Key Points
We describe a novel allo-tumor–reactive and CD8α-dependent Vγ5Vδ1TCR.
The molecular interface with proximity to the peptide-binding groove of HLA-A*24:02 is an essential determinant of recognition.
Abstract
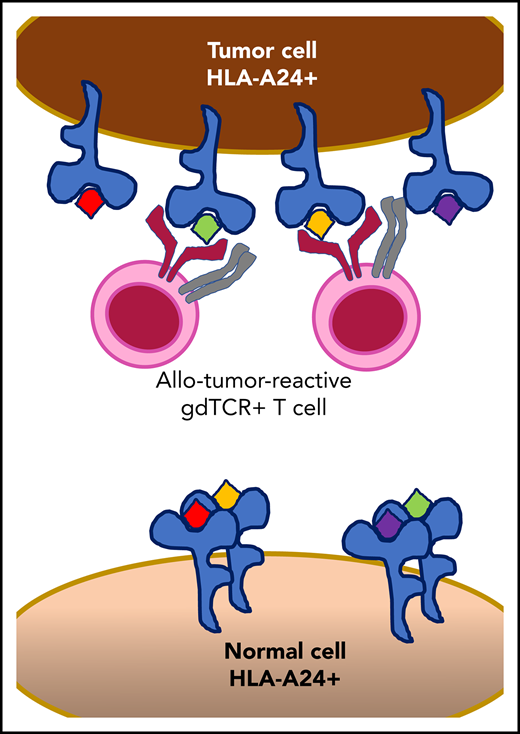
γδT cells are key players in cancer immune surveillance because of their ability to recognize malignant transformed cells, which makes them promising therapeutic tools in the treatment of cancer. However, the biological mechanisms of how γδT-cell receptors (TCRs) interact with their ligands are poorly understood. Within this context, we describe the novel allo-HLA–restricted and CD8α-dependent Vγ5Vδ1TCR. In contrast to the previous assumption of the general allo-HLA reactivity of a minor fraction of γδTCRs, we show that classic anti-HLA–directed, γδTCR-mediated reactivity can selectively act on hematological and solid tumor cells, while not harming healthy tissues in vitro and in vivo. We identified the molecular interface with proximity to the peptide-binding groove of HLA-A*24:02 as the essential determinant for recognition and describe the critical role of CD8 as a coreceptor. We conclude that alloreactive γδT-cell repertoires provide therapeutic opportunities, either within the context of haplotransplantation or as individual γδTCRs for genetic engineering of tumor-reactive T cells.
Introduction
Human immunity is organized by interacting innate and adaptive immune subsystems that elicit a fast and durable response, respectively. γδT cells are situated between the innate and adaptive immune systems, as they share properties of both systems, illustrated by their ability to recognize malignant transformed1 or infected2 cells, to clonally expand, and to form memory.3 Recently, the important biological role of γδT cells in cancer immune surveillance has been further highlighted by the fact that γδT cells infiltrate various tumors.4,5 However, the biological understanding of cancer immune surveillance and potential clinical applicability of γδT cells, or their individual receptors, is substantially hampered by the lack of well-defined γδT-cell receptor (TCR) ligands, as well as their precise molecular requirements for recognition.6 γδT-cell ligands that have been identified so far are mostly associated with metabolic changes in stressed cells. For example, Vγ9Vδ2 T cells, the major subset of γδT cells in the periphery, are activated by cells with an increase in intracellular phosphoantigens caused by a dysregulated mevalonate pathway, related to transformation or infection.7,8 γδT cells that do not express a Vδ2 chain, collectively called Vδ2− γδT cells, are mainly found in tissues and are activated by stress-related ligands, such as EPCR,9 MICA,10 and annexin A2.11 Furthermore, CD1c and CD1d can present self and foreign lipid antigens to Vδ2− γδ cells in a classic αβT cell HLA-like fashion.12 Because ligands of both Vδ2+ and Vδ2− γδT cells are to some extent constitutively expressed on healthy cells, it remains unclear exactly how the balance between self and tumor or infection is orchestrated. Recent data suggest that receptors, such as Vγ9Vδ2TCRs, modulate the delicate line between healthy and diseased tissue by sensing spatial and conformational changes of membrane-expressed CD277, which occurs in transformed cells.8,13 To exploit γδT cells or their receptors as therapeutical tools, the understanding of the localization and structure of the ligands during stress or transformation needs to be understood. Furthermore, identifying new γδTCR ligands restricted to stressed or transformed cells is valuable for developing therapies for unmet medical needs. Within this context, we sought to identify a potential ligand of a Vδ1+ γδT-cell clone that has been classified as reactive against different tumor cell types, as well as to understand the molecular interaction of this receptor with its ligand.2
Materials and methods
Cells lines and flow cytometry
Generation of γδT-cell clone FE11.
