Key Points
Flt3L is a biomarker of progenitor cell mass in AML.
Measurement of Flt3L during induction chemotherapy and follow-up provides prognostic information.
Abstract
Fms-like tyrosine kinase 3 (Flt3) is expressed on progenitor cells and acute myeloid leukemia (AML) blasts. Fms-like tyrosine kinase 3 ligand (Flt3L) is detectable during homeostasis and increases in hypoplasia due to genetic defects or treatment with cytoreductive agents. Conversely, Flt3+ AML is associated with depletion of Flt3L to undetectable levels. After induction chemotherapy, Flt3L is restored in patients entering complete remission (CR) but remains depressed in those with refractory disease. Weekly sampling reveals marked differences in the kinetics of Flt3L response during the first 6 weeks of treatment, proportionate to the clearance of blasts and cellularity of the bone marrow. In the UK NCRI AML17 trial, Flt3L was measured at day 26 in a subgroup of 140 patients with Flt3 mutation randomized to the tyrosine kinase inhibitor lestaurtinib or placebo. In these patients, attainment of CR was associated with higher Flt3L at day 26 (Mann-Whitney UP < .0001). Day 26 Flt3L was also associated with survival; Flt3L ≤291 pg/mL was associated with inferior event-free survival (EFS), and Flt3L >1185 pg/mL was associated with higher overall survival (OS; P = .0119). The separation of EFS and OS curves increased when minimal residual disease (MRD) status was combined with Flt3L measurement, and Flt3L retained a near-significant association with survival after adjusting for MRD in a proportional hazards model. Serial measurement of Flt3L in patients who had received a hematopoietic stem cell transplant for AML illustrates the potential value of monitoring Flt3L to identify relapse. Measurement of Flt3L is a noninvasive test with the potential to inform clinical decisions in patients with AML.
Introduction
Acute myeloid leukemia (AML) is a high-risk malignancy with fewer than one-third of patients surviving at 5 years.1,2 Despite intensive chemotherapy, therapeutic resistance and relapse are the main causes of treatment failure. The early identification of primary treatment refractoriness is especially challenging and independent of standard clinical, cytogenetic, and molecular risk factors,3 even with integrated molecular genetic information.4 Large multicohort studies show that ≤30% of younger patients have primary refractory disease or relapse-free survival (RFS) ≤3 months, rising to 40% with RFS ≤6 months and 57% with RFS ≤1 year.3 A limited ability to predict a poor therapeutic response, in spite of advances in genetic risk profiling and minimal residual disease (MRD) detection, continues to impede the delivery of risk-adapted therapy.5-7 Salvage after relapse is also disappointing, with <50% achieving a subsequent complete remission (CR), leading to median survivals of <1 year.8 Outcomes are considerably worse for patients >60 years, who constitute the majority of cases.9
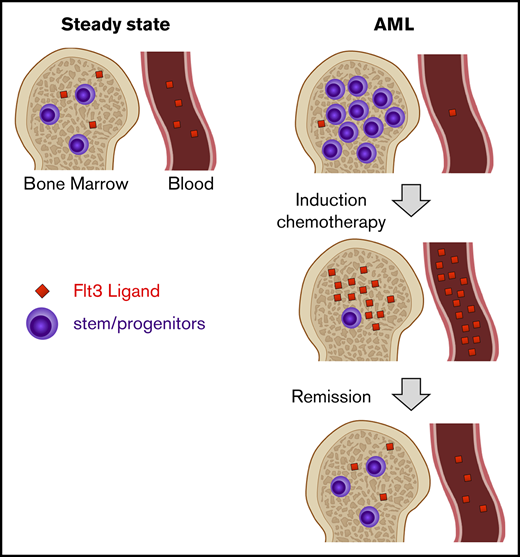
Fms-like tyrosine kinase 3 (Flt3) ligand (Flt3L) is a growth factor involved in the maintenance and proliferation of hematopoietic stem and progenitor cells.10 Its receptor, Flt3 (CD135), is a tyrosine kinase expressed predominantly on primitive CD34+ CD38low progenitor fractions.11 Several lines of evidence indicate that Flt3L rises when the hematopoietic stem cell compartment is compromised. Flt3L is increased in Fanconi anemia, acquired aplastic anemia, chemotherapy- or radiotherapy-induced aplasia, and heterozygous GATA2 mutation.12-17 Elevated Flt3L was also observed in patients with AML at day 15 of treatment and shown to be a potential mechanism of resistance to therapy with Flt3 inhibitors.10
Conversely, suppression of Flt3L in association with expansion of hematopoietic progenitors has not been reported. Previous studies investigating hypercellularity associated with myelodysplastic syndrome (MDS) lacked a sufficiently sensitive enzyme-linked immunosorbent assay (ELISA) to determine levels much below the normal range.18 Mobilization of peripheral blood stem cells with granulocyte colony-stimulating factor is paradoxically associated with a slight elevation of Flt3L.19,20 An inverse relationship between Flt3L and cells bearing its receptor might be predicted from the molecular control of other elements of hematopoiesis such as platelets.21
Here, we show that the presence of CD135+ AML blasts is associated with significant depression of Flt3L and that measurement of this biomarker may have utility in diagnosis, early assessment of response to therapy, and monitoring of remission status.
