis, age >18 y | Efficacy and Safety of SMT and FMT in Radiation Enteritis | SMT or FMT | NGT/NDT or gastroscopy once per day (up to 3 times) | Change of toxicity grade | 1. Scores of GI symptoms, 2. KPS | Recruiting |
| FMT for the prevention of infections in HSCT | |||||||||
| NCT03678493 | Phase 2 RCT | 120 | AML +/− allo-HSCT, age >18 y | A Randomized Placebo-Controlled Clinical Trial of FMT in Patients with AML and Allogeneic HSCT Recipients | Randomized in 2:1 ratio to receive FMT vs placebo: cohort A (AML, induction) and cohort B (Allo-HSCT) | Capsules | Efficacy of FMT measured as incidence of infections | 1. Rate of FMT engraftment, 2. acute grade II-IV GVHD, 3. BSI of suspected gut origin, 4-6. bacterial, viral, and fungal infections | Recruiting |
| NCT02269150 | Phase 2 RCT | 59 | Allo-HSCT, low bacteroidetes abundance, age >18 y | Auto-FMT for Prophylaxis of Clostridium difficile Infection in Recipients of Allo-HSCT | Autologous FMT vs routine management | Retention enema | CDI | NA | Active, not recruiting |
| FMT for the prevention of GVHD in HSCT | |||||||||
| NCT03862079 | Phase 2 RCT | 120 | Allo-HSCT, age 16-75 y | Randomized Phase 2 Trial of TGD followed by FMT, FMT-Alone, or Standard of Care for Reduction in Acute Graft-Versus-Host Disease of the Gastrointestinal Tract in Patients Given Broad-Spectrum Antibiotics | Arm A (TGD + FMT): TGD Oral piperacillin-tazobactam and nystatin until FMT; Arm B (FMT): FMT via enema within 3 wk after HSCT; Arm C (SOC): standard of care | Enema | 1. Acute GI GVHD; 2. RFS | 1.Microbiome diversity, 2. maximum stage lower GI GVHD, 3. acute GVHD, 4. AE and SAE, 5. BSI, 6. hematologic recovery, 7. characterization of the intestinal microbiota, 8. NRM, 9. OS | Not yet recruiting |
| NCT03720392 | Phase 2 double-blind RCT | 48 | Allo-HSCT, age 18-80 y | A Phase 2 Study of FMT in Recipients After Allogeneic Hematopoietic Cell Transplantation | Cohort A: FMT; cohort B: placebo capsule | Capsules | Proportion who achieve gut microbiome diversity at 1 mo | 1. Acute GVHD, 2. NRM , 3. Infection , 4. PFS, 5. OS , 6. GVHD / RFS | Recruiting |
| Other microbiota-related therapies in HSCT | |||||||||
| NCT02763033 | Phase 2 RCT | 70 | Allo-HSCT, age >9 y | Modification of the Intestinal Microbiome by Diet Intervention to Mitigate Acute Graft-Versus-Host Disease | Cohort A: potato starch; cohort B: placebo starch | Oral | Grade II-IV GVHD | NA | Recruiting |
| NCT02805075 | Phase 1 single-arm, dose escalation | 15 | Allo-HSCT, age >18 y | Single-arm Dose-Escalation Trial of Fructo-Oligosaccharides (FOS) in Patients Undergoing Allo-HSCT | FOS | Oral | Maximum tolerated dose | NA | Completed |
| NCT03039257 | Single-arm, dose escalation | 12 | Any HSCT, age >1 y | Single, High-Dose Vitamin A Replacement in Patients Undergoing HSCT and its Role on MBI-LCBI Rates | Single-dose vitamin A supplementation | Oral | Vitamin A level | MBI-LCBI | Completed |
| NCT02406651 | Phase 2a, single-arm | 27 | HSCT with grade II-IV lower GI-aGVHD, age 18-80 y | A Phase 2a Study of Recombinant Human Interleukin-22 IgG2-Fc (F652) in Combination with Systemic Corticosteroids for the Treatment of Newly Diagnosed Grade II-IV Lower GI a GVHD in HSCT | IL-22 IgG2-Fc, once per week for 4 wk + systemic corticosteroids | Intravenous (IV) | AE | 1. aGVHD response, 2.discontinuation of immunosuppressive medications, 3. OS | Active, not recruiting |
AE, adverse events; AML, acute myeloid leukemia; BSI, bloodstream infection; CDI, Clostridium difficile infection; FMT, fecal microbiota transplantation; FOS, fructo-oligosaccharides; GI, gastrointestinal; GVHD, graft-versus-host disease; GU, genitourinary; HSCT, hematopoietic stem cell transplantation; ICI, immune-checkpoint inhibitor; KPS, Karnofsky Performance Status; MBI-LCBI, mucosal barrier injury laboratory-confirmed bloodstream infection; MDRB, multidrug-resistant bacteria; NDT/NGT, nasoduodenal tube/nasogastric tube; NRM, nonrelapse mortality; ORR, objective response rate; OS, overall survival; PFS, progression-free survival; RFS, relapse-free survival; SAE, serious adverse events; SMT, selective microbiota transplantation; TGD, total gut decontamination.