Clone FE11 was generated as described in a previous publication.2 Details are provided in supplemental Methods.
Cloning NEF134-144- and WT1126-134-specific αβTCRs.
Retroviral transduction of TCRs.
Details are provided in supplemental Methods and our previous publication.16
Retroviral transduction of HLA.
Phoenix-ampho retroviral packaging cells were transduced with pLZRS-A*02:01-IRES-NGFR or pLZRS-A*24:02-IRES-NGFR and the retroviral packaging plasmids gag-pol (pHIT60) and env (pCOLT-GALV), using Fugene-HD. The HLA plasmids were kindly provided by Marieke Griffioen (Leiden University Medical Centre, Leiden, The Netherlands).
CRISPR/Cas genome editing.
The β2m gene-specific regions of the gRNA sequence (GAGTAGCGCGAGCACAGCTA) was designed by the CRISPR design tool from the Zhang laboratory (http://crispr.mit.edu/). As control gRNA, the eGFP gene was targeted (GGAGCGCACCATCTTCTTCA). The pSicoR-CRISPR-Cas9 vector used was a kind gift from Robert Jan Lebbink (University Medical Center Utrecht, Utrecht, The Netherlands). LCL-TM cells were transduced with the viral supernatants, and knockdown of β2M was confirmed by flow cytometry.
Functional T-cell assays.
Flow cytometry FRET.
To study dimerization of HLA, cells were labeled with Alexa594-conjugated α-HLA-A (donor) and Alexa647-conjugated α-HLA-A (acceptor), respectively. The donor fluorescence was measured with a FACS LSRFortessa flow cytometer (BD) where donor fluorescence of the double-labeled healthy samples was compared with that of the double-labeled malignant samples. Förster resonance energy transfer (FRET) efficiency was calculated from the fractional decrease of the donor fluorescence in the presence of the acceptor, using the equations described by Sebestyén and colleagues.17 Correction factors for the spectral overlap between the different fluorescence channels were obtained from data measured on unlabeled and single-labeled cells.
Animal model
The NOD.Cg-PrkdcscidIl2rgtm1Wjl Tg(HLA-A24)3Dvs/Sz (NSG-A24) mice18 were kindly provided by Leonard D. Shultz (The Jackson Laboratory, Bar Harbor, ME). C57BL/6 mice were purchased from Janvier (Le Genest‐Saint‐Isle, France). All mice were bred and housed in the specific pathogen-free breeding unit of the Central Animal Facility of Utrecht University. Experiments were conducted according to institutional guidelines after acquiring permission from the local ethics committee and in accordance with current Dutch laws on animal experimentation. NSG-A24 mice received sublethal total body irradiation on day −1, followed by IV injection of 0.1 × 106 K562 HLA-A*24:02 luciferase tumor cells on day 0, after which they were treated with 1 × 107 TEG011 cells or mock TCR–transduced T cells on days 1 and 6. IL2 (6 × 105 IU in 100 µL incomplete Freund’s adjuvant) was administered subcutaneously once every 3 weeks.
Statistical analyses
Differences were analyzed in GraphPad Prism 7 for Windows (GraphPad Software Inc., La Jolla, CA), using the indicated statistical tests.