Methods
Single-center patients and controls
Patients with heterozygous mutation of GATA2, aplastic anemia, MDS, and AML were recruited from the Northern Centre for Cancer Care, Freeman Hospital, Newcastle upon Tyne Hospitals NHS Foundation Trust under ethical permission from the Newcastle and North Tyneside Research Ethics Committee 1 Reference 08/H0906/72 (cohort A). Informed consent was obtained in accordance with the Declaration of Helsinki. Additional patients with AML were recruited from Johns Hopkins Sydney Kimmel Comprehensive Cancer Center, Baltimore under the institutional review board–approved protocol J10145. A total of 84 patients were recruited at Newcastle, United Kingdom and 8 at Johns Hopkins, Baltimore, MD (cohort B). All but 2 patients received intensive induction chemotherapy with cytarabine in combination with daunorubicin, etoposide, or mitoxantrone. Details of all patients included in the study under these protocols are summarized in supplemental Table 1. Healthy control blood was obtained from volunteer donors.
AML17 patients
The UK NCRI AML17 study (ISRCTN 55675535) was a large, prospective phase 3 multicenter trial for patients with newly diagnosed AML or high-risk MDS (≥10% marrow blasts) that ran 2009-2014 at >130 centers in the United Kingdom, Denmark, and New Zealand, recruiting 3583 patients.22,23 325 patients with Flt3 mutation were randomized 2:1 to receive lestaurtinib (CEP701); 140 of those randomized provided a blood sample at day 26 for measurement of Flt3L. 5 patients were excluded from the analysis of CR/no CR, because these data were missing. MRD determined by reverse transcription quantitative polymerase chain reaction (RT-qPCR) for mutated NPM1 was performed on 2 samples of bone marrow (BM) only, 24 samples of paired BM and peripheral blood, and 30 samples of peripheral blood only. The result was defined as positive if, from any source, there was amplification in ≥2 of 3 replicates with cycle-threshold values of ≤40 in samples achieving ABL1 control amplification within 30 cycles according to Europe Against Cancer criteria.24 Flow cytometry MRD was performed centrally on peripheral blood or BM using a standardized gating strategy that screened for leukemia-associated immunophenotypes with sensitivity of detection of 0.2% to 0.05%, as described previously.25
Flt3L ELISA
Serum Flt3L was measured with quantikine human Flt3/Flk-2 ligand immunoassay according the manufacturer’s instructions (R&D Systems).
Flow cytometry
BM or peripheral blood blasts were prepared with ficoll gradients and stained in aliquots of ∼1 million cells. Antibodies were from BD Biosciences (www.bdbiosciences.com) unless stated otherwise and are denoted as: antigen fluorochrome (clone), CD3 fluorescein isothiocyanate (FITC) (SK7), CD10 phycoerythrin (PE)–Texas red (B-Ly6; Beckman Coulter; www.beckmancoulter.com), CD14 FITC (M5E2), CD16 FITC (NKP15/Leu-11a), CD19 FITC (4G7), CD20 FITC (L27), CD34 APCCy7 (581), CD38 PECy7 (HB7), CD45 V450 (2D1), CD45RA BV510 (HI100; BioLegend), CD56 FITC (NCAM16.2), CD90 PerCPCY5.5 (5E10; BioLegend), CD123 PerCPCY5.5 (7G3), and CD135 PE (4G8), HLA-DR V500 (L243/G46-6). Events were acquired with a BD Biosciences Fortessa X20 running Diva version 8 and analyzed with Tree Star FlowJo version 7.6.5. Blasts were identified as a high forward scatter/side scatter lineage-negative population and median fluorescence intensity (MFI) of CD135 was calculated by subtraction of an appropriate isotype control.
Statistical analyses
Figures were plotted in R (version 3.0.1; http://www.r-project.org/) or Prism (version 7.0d; GraphPad Software). All statistical analyses for AML17 patient data were carried out in R 3.0.1. Date of death was used to calculate overall survival (OS). Event-free survival (EFS) events were defined as failure to achieve CR, disease relapse, or death from any cause. For both survival end points, patients without a date of relapse or death were censored at the date of last visit or the date at which patients were last known to be alive. Remission status was measured using 7 categories, namely CR, death before chemotherapy started, induction death, resistant disease, Partial remission, CR with incomplete count recovery, and other. Remission status was then dichotomized into CR vs non-CR. The optimal cut point separating patients in CR from those with no CR was defined by the Youden method using the receiver operating characteristic (ROC) analysis in the R package Optimal Cutpoints.26 We then plotted a ROC curve for this cut point and determined the area under the curve (AUC), sensitivity, and specificity. The R package Survminer was then used to determine the optimal cut point for OS and EFS based on the maximally selected log-rank statistic. The 2 survival curves split by this cut point were then plotted using the descriptive Kaplan-Meier method with the log-rank P value.