In addition to mitigating chemotherapy and radiation effects on the host, gut microbiota alter the efficacy and toxicity of immunotherapies targeting the immune checkpoint receptors CTLA-4 and programmed death-1/programmed death ligand-1. Although much of the data have been published in patients with solid-organ malignancies, immune checkpoint inhibitors (ICIs) nivolumab and pembrolizumab are US Food and Drug Administration (FDA) approved for use in patients with Hodgkin lymphoma and are under investigation for other hematologic malignancies.10,11 Multiple studies found that the taxonomic composition of pretreatment gut microbiota is different between those patients who responded to checkpoint inhibition compared with nonresponders.12-14 Interestingly, across all studies, there was little consistency in microbial taxonomic signatures associated with response, although 1 possibility may be that important microbial functions in the gut are preserved across responders despite taxonomic variability. To examine a potential causal link between favorable gut microbiota and therapeutic efficacy, stools from human responders and nonresponders were delivered as fecal transplants to germ-free melanoma mouse models and tumor size was measured over time.12-14 Tumor growth was significantly slower in mice provided FMTs from human responders compared with nonresponders.12-14 In 1 study, antibiotic-induced dysbiosis and rapid tumor growth rate were reversed by anti–programmed death 1 immunotherapy plus Akkermansia muciniphila alone or in combination with Enterococcus hirae,12 suggesting the possibility of a microbial therapy with the potential for altering immunotherapy response.
In addition, the relative abundance of gut microbes prior to ICI treatment has been correlated with ICI-related toxicity within the gut.15,16 Notably, vancomycin-induced severe colitis in mice administered anti–CTLA-4 antibody therapy was ameliorated by the administration of a mixture of Bifidobacterium species, suggesting that gut microbiota may mitigate ICI-related toxicity.17 To date, only the results of 2 FMTs performed in patients with severe refractory anti–CTLA-4–related colitis have been reported.18 Clinical trials of FMT to improve immunotherapy response and mitigate toxicity are currently recruiting patients with solid-organ malignancies (Table 1).
FMT as treatment and prevention of complications in HSCT recipients
Microbiota modulation through FMT is increasingly being reported in case reports and pilot clinical trials of HSCT recipients as treatment of steroid-refractory or steroid-resistant gastrointestinal (GI) acute graft-versus-host disease (aGVHD). The development of GI aGVHD has long been correlated with both community- and species-level changes in the intestinal microbiota although primarily in small single-center studies (for a review of this topic, see Andermann et al19 ). Researchers have demonstrated that decreased microbial diversity at the time of engraftment is associated with higher mortality.6 The development of aGVHD and aGVHD-related mortality has also been correlated with the loss of specific obligate anaerobic bacteria such as Blautia,5 Faecalibacterium, and Bacteroidetes,20 and higher relative abundance of Enterococcus and Enterobacteriaciae.20 FMTs for steroid-refractory or steroid-resistant GI aGVHD are being performed, based on associations between microbiota composition and aGVHD outcomes demonstrated in previous studies. The first FMT study in 2016 used fecal donations from spouses and relatives and were delivered via nasoduodenal tube in 4 HSCT patients (Table 2).21 All patients noted improvements in symptoms, and 3 of the 4 experienced complete resolution of diarrhea.21 In another case study, the patient required multiple FMTs for resolution of her GI aGVHD symptoms. Of note, she was also found to have cytomegalovirus (CMV) viremia. Although viral inclusions were not observed on biopsy, it is unclear what role the treatment of CMV viremia and possible CMV colitis may have played in resolving her diarrhea. This case highlights several important critical points in the use of FMT: (i) often more than 1 or 2 FMT treatments are required for non-CDI indications, potentially increasing the risk for procedure-related complications in those receiving FMT via endoscopy or colonoscopy; and (ii) patients may start multiple therapies including antimicrobials, antivirals, or immunosuppressants at the time of FMT, making it more difficult to determine whether FMT was solely responsible for symptom resolution.