Results
Tumor specificity of the Vγ5Vδ1T-cell clone can be transferred to αβT cells by transfer of the γδTCR only
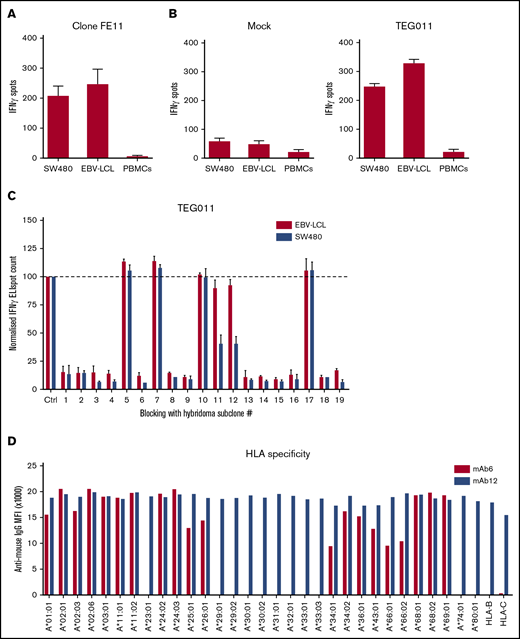
To confirm the tumor reactivity of the recently identified, tumor-specific γδT-cell clone FE11,2 the clone was coincubated with SW480 (colorectal adenocarcinoma) cells, Epstein-Barr virus-transformed lymphoblastoid cell lines (EBV-LCLs), and healthy peripheral blood mononuclear cells (PBMCs), leading to recognition, as measured by interferon (IFN)-γ ELISPOT, of the 2 tumor cells lines, but not the healthy PBMCs (Figure 1A). Next, both the γ and δ chains of γδT-cell clone FE11 were sequenced, identified as a Vγ5Vδ1 TCR, and cloned into the pBullet retroviral vector and subsequently introduced into αβT cells, as previously described.16 Taking the γδTCR out of the innate-like environment enabled us to study the functioning of the receptor without interference of NK receptors, which are not present on αβT cells.19,20 We have recently described this strategy as T cells engineered to express a defined γδT-cell receptor (TEG cells).21,-23 Introduction of FE11 γδTCR in αβT cells (later referred to as TEG011 cells) resulted, as shown by the strong expression of the introduced FE11 γδTCR and a substantial downregulation of the endogenous αβTCR, in many cells becoming single positive for the expression of the introduced γδTCR (supplemental Figure 1). This finding led to a comparable recognition of target cells, when comparing TEG011 to the original clone FE11 (Figure 1B), indicating that tumor reactivity is mediated by the γδTCR and independent of (epi)genetic factors exclusively present in the original T-cell clone.
Introduction of FE11 γδTCR in αβT cells can reestablish tumor cell recognition of clone FE11 cells. (A) To assess tumor reactivity, clone FE11 cells were incubated with SW480 or EBV-LCL tumor target cells. IFN-γ secretion was measured by ELISPOT. Healthy PBMCs served as negative control targets. (B) The TCR-γ and -δ chains of clone FE11 cells were sequenced and retrovirally transduced into αβT cells. Transfer of γδTCR-mediated tumor reactivity was tested by coincubating mock- (left) or γδTCR-transduced (right) T cells with indicated target cells in an IFN-γ ELISPOT. (C) The effect of blocking with FE11-like hybridoma supernatant on the recognition of SW480 and LCL-TM cells by FE11 γδTCR–transduced T cells. (D) LABScreen Single Antigen HLA class I beads were incubated with antibodies purified from hybridoma 6 (mAb6) or from hybridoma 12 (mAb12) and secondary α-mIgG-PE measured using Luminex. Error bars represent the standard deviation (SD; n ≥ 1). MFI, mean fluorescence intensity.
Introduction of FE11 γδTCR in αβT cells can reestablish tumor cell recognition of clone FE11 cells. (A) To assess tumor reactivity, clone FE11 cells were incubated with SW480 or EBV-LCL tumor target cells. IFN-γ secretion was measured by ELISPOT. Healthy PBMCs served as negative control targets. (B) The TCR-γ and -δ chains of clone FE11 cells were sequenced and retrovirally transduced into αβT cells. Transfer of γδTCR-mediated tumor reactivity was tested by coincubating mock- (left) or γδTCR-transduced (right) T cells with indicated target cells in an IFN-γ ELISPOT. (C) The effect of blocking with FE11-like hybridoma supernatant on the recognition of SW480 and LCL-TM cells by FE11 γδTCR–transduced T cells. (D) LABScreen Single Antigen HLA class I beads were incubated with antibodies purified from hybridoma 6 (mAb6) or from hybridoma 12 (mAb12) and secondary α-mIgG-PE measured using Luminex. Error bars represent the standard deviation (SD; n ≥ 1). MFI, mean fluorescence intensity.