Results
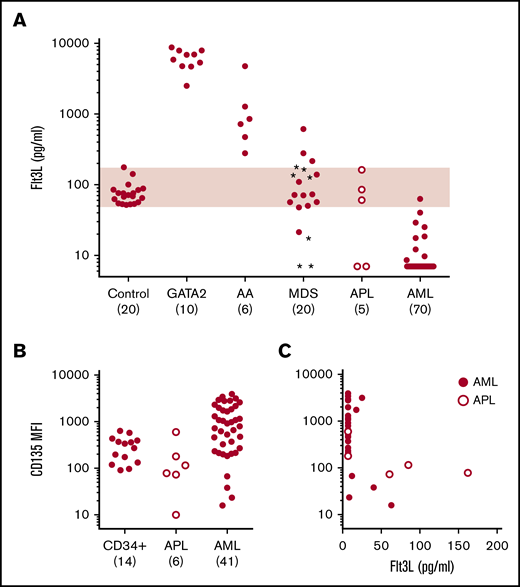
Association of Flt3L with progenitor cell mass and Flt3 expression in AML
The relationship between Flt3L level and progenitor cell mass was explored in a number of distinct patient groups recruited at the Newcastle center, including cohort A patients with AML (Figure 1A). As reported previously, patients with hypoplasia of the hematopoietic stem/progenitor compartment due to aplastic anemia or germline GATA2 mutation have very elevated serum Flt3L.12,13,16,17 A cohort of ambulatory patients with MDS showed increased variance of Flt3L levels, while patients admitted for treatment of AML mostly had low or undetectable levels of Flt3L. A potential link between decreasing Flt3L and progression to AML was suggested by the observation that although patients with excess blasts had a range of Flt3L levels (Figure 1A, asterisks), the 3 MDS patients with the lowest Flt3L (≤21 pg/mL) progressed to AML within 6 months. Of 75 consecutive patients admitted for treatment of AML, 71 had Flt3L below the level of healthy controls (range, 48.3-173.8 pg/mL; n = 20) and 63 had Flt3L below the limit of detection of 7 pg/mL. Further clinical details of patients with AML are given in supplemental Table 1.
Association of Flt3L with progenitor cell mass and Flt3 expression in AML cohort A. (A) Serum Flt3L measured by ELISA in healthy controls (range, 48.3-173.8 pg/mL; shaded region), individuals with heterozygous germline GATA2 mutation, acquired aplastic anemia (AA), MDS, APL (open symbols), and AML. Asterisks in the MDS cohort indicate patients with excess blasts. Where Flt3L was reported as undetectable, data were set to the limit of detection at 7 pg/mL. Numbers in each cohort are shown in parentheses. (B) Level of Flt3 (CD135) expression indicated by MFI (minus isotype control) in control CD34+ BM progenitors, APL blasts, and AML blasts. The numbers in each cohort are indicated in parentheses. Note MFI is a log scale. (C) Inverse relationship between CD135 expression and Flt3L in 14 AML and 4 APL patients in whom both measurements were performed.
Association of Flt3L with progenitor cell mass and Flt3 expression in AML cohort A. (A) Serum Flt3L measured by ELISA in healthy controls (range, 48.3-173.8 pg/mL; shaded region), individuals with heterozygous germline GATA2 mutation, acquired aplastic anemia (AA), MDS, APL (open symbols), and AML. Asterisks in the MDS cohort indicate patients with excess blasts. Where Flt3L was reported as undetectable, data were set to the limit of detection at 7 pg/mL. Numbers in each cohort are shown in parentheses. (B) Level of Flt3 (CD135) expression indicated by MFI (minus isotype control) in control CD34+ BM progenitors, APL blasts, and AML blasts. The numbers in each cohort are indicated in parentheses. Note MFI is a log scale. (C) Inverse relationship between CD135 expression and Flt3L in 14 AML and 4 APL patients in whom both measurements were performed.
Clinical variables were explored in order to try to understand the reason for Flt3L suppression in most, but not all, cases of AML. Although there was a clear inverse relationship between percentage of BM blasts and Flt3L across all disease groups, there were no statistically significant relationships within the AML cohort between white blood cell count at diagnosis, blast percentage in BM, cytogenetics, presence of Flt3 internal tandem duplication (ITD), blast phenotype, and disease stage (supplemental Figure 1). The only notable feature was an association between the diagnosis of acute promyelocytic leukemia (APL) or the presence of t(15;17) in patients with normal Flt3L. There were 5 cases of APL, of which 3 had normal Flt3L, compared with only 1 of 70 cases of non-APL.
The expression of Flt3 (CD135) on AML blasts was analyzed by flow cytometry in a subset of patients shown in Figure 1A, including the 5 patients with APL. This confirmed that Flt3 was expressed at a lower level on APL than most AML blasts (Figure 1B) and that there was an approximate inverse relationship between the expression of Flt3 and the level of Flt3L across all cases (Figure 1C).
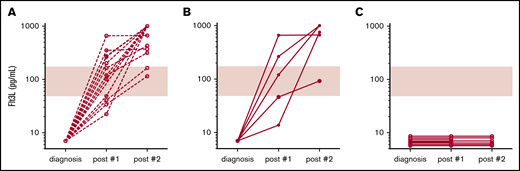
Association of Flt3L with remission assessment postchemotherapy
Further samples, following 2 rounds of intensive chemotherapy, were available from 28 patients in cohort A (Newcastle) who had undetectable Flt3L at diagnosis. These were taken at the time of remission assessment, between 28 and 42 days after the start of each round of chemotherapy. Fifteen patients were in morphological CR after both courses of chemotherapy and showed recovery of Flt3L to normal or supranormal levels at both time points (Figure 2A). A further 8 patients did not achieve morphological CR after the first course but subsequently entered remission after the second course (daunorubicin and cytarabine or fludarabine, cytarabine, and idarubicin salvage) (Figure 2B). In contrast, Flt3L remained suppressed in 5 patients who did not enter CR after 2 cycles of chemotherapy. In addition, 3 patients thought to be in morphological CR after the first course failed to show any appreciable recovery of Flt3L after either course 1 or course 2. These patients all relapsed within 6 months of diagnosis at 114 to 172 days compared with RFS of 317 to 825 days for patients in A and B, whose Flt3L was elevated after treatment (Figure 2C).