Studies of FMT in patients with hematologic malignancies
| Studies . | Indication . | Underlying disease . | Study type . | n . | Donor type . | Method of delivery . | Total number of FMTs per patient . | Primary clinical outcome . | FMT-related adverse events . | Microbiome changes . | Institutional review or regulatory approval reported . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| FMT for steroid-refractory or resistant GVHD | |||||||||||
| Kakihana et al 201621 | Steroid-resistant/dependent GI GVHD | AML + allo-HSCT | Prospective, single-center pilot | 4 | Spouse or relative | ND tube | 1-2 | 3 CR, 1 PR | No | 16S sequencing: patient 1: ↑Lactobacillus and Bacteroides, patient 2: ↓Streptococcus ↑Bacteroides, Lactobacillus, and Bifidobacterium, patient 3: ↑Bacteroides, Bifidobacterium, and Faecalibacterium, [atient 4: ↑Escherichia coli at recurrence | Approved by the institutional ethics committee |
| Spindelboeck et al 201722 | Severe steroid-refractory GI GVHD | AML and MDS + allo-HSCT | Case series | 3 | Unrelated and related | Colonoscopy | 1-6 | 2 CR, 1 PR | No | 16S sequencing: patient 1: ↑richness with resolution, patient 2: ↑richness with resolution, patient 3: ↓richness with recurrence | Approved by the ethics review board of Tokyo Metropolitan Cancer and Infectious Diseases Center, Komagome Hospital |
| Qi et al 201823 | Steroid-refractory GI GVHD | Acute and chronic leukemias and MDS + allo-HSCT | Retrospective observational cohort | 8 FMT; 8 controls | Unrelated | ND tube | 1-2 | 4 CR (cure), 2 relapse, 1 PR, 1 remission | No | 16S sequencing: ↑diversity, ↓Firmicutes and Enterococcus, ↑Bacteroidetes | Approved by the Institutional Review Board of the First Affiliated Hospital of Soochow University |
| Kaito et al 201824 | Severe steroid-refractory GI GVHD | ALL + allo-HSCT | Case study | 1 | Relative | Oral capsules of pelleted stool | 7 | 1 PR | No | 16S sequencing: ↑diversity and ↑Bacteroides, Parabacteroides, Clostridium, Faecalibacterium, Lactobacillus | A priori permission of the hospital board of the LKH Universitätsklinikum Graz and after obtaining informed consent. Publication was approved by the local institutional review board |
| FMT for the prevention of HSCT complications | |||||||||||
| Taur et al 201827 | Dysbiosis following allo-HSCT, Bacteroidetes ≦0.1% | Acute and chronic leukemias, MDS, MM, NHL + allo-HSCT | Pilot study within an RCT | FMT, n=14; no FMT, n=11 | Auto-FMT | Retention enema | 1 | NA | None | 16S and shotgun metagenomics: ↑diversity, Lachnospiraceae, Ruminococcacae, Bacteroidetes | Approved by the Memorial Sloan Kettering Cancer Center Institutional Review and Privacy Board |
| DeFilipp et al 201826 | Post-allo-HSCT | Acute and chronic leukemias, NHL, MDS, MPD, and MF + allo-HSCT | Prospective, single-arm pilot study | 13 | Unrelated | Oral capsules | 1 | 85% OS and 85% PFS. 2 deaths in total with 1 death due to acute GI GVHD | 1 SAE (grade 3 abdominal pain) | 16S sequencing: ↑diversity and expansion of stool donor taxa, ↑Clostridiales abundance | Approved by the Institutional Review Board at the Dana-Farber Harvard Cancer Center and conducted under IND 16857 |
| FMT for intestinal decolonization of MDROs | |||||||||||
| Biliński et al 201629 | Gut colonization with NDM+ Klebiella pneumoniae and ESBL+ Escherichia coli | MM + auto-HSCT | Case report | 1 | Unrelated | ND tube | 1 | NA | No | Not assessed | Reviewed and accepted by the Bioethical Committee of the Medical University of Warsaw |
| Biliński et al 201730 | MDRO gut colonization | Immunocompromised (includes hematologic malignancies, and patients post-HSCT with GVHD) | Prospective cohort | 20 (25 FMTs) | Unrelated | ND tube | 1-3 | NA | No | 16S sequencing: ↑Barnesiella, Bacteroides, and Butyricimonas, ↑richness | Approved by The Medical University of Warsaw Ethics Committee approved the research protocol |
| Innes et al 201731 | Gut colonization with carbapenemase-producing Klebsiella oxytoca | ALL, prior to allo-HSCT | Case report | 1 | Unrelated | NG tube | 1 | NA | No | Not assessed | None noted |
| Battipaglia et al 201932 | MDR gut colonization with carbapenamase + Enterobacteriaceae or Pseudomonas aeruginosa | Hematologic malignancies before or after allo-HSCT | Retrospective | 10 | Related and unrelated | Enema or NG tube | 1-2 | MA | No | Not assessed | Approved by the institutional ethics committees |
| Studies . | Indication . | Underlying disease . | Study type . | n . | Donor type . | Method of delivery . | Total number of FMTs per patient . | Primary clinical outcome . | FMT-related adverse events . | Microbiome changes . | Institutional review or regulatory approval reported . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| FMT for steroid-refractory or resistant GVHD | |||||||||||