Hybridoma-derived antibodies indicate a role for classic HLA molecules
The observation that the FE11 γδTCR by itself recognizes multiple tumor cell lines, but not healthy PBMCs, was highly interesting. We wanted to identify the ligand of the FE11 γδTCR by generating TCR-like antibodies by the immunization of C57BL/6 mice with the complete tumor cell lines SW480 and LCL-TM, which were recognized in vitro by TEG011 cells. From the hybridomas generated, 19 clones were isolated that produced antibodies that specifically bound FE11 γδTCR–reactive tumor cells in an antibody binding screen. To further determine the ligand specificity of the antibodies, the FE11 target SW480 and LCL-TM cells were preincubated with supernatants from these hybridomas and subsequently used in cocultures to stimulate the TEG011 cells. Thirteen of the 19 antibodies (ie, hybridoma supernatants) blocked the activation of the TEG011 cells substantially, as measured by IFN-γ ELISPOT (Figure 1C). These data suggest that most of the raised antibodies partially or completely prevented the binding of the FE11 γδTCR to its ligand. In contrast, none of the 19 hybridomas produced an antibody that blocked the recognition of the WT1126-134 (HLA-A*02:01) peptide–loaded SW480 cells by αβT cells engineered with a WT1126-134-specific αβTCR (supplemental Figure 2A), suggesting that the blocking was not induced via binding to molecules expressed on an αβT cell other than the introduced γδTCR.24 From the 19 hybridomas, 1 antibody that completely blocked activity (clone 6) and 1 that partially blocked activity (clone 12; from here on named mAb6 and mAb12, respectively) were arbitrarily selected for the array of options for antibody production and purification. These purified antibodies were coupled to streptavidin beads and subsequently used for ligand immunoprecipitation in cell lysates of either SW480 or LCL-TM cells. Mass spectrometry analysis resulted in the identification of a panel of mostly classic HLA molecules (supplemental Table 1), suggesting that, in contrast to the general assumption, classic HLA molecules may be involved in recognition of tumor cells by this particular γδTCR. To confirm that raised antibodies are specific for classic HLA, we incubated LABScreen Single Antigen HLA class I beads25 with mAb6 and mAb12 and measured the beads by Luminex to determine HLA specificity. Figure 1D shows that mAb6 had reactivity to a defined subgroup of HLA-A alleles, whereas mAb12 displayed no specificity, reacting to all HLA class I alleles, including HLA-B and -C, present on the LABScreen beads.
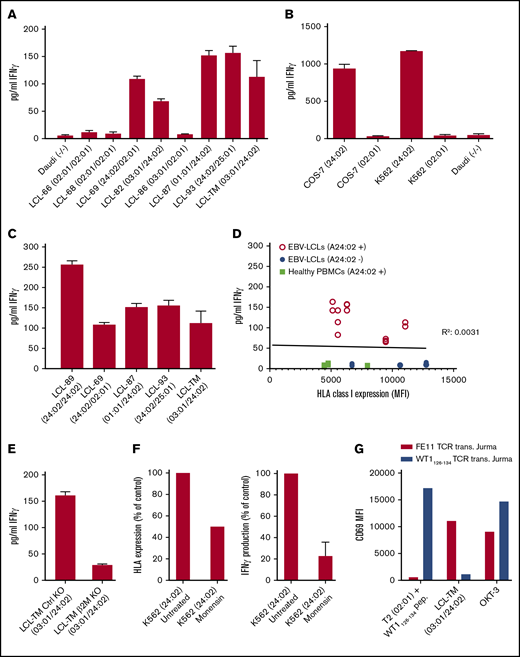
Target cell recognition by the FE11 γδTCR is critically dependent on HLA-A*24:02
The raised antibodies bound to a broad range of different HLA types. To further narrow down the type of HLA recognized by γδTCR-FE11, we made use of the library of cell lines from the Centre d’Etude du Polymorphisme Human (CEPH), which contains a large collection of EBV-transformed B-cell lines (EBV-LCLs) obtained from several family pedigrees with a large variety of HLA haplotypes.26 TEG011 cells were coincubated with 7 different CEPH EBV-LCLs, covering multiple possible HLA molecules, as suggested by the LABScreen beads (Figure 1D), Daudi, and LCL-TM cells, and reactivity was assessed by measuring IFN-γ release. Correlating reactivity of TEG011 cells to the different HLA types from a large panel of LCLs covering many frequent HLA types suggested uniquely that the HLA-A*24:02 haplotype, but not the HLA-A*02:01 or the HLA-A*03:01 haplotype (Figure 2A; supplemental Table 2), was involved in the recognition. To formally confirm HLA-A*24:02-mediated recognition, we