Serial serum Flt3L measurements in AML patients. (A) Patients were sampled at diagnosis and following each of 2 cycles of intensive chemotherapy with daunorubicin and cytarabine (3+10) or fludarabine, cytarabine, and idarubicin (cohort A, Newcastle; shaded regions indicate normal range). Patients who entered continuing morphological CR after 2 courses maintained increasing Flt3L at remission assessments performed 28 to 42 days after the start of chemotherapy (range of detection, 7-1000 pg/mL; n = 15; broken lines). (B) Patients who did not achieve morphological CR after the first course of chemotherapy but subsequently entered remission after the second also demonstrated increasing Flt3L over both cycles (n = 5; filled circles and solid lines). (C) Patients who remained refractory after 2 courses of chemotherapy had undetectable Flt3L (n = 5; open circles and solid lines). The graph also includes a further 3 patients thought to be in morphological CR after the first course of chemotherapy who experienced relapse within 6 months.
Serial serum Flt3L measurements in AML patients. (A) Patients were sampled at diagnosis and following each of 2 cycles of intensive chemotherapy with daunorubicin and cytarabine (3+10) or fludarabine, cytarabine, and idarubicin (cohort A, Newcastle; shaded regions indicate normal range). Patients who entered continuing morphological CR after 2 courses maintained increasing Flt3L at remission assessments performed 28 to 42 days after the start of chemotherapy (range of detection, 7-1000 pg/mL; n = 15; broken lines). (B) Patients who did not achieve morphological CR after the first course of chemotherapy but subsequently entered remission after the second also demonstrated increasing Flt3L over both cycles (n = 5; filled circles and solid lines). (C) Patients who remained refractory after 2 courses of chemotherapy had undetectable Flt3L (n = 5; open circles and solid lines). The graph also includes a further 3 patients thought to be in morphological CR after the first course of chemotherapy who experienced relapse within 6 months.
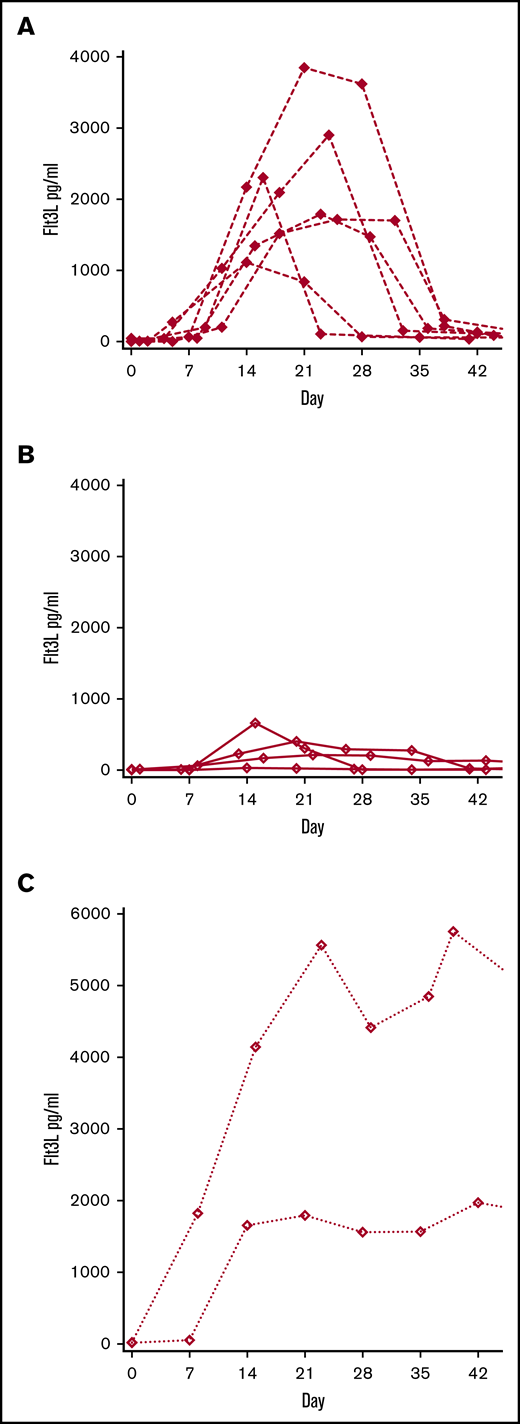
Kinetics of Flt3L response during induction chemotherapy
The preceding data suggest that the level of Flt3L was highly discriminatory between a state of normal hematopoiesis and the presence of CD135+ AML blasts. Undetectable Flt3L appeared to associate with resistant or refractory disease when measured between courses of chemotherapy at the time of remission assessments by BM aspiration. Weekly sampling was then performed in a subset of 12 non-APL AML patients (4 in cohort A and 8 in cohort B) in order to determine whether it might be possible to predict remission status from the kinetics of Flt3L response. Six patients who eventually achieved CR showed Flt3L elevation of 1000 to 4000 pg/mL, peaking between days 14 and 21 and returning to the normal range after chemotherapy (Figure 3A). In contrast, 4 patients who did not enter CR showed more modest elevations of <1000 pg/mL that subsequently dropped back to below normal or undetectable levels at day 42 (Figure 3B). Two patients in the series remained pancytopenic after chemotherapy induction and were found to be have hypocellular BMs without detectable blasts. In these cases, Flt3L remained high (>1000 pg/mL) (Figure 3C). One was salvaged by hematopoietic stem cell transplantation, but the other died of sepsis without any count recovery.