| Kakihana et al 201621 | Steroid-resistant/dependent GI GVHD | AML + allo-HSCT | Prospective, single-center pilot | 4 | Spouse or relative | ND tube | 1-2 | 3 CR, 1 PR | No | 16S sequencing: patient 1: ↑Lactobacillus and Bacteroides, patient 2: ↓Streptococcus ↑Bacteroides, Lactobacillus, and Bifidobacterium, patient 3: ↑Bacteroides, Bifidobacterium, and Faecalibacterium, [atient 4: ↑Escherichia coli at recurrence | Approved by the institutional ethics committee |
| Spindelboeck et al 201722 | Severe steroid-refractory GI GVHD | AML and MDS + allo-HSCT | Case series | 3 | Unrelated and related | Colonoscopy | 1-6 | 2 CR, 1 PR | No | 16S sequencing: patient 1: ↑richness with resolution, patient 2: ↑richness with resolution, patient 3: ↓richness with recurrence | Approved by the ethics review board of Tokyo Metropolitan Cancer and Infectious Diseases Center, Komagome Hospital |
| Qi et al 201823 | Steroid-refractory GI GVHD | Acute and chronic leukemias and MDS + allo-HSCT | Retrospective observational cohort | 8 FMT; 8 controls | Unrelated | ND tube | 1-2 | 4 CR (cure), 2 relapse, 1 PR, 1 remission | No | 16S sequencing: ↑diversity, ↓Firmicutes and Enterococcus, ↑Bacteroidetes | Approved by the Institutional Review Board of the First Affiliated Hospital of Soochow University |
| Kaito et al 201824 | Severe steroid-refractory GI GVHD | ALL + allo-HSCT | Case study | 1 | Relative | Oral capsules of pelleted stool | 7 | 1 PR | No | 16S sequencing: ↑diversity and ↑Bacteroides, Parabacteroides, Clostridium, Faecalibacterium, Lactobacillus | A priori permission of the hospital board of the LKH Universitätsklinikum Graz and after obtaining informed consent. Publication was approved by the local institutional review board |
| FMT for the prevention of HSCT complications | |||||||||||
| Taur et al 201827 | Dysbiosis following allo-HSCT, Bacteroidetes ≦0.1% | Acute and chronic leukemias, MDS, MM, NHL + allo-HSCT | Pilot study within an RCT | FMT, n=14; no FMT, n=11 | Auto-FMT | Retention enema | 1 | NA | None | 16S and shotgun metagenomics: ↑diversity, Lachnospiraceae, Ruminococcacae, Bacteroidetes | Approved by the Memorial Sloan Kettering Cancer Center Institutional Review and Privacy Board |
| DeFilipp et al 201826 | Post-allo-HSCT | Acute and chronic leukemias, NHL, MDS, MPD, and MF + allo-HSCT | Prospective, single-arm pilot study | 13 | Unrelated | Oral capsules | 1 | 85% OS and 85% PFS. 2 deaths in total with 1 death due to acute GI GVHD | 1 SAE (grade 3 abdominal pain) | 16S sequencing: ↑diversity and expansion of stool donor taxa, ↑Clostridiales abundance | Approved by the Institutional Review Board at the Dana-Farber Harvard Cancer Center and conducted under IND 16857 |
| FMT for intestinal decolonization of MDROs | |||||||||||
| Biliński et al 201629 | Gut colonization with NDM+ Klebiella pneumoniae and ESBL+ Escherichia coli | MM + auto-HSCT | Case report | 1 | Unrelated | ND tube | 1 | NA | No | Not assessed | Reviewed and accepted by the Bioethical Committee of the Medical University of Warsaw |
| Biliński et al 201730 | MDRO gut colonization | Immunocompromised (includes hematologic malignancies, and patients post-HSCT with GVHD) | Prospective cohort | 20 (25 FMTs) | Unrelated | ND tube | 1-3 | NA | No | 16S sequencing: ↑Barnesiella, Bacteroides, and Butyricimonas, ↑richness | Approved by The Medical University of Warsaw Ethics Committee approved the research protocol |
| Innes et al 201731 | Gut colonization with carbapenemase-producing Klebsiella oxytoca | ALL, prior to allo-HSCT | Case report | 1 | Unrelated | NG tube | 1 | NA | No | Not assessed | None noted |
| Battipaglia et al 201932 | MDR gut colonization with carbapenamase + Enterobacteriaceae or Pseudomonas aeruginosa | Hematologic malignancies before or after allo-HSCT | Retrospective | 10 | Related and unrelated | Enema or NG tube | 1-2 | MA | No | Not assessed | Approved by the institutional ethics committees |
AML, acute myeloid leukemia; ATG, anti-thymocyte globulin; CR, complete remission; FMT, fecal microbiota transplant; MDRO, multidrug-resistant organisms; MDS, myelodysplastic syndrome; MF, myelofibrosis; MM, multiple myeloma; MPD, myeloproliferative disorder; ND, nasoduodenal; NDM, New Delhi metallo-β-lactamase type carbapenamase; NG, nasogastric; NHL, non-Hodgkin lymphoma; OS, overall survival; PFS, progression-free survival; PR, partial remission; SAE, serious adverse event; TPN, total parenteral nutrition; XDRO, extensively drug resistant organism.
To date, results from 16 total fecal transplants for steroid-refractory or steroid-resistant GI aGVHD have been published; 9 of these patients responded with complete resolution of their symptoms (Table 2).21-24 FMT increased both microbial diversity and the relative abundance of organisms previously associated with improved HSCT outcomes such as Faecalibacterium and Bacteroidetes (Table 2).19 Similar to FMT for CDI, methods of delivery include nasoduodenal tubes, oral capsules, and colonoscopy although safety and efficacy for each method have been compared only in patients with CDI.25 Of the published cases, none had any reported adverse events or infections attributed to FMT. Multiple single-arm trials are currently under way to determine whether FMT can be used to safely treat steroid-refractory GI aGVHD (Table 1).
FMT is also being explored for the prevention of HSCT complications. Two pilot trials have demonstrated the safety and feasibility of microbiota restoration using third-party donor and autologous FMT in HSCT patients prior to developing GVHD or infectious complications (Table 2).26,27 Randomized clinical trials (RCTs) are ongoing to determine whether FMT may function to prevent complications of dysbiosis in acute myeloid leukemia (AML) and HSCT recipients (Table 1) .
FMT for elimination of intestinal colonization with MDROs
The urgent need to find alternatives to antibiotics given the steadily rising incidence of MDRO infections has led to the exploration of FMT as a novel tool for MDRO elimination. FMT efficacy in this setting is thought to be secondary to the transfer of organisms that restore microbiome diversity and provide resistance to colonization. Mechanisms for colonization resistance, defined as the ability to inhibit the colonization and expansion of invading microbes, include microbially produced antimicrobials such as lantibiotics, and the competition for ecological niches held by pathogens including MDROs.7 Previously reported as preliminarily safe and feasible in immunocompetent individuals,28 case studies using FMT for MDRO decolonization have demonstrated promising efficacy in immunocompromised patients with cancer or undergoing HSCT (Table 2).29-32 To date, 75% (n = 24 of 32) reported patients with cancer have achieved decolonization via FMT with no detectable MDROs in follow-up rectal surveillance cultures. In many of these cases, MDROs have remained undetected for up to 6 months even after subsequent allogeneic HSCT or use of broad-spectrum antibiotics and chemotherapy. FMT therefore remains an investigational but promising method for restoring microbial diversity and eliminating MDROs in patients undergoing chemotherapy, radiation, and HSCT. In the future, the use of FMT in patients with hematologic malignancies will require balancing the benefits of MDRO decolonization with the risk of infection from MDROs absent decolonization as well as the potential risk of complications from FMT.
A critical evaluation of FMT and the need for emerging strategies
In preclinical models and small studies or case series, FMT has shown preliminary benefit in treating and preventing a variety of chemotherapy-, radiation-, immunotherapy-, and transplant-related complications, however, optimal approaches for non-CDI indications in immunocompromised patients remain unknown. RCTs comparing FMT to standard of care in patients with hematologic malignancy are greatly needed. No studies have rigorously compared the microbiota characteristics of the fecal donors to determine those of the most successful “super donors” in patients with cancer, although rational selection of donor stool taxonomic characteristics has demonstrated improved efficacy in other patient populations.33 Notably, the designation of “super donor” will be specific to patient populations and desired outcome because varied microbial signatures have been found for different diseases.
With a limited number of published cases and no RCTs comparing FMT to other therapies for non-CDI indications, FMT’s true efficacy and infectious risk remains unclear. A systematic review of 303 immunocompromised patients reported 2 colectomies, 5 episodes of bacteremia or infection, and other serious complications following FMT performed for CDI.34 In June of 2019, the FDA issued a warning regarding the potential risk of serious or life-threatening infections following invasive extended-spectrum β-lactamase–producing Escherichia coli infections in 2 immunocompromised patients, 1 of whom died.35 Furthermore, fecal donor screening for FMT in immunocompromised patients has not yet been standardized and varies widely between studies.19 Given reports of severe infection following FMT, it is even more important that clear guidelines for additional screening (for example, for MDROs) in compromised hosts are established. Alternatives to FMT in severely immunocompromised patients may be an even more compelling option for those patients at highest risk, such as those with GI aGVHD. Standardized “designer” microbial consortia composed of nonpathogenic bacterial spores have been studied, although results have been contradictory: although a phase 1 study of the standardized microbial product SER-109 appeared promising for CDI treatment, an abstract of the preliminary results from the phase 2 trial did not demonstrate similar efficacy.36,37 Additionally, sterile fecal filtrates transferred from healthy donor stool demonstrated successful treatment of CDI in all 5 patients tested.38 In the future, defined consortia or sterile fecal filtrates may serve as the safest and most efficacious alternatives to FMT in severely immunocompromised patients.
Although FMT may have promise as a treatment of conditions beyond CDI, the variability in outcomes based on undefined donor and microbiota characteristics argues for the investigation of other methods for microbiota manipulation. For that reason, probiotics and prebiotics have been studied as potential therapies in patients with hematologic malignancies, and will be reviewed in the next sections.