Kinetics of Flt3L response during induction. Sequential patients with weekly measurement of Flt3L during induction chemotherapy (n = 12; 4 in cohort A and 8 in cohort B). Dotted line indicates the timing of a single Flt3L measurement in patients treated on the AML17 trial. (A) Weekly Flt3L in 6 patients entering CR following induction chemotherapy (B) Weekly Flt3L in 4 patients with refractory disease or partial response following induction chemotherapy. (C) Weekly Flt3L in 2 patients rendered aplastic by induction chemotherapy
Kinetics of Flt3L response during induction. Sequential patients with weekly measurement of Flt3L during induction chemotherapy (n = 12; 4 in cohort A and 8 in cohort B). Dotted line indicates the timing of a single Flt3L measurement in patients treated on the AML17 trial. (A) Weekly Flt3L in 6 patients entering CR following induction chemotherapy (B) Weekly Flt3L in 4 patients with refractory disease or partial response following induction chemotherapy. (C) Weekly Flt3L in 2 patients rendered aplastic by induction chemotherapy
Analysis of AML17 CR and survival according to course 1 Flt3L
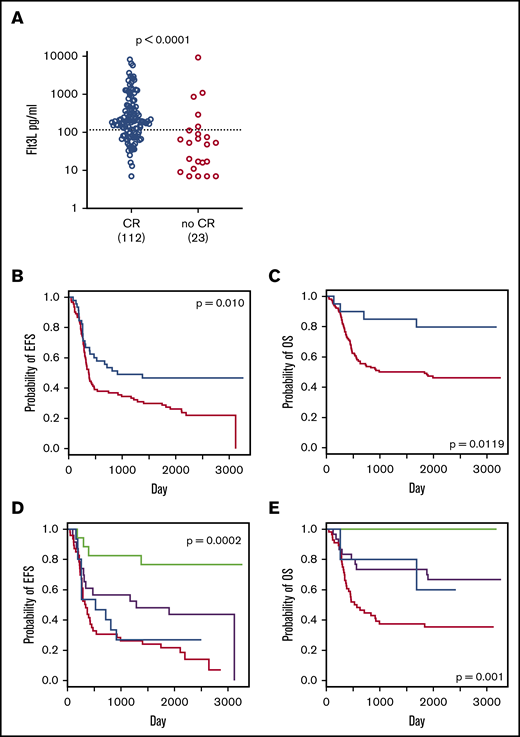
Weekly sampling in 12 patients suggested that the response of Flt3L to chemotherapy might predict attainment of CR. In order to test this in a larger cohort, we reanalyzed Flt3L levels at day 26 of induction recorded in 140 patients with Flt3 ITD or kinase domain mutation who were treated within the UK NCRI AML17 trial. In these patients, a single Flt3L measurement was performed at day 26 of induction, following 10 days of chemotherapy and 14 days of either tyrosine kinase inhibitor lestaurtinib or placebo.23 A CR status post course 1 was reported in 135 of 140 patients. We first analyzed Flt3L in relation to attainment of CR and found a significantly lower median level in patients not achieving CR, including 4 patients with undetectable levels (Figure 4A). A ROC curve identified an optimal cut point of 116 pg/mL with AUC of 0.735, sensitivity of 0.721, and specificity of 0.737. There was no difference in Flt3L according to randomization to lestaurtinib or NPM1 mutation status (not shown).
Association between Flt3L and post–course 1 remission and survival. Serum Flt3L was measured on day 26 of induction in non-APL AML patients with Flt3 mutation randomized to lestaurtinib (days 11-24) on the UK NCRI AML17 trial. (A) Serum Flt3L at day 26 in patients who subsequently achieved or did not achieve CR. Dotted line indicates optimal cut point identified by the ROC curve: 116 pg/mL (Mann-Whitney UP value). (B) EFS of subgroups with serum Flt3L level ≥291 pg/mL (blue line) or <291 pg/mL (red line). Events include failure to achieve CR and relapse or death from any cause. Threshold of Flt3L for maximum discrimination identified by log-rank testing (log-rank P value). (C) OS of subgroups with a serum Flt3L level ≥1185 pg/mL (blue line) or <1185 pg/mL (red line). Threshold of Flt3L for maximum discrimination identified by log-rank testing (log-rank P value). (D) EFS of subgroups divided according to Flt3L level ≥291 pg/mL and MRD negative (green line, n = 17), ≥291 pg/mL and MRD positive (blue line, n = 15), Flt3L <291 pg/mL and MRD negative (black line, n = 23), or <291 pg/mL and MRD positive (red line, n = 46) (log-rank P value). (E) OS of subgroups divided according to Flt3L level ≥1185 pg/mL and MRD negative (green line, n = 10), ≥1185 pg/mL and MRD positive (blue line, n = 5), Flt3L <1185 pg/mL and MRD negative (black line, n = 30), or <1185 pg/mL and MRD positive (red line, n = 56) (log-rank P value).
Association between Flt3L and post–course 1 remission and survival. Serum Flt3L was measured on day 26 of induction in non-APL AML patients with Flt3 mutation randomized to lestaurtinib (days 11-24) on the UK NCRI AML17 trial. (A) Serum Flt3L at day 26 in patients who subsequently achieved or did not achieve CR. Dotted line indicates optimal cut point identified by the ROC curve: 116 pg/mL (Mann-Whitney UP value). (B) EFS of subgroups with serum Flt3L level ≥291 pg/mL (blue line) or <291 pg/mL (red line). Events include failure to achieve CR and relapse or death from any cause. Threshold of Flt3L for maximum discrimination identified by log-rank testing (log-rank P value). (C) OS of subgroups with a serum Flt3L level ≥1185 pg/mL (blue line) or <1185 pg/mL (red line). Threshold of Flt3L for maximum discrimination identified by log-rank testing (log-rank P value). (D) EFS of subgroups divided according to Flt3L level ≥291 pg/mL and MRD negative (green line, n = 17), ≥291 pg/mL and MRD positive (blue line, n = 15), Flt3L <291 pg/mL and MRD negative (black line, n = 23), or <291 pg/mL and MRD positive (red line, n = 46) (log-rank P value). (E) OS of subgroups divided according to Flt3L level ≥1185 pg/mL and MRD negative (green line, n = 10), ≥1185 pg/mL and MRD positive (blue line, n = 5), Flt3L <1185 pg/mL and MRD negative (black line, n = 30), or <1185 pg/mL and MRD positive (red line, n = 56) (log-rank P value).
This analysis suggested that Flt3L measured at a single point on day 26 had a modest ability to predict CR status after course 1. Consistent with the previous data from cohort A (Figure 2), 4 out of 5 patients with undetectable Flt3L at day 26 were reported as failing to achieve CR. In practice, these patients may be salvaged by the second course of chemotherapy, as also illustrated in Figure 2, so there is not necessarily an association between Flt3L measured during the first course and more distal outcomes such as EFS and OS. In order to test this, a maximally selected log-rank test was used to define cut points for Flt3L in relation to EFS and OS. This determined a significantly greater EFS for patients with Flt3L >291 pg/mL at day 26 (log rank P = .010; Figure 4B) and an OS advantage for patients with Flt3L >1185 pg/mL (log rank P = .0119; Figure 4C). Of 140 patients with an Flt3L measurement, an MRD assessment after course 1 was performed by flow cytometry in 74 by NPM1 RT-qPCR in 56 patients and by both methods in 28 patients. Combining these results, an MRD test by ≥1 methodology was available for 101 patients. Of the 28 patients with both tests, positivity in either test result was scored as positive (see supplemental Table 2 for details). As expected, patients with MRD positive status by either test had a significantly lower chance of EFS and OS (Table 1). We then probed the association between Flt3L and survival, adjusting for MRD status as a covariable in Cox proportional hazard regression models, using the optimal cut points previously determined for EFS and OS to define Flt3L as a categorical variable. Independently of MRD status, the level of Flt3L retained associations with survival that were only just outside 95% confidence intervals (Table 1). The additive effect of MRD and Flt3L was evident from the separation of Kaplan-Meier curves, which showed greater divergence and lower P values than groups defined by either variable alone (Figure 4D-E).
Hazard ratios for survival in 101 patients from AML17 with dual Flt3L measurement and MRD assessment after course 1
| . | HR . | 95% CI . | Test . | P . |
|---|---|---|---|---|
| EFS | ||||
| Flt3L <291 vs ≥291 | 0.51 | 0.31-0.84 | Log rank | .0076 |
| MRD positive vs negative | 0.38 | 0.23-0.61 | Log rank | .0001 |
| Flt3L <291 vs ≥291, adjusting for MRD | 0.57 | 0.32-1.03 | Cox | .0600 |
| OS | ||||
| Flt3L <1185 vs ≥1185 | 0.38 | 0.18-0.79 | Log rank | .0097 |
| MRD positive vs negative | 0.41 | 0.23-0.73 | Log rank | .0025 |
| Flt3L <1185 vs ≥1185, adjusting for MRD | 0.25 | 0.06-1.05 | Cox | .0590 |
| . | HR . | 95% CI . | Test . | P . |
|---|---|---|---|---|
| EFS | ||||
| Flt3L <291 vs ≥291 | 0.51 | 0.31-0.84 | Log rank | .0076 |
| MRD positive vs negative | 0.38 | 0.23-0.61 | Log rank | .0001 |
| Flt3L <291 vs ≥291, adjusting for MRD | 0.57 | 0.32-1.03 | Cox | .0600 |
| OS | ||||
| Flt3L <1185 vs ≥1185 | 0.38 | 0.18-0.79 | Log rank | .0097 |
| MRD positive vs negative | 0.41 | 0.23-0.73 | Log rank | .0025 |
| Flt3L <1185 vs ≥1185, adjusting for MRD | 0.25 | 0.06-1.05 | Cox | .0590 |
HR, hazard ratio; CI, confidence interval.
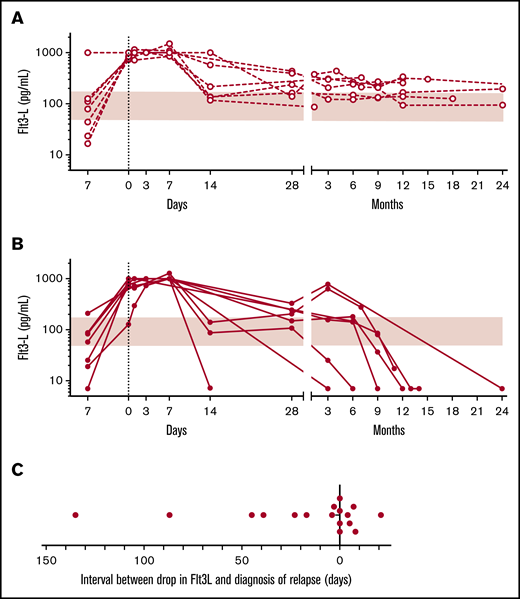
Posttransplant remission assessment using Flt3L
In order to assess the potential utility of Flt3L in identifying patients at risk of relapse following hematopoietic stem cell transplantation, samples were collated from a calendar-driven prospective serum collection from day −7 to 24 months from patients receiving hematopoietic stem cell transplantation in cohort A. From this were identified 8 sequential patients who relapsed and 7 patients in continuing CR over the same period (Figure 5). In all patients, Flt3L increased to a peak of ∼1000 pg/mL during the aplastic phase, immediately following conditioning. Flt3L remained at or above physiological levels in 7 patients with sustained remission (Figure 5A) but declined and became undetectable in 8 patients who relapsed (Figure 5B). Samples were only collected every 3 months, so it was not always possible to observe a decline in Flt3L prior to relapse. However, in 6 out of 17 posttransplant relapses, a drop in Flt3L occurred ≥10 days prior to the diagnosis of relapse.