Why probiotics? Changing cancer outcomes using precision medicine
As an alternative to complex, poorly defined live microbial therapies such as FMT, probiotics are isolated viable organisms administered to confer a health benefit on the host. Clinical studies of probiotics in patients with cancer have been primarily focused on the amelioration of adverse effects following chemotherapy and radiation. In 2018, a Cochrane Review of patients receiving probiotics for chemotherapy- or radiation-related diarrhea found only 25% of studies demonstrating efficacy in preventing severe diarrhea.39 Notably, heterogeneity in patient population, probiotic strain, and probiotic dose makes it difficult to generalize to other patient populations or other probiotic products.
In HSCT, preclinical and clinical studies of probiotics show inconsistent clinical outcomes. Lactobacillus-containing probiotics have been tested for prevention of GVHD in murine models and in patients undergoing allogeneic HSCT. Although a study in mice demonstrated increased survival and reduced aGVHD with the administration of Lactobacillus rhamnosus GG,40 this same probiotic was tested in HSCT patients in a randomized clinical trial and was found not to alter gut microbiota composition or GVHD incidence.41 Colonization resistance by established recipient microbiota may be 1 major contributing factor to the lack of probiotic efficacy in many cases due to the baseline variability in human microbiota.42 Potential harms of probiotics in immunocompromised patients are also increasingly being recognized including bloodstream infections with organisms commonly found in probiotics.43,44
In the future, precision medicine efforts may be directed toward the development of probiotics targeted for specific immunomodulatory effects. For example, probiotic consortia are being isolated based on their ability to induce proinflammatory interferon γ–positive CD8+ T cells45 and to improve ICI efficacy.12 Probiotic development will also likely require “precision matching” by taking into account microbiota features unique to each disease and each patient. Precise targeting of microbial therapies that takes into account underlying disease and patients’ unique microbiota features may help to overcome the colonization resistance to probiotic colonization due to patients’ baseline microbiota variability.42 It is expected that more of these novel targeted probiotic therapies will become available for clinical use; once they are deemed medical foods or drugs, they will likely be subject to higher thresholds for quality and efficacy testing. In contrast, prebiotics, dietary fibers fermented by gut microbiota that alter microbiota composition, would likely minimize the risk of infections in severely immunocompromised populations, and are reviewed in the section that follows.
Microbially targeted dietary therapies
Why prebiotics? Microbial substrates and metabolites that influence outcomes in hematology
Prebiotics are historically defined as dietary fibers that are fermented by microbes and contribute to health but are nondigestible by humans. Examples of these fibers include resistant starches, fructo-oligosaccharides (including inulin), and galacto-oligosaccharides, which are found in a variety of foods including onions, oats, garlic, asparagus, and human milk. Although growing evidence suggests a link between the diet, microbiota, and clinical outcomes,46,47 we have a limited understanding of how dietary compounds might support the expansion of specific gut microbes to impact host health. Only a single study of prebiotics in patients undergoing HSCT has been published to date.48 Authors found a decrease in the number of days of diarrhea and the use of IV hyperalimentation in 22 patients who received fructo-oligosaccharide–containing prebiotics compared with controls, but without an effect on GVHD rates.48 Importantly, patients in the study also received Lactobacillus as part of standard care. Two clinical trials, 1 investigating the impact of a prebiotic potato starch on GVHD risk is currently enrolling (NCT02763033), and a prospective dose-escalation trial to determine the tolerability of fructo-oligosaccharide prebiotics in HSCT patients was recently completed; results are pending (NCT02805075) (Table 1).
Although data exploring how prebiotics influence outcomes in patients with hematologic malignancies are limited, there are several important studies highlighting the mechanism of their effect on gut mucosa and host immune response mediated by the intestinal microbiota. Prebiotics are metabolized by select gut microbes to generate a variety of compounds through fermentation, including the short-chain fatty acids (SCFAs) butyrate, acetate, and propionate. SCFAs affect the host by (i) serving as a direct substrate for intestinal epithelial metabolism and maintenance of the mucosal barrier, (ii) affecting immune cell signaling and proliferation, (iii) altering epigenetic modifications, (iv) impacting microbial-microbial and microbial-host interactions, and (v) influencing chemotherapy efficacy and toxicity.
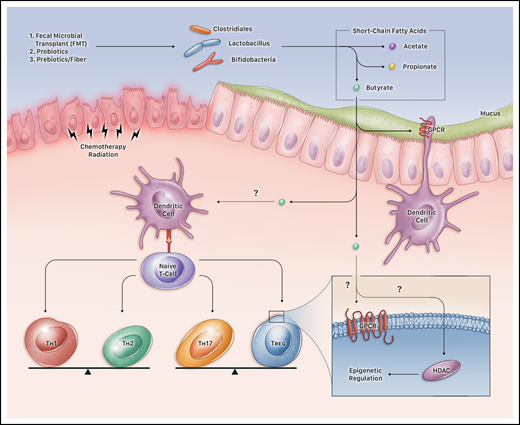
Butyrate and related SCFAs are major products of prebiotic metabolism,49 and are a preferred energy source for the colonic epithelium.50,51 Butyrate also upregulates claudins and occludins comprising tight junctions between epithelial cells, and triggers signaling molecules such as hypoxia-inducible factor 1 subunit α to maintain barrier function.52 Additionally, SCFAs also appear to alter the signaling of host immune cells: butyrate in the colonic lumen is thought to increase the proliferation of host regulatory T cells (T-regs)53,54 and to activate dendritic cells through signaling via chemokine G-protein–coupled receptors55 (Figure 1). The resulting differentiation of naive T cells into T-regs functions to suppress other immune cells that may induce inflammation.53
Microbiota impact on the immune system. FMT, probiotics, and prebiotics impact the immune system through production of SCFAs such as butyrate, propionate, and acetate. These microbiota-altering therapies likely abrogate and prevent damage to intestinal mucosal integrity resulting from chemotherapy and radiation in patients with hematologic malignancies and those undergoing HSCT. For example, butyrate is a source of nutrition for intestinal epithelial cells, and interacts with dendritic cells through G-protein–coupled receptors (GPCRs) and other mechanisms to induce naive T cells to differentiate into different subtypes of T-regs. T-regs are influenced directly by the local fecal concentrations of SCFAs such as butyrate that can have downstream epigenetic modulatory effects, altering histone acetylation via histone deacetylase (HDAC) and DNA methylation, which may have an effect on colon cancer tumorigenesis and leukemia prognosis.
Microbiota impact on the immune system. FMT, probiotics, and prebiotics impact the immune system through production of SCFAs such as butyrate, propionate, and acetate. These microbiota-altering therapies likely abrogate and prevent damage to intestinal mucosal integrity resulting from chemotherapy and radiation in patients with hematologic malignancies and those undergoing HSCT. For example, butyrate is a source of nutrition for intestinal epithelial cells, and interacts with dendritic cells through G-protein–coupled receptors (GPCRs) and other mechanisms to induce naive T cells to differentiate into different subtypes of T-regs. T-regs are influenced directly by the local fecal concentrations of SCFAs such as butyrate that can have downstream epigenetic modulatory effects, altering histone acetylation via histone deacetylase (HDAC) and DNA methylation, which may have an effect on colon cancer tumorigenesis and leukemia prognosis.
SCFAs not only influence immune regulation, they can also act as histone deacetylase (HDAC) inhibitors that change DNA structure and transcription, altering leukocytes and potentially affecting cancer56 and infection risk57 (Figure 1). Epigenetic changes are recognized as important driving factors in colon cancer and other solid-organ malignancies, but are increasingly implicated in hematologic malignancies like AML58 and may be affected by the gut microbiota. For example, DNA-methyltransferase function is altered in germ-free mice59 and mutations in DNA methyltransferase in adult patients with AML are associated with poor prognosis.60 Given that select microbes may influence epigenetic modifications in their host, knowing which organisms are present within the microbiota may be important, especially in those trials using agents that act through epigenetic priming.
Prebiotics not only impact the risk of infection and GVHD, but also may influence chemotherapy efficacy and toxicity likely through cellular signaling pathways influenced by SCFA production. For example, diet may decrease chemotherapy toxicity: in 1 study, soybean fiber reduced methotrexate-induced diarrhea and anorexia in patients with cancer,61 and in another, the combination of oat fiber and pectin reduced methotrexate-related enterocolitis.62,63 In rats given oligosaccharides, irinotecan-associated gut toxicity was strongly inversely correlated with butyrate production.64
Milk oligosaccharides improve cancer risk and HSCT outcomes
The most significant role of prebiotics in patients with hematologic malignancies has been demonstrated in studies of children. The consumption of human milk by babies is correlated with a decreased risk of developing acute lymphocytic leukemia in childhood.65 One hypothesis suggests that leukemia risk may be decreased by antibodies present in milk as well as by naturally occurring prebiotic milk galacto-oligosaccharides that promote the growth of organisms important for reducing cancer risk.