Serial measurement of Flt3L after hematopoietic stem cell transplantation. (A) Serial serum Flt3L measurements in patients with non-APL AML undergoing hematopoietic stem cell transplantation remaining in continuous remission (n = 8; open circles and broken lines; shaded region indicates normal range). Patients were sampled prior to conditioning (day −7), on the day of transplant (day 0), and on days and months posttransplant, as indicated. Patients were selected over the same period as panel B. (B) Serial serum Flt3L measurements in 7 patients with non-APL AML undergoing hematopoietic stem cell transplantation who relapsed (n = 7; filled circles and broken lines). Consecutive relapsed patients ≤2 years posttransplant are reported. (C) Interval between drop in Flt3L below the normal range and diagnosis of relapse. Summary of calendar-driven Flt3L measurement in 17 patients indicating timing of the point at which Flt3L first went below normal relative to the hematological diagnosis of relapse. Includes all patients in B with 10 additional patients in whom ≥1 Flt3L measurement was recording posttransplantation.
Serial measurement of Flt3L after hematopoietic stem cell transplantation. (A) Serial serum Flt3L measurements in patients with non-APL AML undergoing hematopoietic stem cell transplantation remaining in continuous remission (n = 8; open circles and broken lines; shaded region indicates normal range). Patients were sampled prior to conditioning (day −7), on the day of transplant (day 0), and on days and months posttransplant, as indicated. Patients were selected over the same period as panel B. (B) Serial serum Flt3L measurements in 7 patients with non-APL AML undergoing hematopoietic stem cell transplantation who relapsed (n = 7; filled circles and broken lines). Consecutive relapsed patients ≤2 years posttransplant are reported. (C) Interval between drop in Flt3L below the normal range and diagnosis of relapse. Summary of calendar-driven Flt3L measurement in 17 patients indicating timing of the point at which Flt3L first went below normal relative to the hematological diagnosis of relapse. Includes all patients in B with 10 additional patients in whom ≥1 Flt3L measurement was recording posttransplantation.
Discussion
Flt3L is a critical hematopoietic growth factor that becomes markedly elevated in response to depletion of the hematopoietic stem/progenitor compartment. Here, we show that it is depleted in the overwhelming majority of patients with AML, the exceptions being associated with low expression of the receptor Flt3 (CD135) by blasts, as frequently observed in APL. These results are consistent with a model in which the level of Flt3L is inversely related to the abundance of Flt3+ stem/progenitor cells or AML blasts. Several previous reports have highlighted the expression of Flt3 in AML27,28 and documented that Flt3L may function as an autocrine growth factor29 and possibly attenuate the effect of Flt3 inhibitors during therapy.10
Regulation of Flt3L production is not completely understood. In the steady state, the major source appears to be nonhematopoietic30 but it is also secreted by activated and peripheral blood T cells.17,30 Alternative splicing produces membrane-bound Flt3L that may play a major role in homeostasis but was not studied here.31 Preformed Flt3L has also been described in progenitor cells and AML blasts.32 In mice, Flt3L has been described mainly in the hematopoiesis of dendritic cells,33 but in humans, Flt3 is expressed by CD38low CD45RA+ early progenitor cells, suggesting a more fundamental role in the regulation of lymphomyeloid hematopoiesis.11,34
The potential utility of Flt3L to assist in the assessment of remission between courses of chemotherapy was demonstrated by restoration of Flt3L as patients entering remission, but not in the setting of refractory disease. However, morphological assessment and Flt3L were not always concordant. Five patients thought not to be in CR after course 1 showed elevations of Flt3L that heralded attainment of morphological CR after course 2. In 3 cases, CR was reported but there was no restoration of Flt3L, and early relapse ensued. In the larger cohort of patients taken from the AML17 trial, there was a significantly different distribution of Flt3L in relation to CR status, but a number of patients with low or undetectable Flt3L were reported to be in CR. It is possible that some patients entering CR overshoot the normal range, becoming transiently depressed. An attractive alternative is that measurement of Flt3L will increase the accuracy of assigning CR by morphology alone. Further prospective study will be required to answer this question.
An MRD assessment after course 1 was performed by flow cytometry or NPM1 RT-qPCR in 101 patients on AML17. A caveat of our analysis is that these measurements may not be directly comparable but were combined in the interest of greater statistical power. Remarkably, a single measurement of Flt3L provided similar hazard ratios for EFS and OS as these tests. Furthermore, the combination of MRD status and Flt3L defined subgroups with highly divergent EFS and OS, including 10 out of 101 elite survivors with high Flt3L and undetectable MRD who had 100% survival. The association between Flt3L and survival remained almost significant (P ≤ .06) after adjustment for MRD status in a Cox proportional hazard model, suggesting that Flt3L reports independent prognostic information.