Decreased gut inflammation through the consumption of human milk may be most effective in reducing adverse outcomes in children undergoing HSCT. A pilot study of 46 children receiving an allogeneic HSCT showed that compared with standard formula, human milk decreases markers of intestinal inflammation and lowers the prevalence of potentially pathogenic species detectable in stool samples.66 This same study found a decrease in both proinflammatory (IL-8 and interferon-γ) and anti-inflammatory (IL-10) cytokines in the patients provided human milk. In contrast, those who received standard formula were found to have increased levels of both proinflammatory CD8+ T cells and markers of intestinal injury (eg, REG3α). Despite these differences, however, fecal levels of butyrate and propionate were the same between groups.66 Further work is under way to identify the most immune-modulating components of human milk. For example, breast milk is a source of epidermal growth factor (EGF); in a preclinical model, EGF from breast milk was found to decrease rates of necrotizing enterocolitis through inhibition of intestinal Toll-like receptor 4 signaling.67 In addition, the risk of grade III/IV aGVHD correlated with EGF plasma concentrations in a study demonstrating that patients with low levels of EGF at day +28 after HSCT had an increased risk of death by 1 year compared with individuals with higher levels of EGF.68
Emerging strategies for prebiotics
In December of 2016, the definition of a prebiotic was refined to include not only resistant starches and oligosaccharides, but also any “substrate that is selectively utilized by host microorganisms to confer a health benefit.”69 Recent studies have investigated the impact of nonfiber dietary supplements such as vitamin A on both microbiota composition and HSCT outcomes. Currently, retinoids such as all-trans retinoic acid and isotretinoin are used in the treatment of acute promyelocytic leukemia and neuroblastoma, although recent work suggests that retinoids may also prevent GVHD and gut microbial dysbiosis. In a small cohort of 114 children, vitamin A levels in patients 30 days after HSCT predicted the incidence of GVHD.70 One hypothesis suggests that vitamin A may lead to the differentiation of naive T-cells into T-regs rather than Th-17 cells, facilitating mucosal tolerance and improving mucosal barrier integrity by ameliorating gut mucosal “leakiness.” Similarly, commensal bacteria may suppress retinoid metabolism in the intestinal epithelium to lower IL-22 levels and to prevent dysbiosis.71 The relationship between retinoid metabolism, IL-22 levels, and GVHD is further supported by the finding that IL-22 levels were increased in children with GI aGVHD.72 An open-label trial of vitamin A supplementation in 12 pediatric and young adult HSCT recipients was just completed (NCT03039257) and another trial directly administering IL-22 Fc as a potential therapy to attenuate GI GVHD is ongoing (NCT02406651) (Table 1).
Summary: returning to our clinical case
In the original case, our patient received a FMT for steroid-refractory GI GVHD resulting in a complete response. The use of FMT for non-CDI indications remains in the early stages of investigation, although case reports and pilot studies are encouraging. Given that we only have limited data from FMT for non-CDI indications in immunocompromised patients, more information is needed in larger clinical trials to determine clinical efficacy as well as the true risk of infection and adverse events attributable to FMT.
In the future, precisely characterizing an individual’s microbiome may be important for predicting patients’ treatment outcomes and the risk of complications. Not unlike the use of genetic testing to guide chemotherapy regimens, we may characterize microbiota composition and function to better tailor our therapies while minimizing adverse effects. With current technologies, it is not yet practical to fully characterize the microbiota in real time, however, improvements in sequencing and computational pipelines may allow for real-time assays that evaluate microbiota dynamics to influence clinical decision-making. For example, PCR-based technologies that identify cell-free microbial DNA in patients’ blood are being developed commercially to rapidly respond to potential infectious agents. Although PCR may work to identify individual organisms, it may not be adequate to understand functional and community-level properties of the microbiota that may even be more important than taxonomic identification. Whether a single organism or the microbial ecosystem as a whole matters more in affecting outcomes for cancer patients remains to be seen, although the improved efficacy of FMT over probiotics for CDI argues that the use of a single organism is unlikely to reverse the effects of antibiotics and chemotherapy on the microbiota. These efforts toward precision medicine will require more in-depth characterization of host microbial compositional and functional status. As the technology of microbial genomics advances, we may be able to understand microbial community dynamics in real time and more rapidly and effectively impact outcomes in patients with cancer.
Acknowledgments
The authors sincerely thank Ami S. Bhatt, who assisted in reviewing the manuscript and providing invaluable feedback.
This work was supported in part by National Institutes of Health (NIH) National Center for Advancing Translational Science Awards KL2 TR001083 and UL1 TR001085, the American Society of Blood and Marrow Transplantation New Investigator Award (T.M.A.), and the Amy Strelzer Manasevit Award (T.M.A.). C.J.S. is a Stanford Maternal & Child Health Research Institute (MCHRI) Pete and Arline Harman Fellow and receives funding from the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases (T32 DK098132).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Authorship
Contribution: C.J.S. and T.M.A. performed the literature review and wrote the manuscript; R.B. designed and created the figure; and all authors reviewed and edited the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests. Off-label drug use: None disclosed.
Correspondence: Tessa M. Andermann, Division of Infectious Diseases, Department of Medicine, School of Medicine, University of North Carolina at Chapel Hill, 2115 Bioinformatics Bldg, 130 Mason Farm Rd, CB#7030, Chapel Hill, NC 27514; e-mail: tessa_andermann@med.unc.edu.
References
Author notes
This article was selected by the Blood Advances and Hematology 2019 American Society of Hematology Education Program editors for concurrent submission to Blood Advances and Hematology 2019. It is reprinted in Hematology Am Soc Hematol Educ Program. 2019;2019:303-314.