Weekly Flt3L measurement provided a fascinating insight into the dynamics of response to cytoreductive chemotherapy. Patients achieving CR had significantly elevated Flt3L peaking just after the end of therapy and returning to the normal range upon count recovery. Those with refractory disease showed transient elevation of Flt3L followed by rapid depletion. Two patients who were rendered aplastic maintained high levels in the absence of further chemotherapy. Based on these observations, serum ELISA for Flt3L appears to be a low-cost noninvasive method for the serial monitoring of patients during remission induction. In particular, Flt3L is likely to dichotomize patients with delayed count recovery into those with low Flt3L due to residual disease and those with high Flt3L and hypoplasia. Tracking of the Flt3L response may thus potentially reduce the need for serial invasive BM assessments and stratify patients for further therapy.
The development of Flt3L as a prognostic tool is more challenging. We took advantage of AML17 trial data in which a single measurement was performed at day 26. A strong association with attainment of CR was observed in the expected direction, at a cut point of 116 pg/mL. This is approximately the median of the normal range, reinforcing the rationale of Flt3L as a biomarker of progenitor cell mass. A more accurate predictive tool might be developed from serial weekly measurements in which the rate of rise, peak level, or AUC could have higher discriminatory potential. Concerning longer-term survival outcomes, we found discriminatory thresholds for EFS and OS. EFS was inferior in patients with Flt3L <291 pg/mL. Failure to achieve CR was included as an event, so this subgroup includes all patients with refractory disease who did not survive. A subgroup of 20 patients with high Flt3L (>1185 pg/mL) also enjoyed unusually good OS of >80% at 3 years compared with ∼50% in the remainder of the cohort. The reason for this is not immediately apparent. We speculate that very high levels of Flt3L occur in association with deep remissions in chemosensitive disease, but further studies will be required to validate these thresholds and determine their prognostic utility in the context of MRD assessment. We note that all patients were taken from a relatively homogeneous genetic group with either Flt3 ITD or kinase domain mutation. Consequently, we found no evidence to suggest that the elite survivor subgroup group had unusually favorable genetics.
We explored the use of Flt3L measurement to detect relapse in patients after hematopoietic stem cell transplantation. As expected, there was elevation of Flt3L during aplasia and a recovery to normal or supranormal in patients in continuing CR. Using a schedule of sampling every 3 months, it was possible to detect relapse early in a proportion of patients. As with postchemotherapy evaluation, Flt3L may provide useful insights into pancytopenia in the posttransplant patient, distinguishing between poor graft function or myelosuppression and incipient relapse. The temporal resolution of this would clearly be improved by weekly sampling in future studies. Monitoring for progression or relapse is not limited to transplant patients; 2 patients with MDS in whom Flt3L became undetectable as they progressed to AML illustrate that Flt3L could facilitate the timing of surveillance BM testing in this patient group.
Remission assessment after the first course of induction chemotherapy is a key milestone in achieving long-term RFS of AML. Presently, the standard of care is expectant, and remission is formally assessed by examination of the BM following hematopoietic recovery. Patients will not know that they have resistant or refractory disease until several weeks after completing the first course of chemotherapy, a problem that is frequently compounded by delayed blood count recovery in those most at risk of treatment failure.
Treatment refractoriness is difficult to predict from clinical, cytogenetic, and molecular genetic information.3,4 An interim BM assessment at day 15 may discern blast clearance and is routine practice in many North American centers.35 However, this is often a nadir for the patient in terms of cytopenia and attendant systemic illness, and interpretation can be difficult. It is not a universal practice in Europe.7
The data presented here suggest that Flt3L may provide an inexpensive, rapid, and noninvasive means of assessing remission status in AML. As with MRD techniques, it is likely that performance of the test will be specific to the intensity of treatment. For example, a different kinetics of response has previously been reported in the context of lower-intensity treatment with azacitidine and sorafenib.36
Finally, the response of Flt3L to chemotherapy is likely to reflect multiple known risk factors in AML, including genetic subgroup, blast count, and attainment of MRD-negative status. Large prospective studies will be required to evaluate this information in a stratified manner in order to determine whether Flt3L responses are integrative of known risk factors or provide independent prognostic information. Both have the potential to find utility in clinical practice.
Acknowledgments
The authors thank Hyun Yu (Newcastle University) for assistance with sample collection, Robert Hills (Oxford University) for preliminary statistical analysis, and Paresh Vyas (Oxford University) for helpful discussion.
C.W.-B. and S.K. are supported by Cancer Research UK (CRUK) Cardiff Experimental Cancer Medicine Centre core funding and CRUK Clinical Research Committee Clinical Trials Unit Programme Award core funding. P.M. and M.C. are supported by CRUK (C30484/A21025), Histiocytosis UK, the Histiocytosis Association, and Bright Red. The authors also acknowledge support from NIHR Newcastle Biomedical Research Centre at Newcastle upon Tyne Hospitals NHS Foundation Trust.
Authorship
Contribution: P.M. designed the study, acquired, analyzed, and interpreted data, and drafted the manuscript; C.W.-B. analyzed and interpreted data and performed critical revision; M.R.G., S.D.F., K.G. A.P., S.P., H.M., R.D., A.G., and G.L.J. acquired and analyzed data; V.B. acquired, analyzed, and interpreted data; A.M.D. and A.K.B. acquired data; N.H.R. interpreted data and performed critical revision of the manuscript; M.L. conceived and designed the study and interpreted data; S.K. conceived and designed the study, interpreted data, and performed critical revision; and M.C. conceived and designed the study, analyzed and interpreted data, drafted the manuscript, and performed critical revision.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Matthew Collin, Institute of Cellular Medicine, Newcastle University, Framlington Pl, Newcastle upon Tyne NE2 4HH, United Kingdom; e-mail: matthew.collin@ncl.ac.uk.
References
Author notes
S.K. and M.C. contributed equally to this study.
The full-text version of this article contains a data supplement.