retrovirally introduced either HLA-A*24:02 or HLA-A*02:01 (as the control) into the HLA− cell lines COS-7 and K562. In both cell lines, introduction of HLA-A*24:02, but not HLA-A*02:01, resulted in strong activation of TEG011 (Figure 2B). In addition, we found that the density of the ligand HLA-A*24:02 on the target cells was associated with the activity of TEG011 cells, since the reactivity of TEG011 cells was higher against cell lines homozygous for HLA-A*24:02 than against heterozygous cell lines (Figure 2C). Major differences in HLA expression could therefore contribute to the differential recognition between healthy cells and tumor cells. Therefore, HLA class I expression was measured in multiple HLA-A*24:02 heterozygous and negative LCLs and in HLA-A*24:02+ PBMCs. However, no correlation was observed for small variations between the total HLA class I expression and TEG011-cell targeting within these LCLs, indicating that only the expression levels of HLA-A*24:02 are associated with TEG011 cell targeting (Figure 2D). Also, no substantial differences in HLA expression between PBMCs and recognized LCLs have been observed. A partial CRISPR/Cas9 knockout of β2-microglobulin within recognized LCLs, reduced activation of TEG011 (Figure 2E; supplemental Figure 2B), as expected. In addition, a substantial reduction of HLA expression on the cell membrane by monensin, a protein-transport inhibitor, resulted in a decreased recognition of target cells (Figure 2F).
Activation of FE11 γδTCR–transduced T cells is dependent on expression of HLA-A*24:02. (A) Activation of T cells, transduced with FE11 γδTCR by EBV-LCLs with different HLA genotypes. (B) Activation of T cells, transduced with FE11 γδTCR by HLA-A*24:02 or HLA-A*02:01 target cells. (C) Activation of T cells, transduced with FE11 γδTCR by EBV-LCLs with different either homozygous or heterozygous HLA-A*24:02 expression. (D) Total HLA class I expression of HLA-A*24:02-positive and -negative EBV-LCLs compared with TEG011 recognition. (E) The effect of β2m knockout of HLA-A*24:02 target cells on the activation of FE11 γδTCR–transduced T cells. (F) Activation of T cells, transduced with FE11 γδTCR by K562 HLA-A*24:02 cells untreated or overnight monensin incubation. (G) Activation of Jurma cells, transduced with FE11 γδTCR or αβTCR WT1126-134 (control) by LCL-TM or A2-restricted WT1126-134 peptide–loaded T2 cells. CD3 cross-linking by plate-bound α-CD3 mAb clone OKT-3 served as the positive control. Recognition was assessed by measuring IFN-γ secretion using ELISA. Error bars represent the SD (n ≥ 1).
Activation of FE11 γδTCR–transduced T cells is dependent on expression of HLA-A*24:02. (A) Activation of T cells, transduced with FE11 γδTCR by EBV-LCLs with different HLA genotypes. (B) Activation of T cells, transduced with FE11 γδTCR by HLA-A*24:02 or HLA-A*02:01 target cells. (C) Activation of T cells, transduced with FE11 γδTCR by EBV-LCLs with different either homozygous or heterozygous HLA-A*24:02 expression. (D) Total HLA class I expression of HLA-A*24:02-positive and -negative EBV-LCLs compared with TEG011 recognition. (E) The effect of β2m knockout of HLA-A*24:02 target cells on the activation of FE11 γδTCR–transduced T cells. (F) Activation of T cells, transduced with FE11 γδTCR by K562 HLA-A*24:02 cells untreated or overnight monensin incubation. (G) Activation of Jurma cells, transduced with FE11 γδTCR or αβTCR WT1126-134 (control) by LCL-TM or A2-restricted WT1126-134 peptide–loaded T2 cells. CD3 cross-linking by plate-bound α-CD3 mAb clone OKT-3 served as the positive control. Recognition was assessed by measuring IFN-γ secretion using ELISA. Error bars represent the SD (n ≥ 1).
TEG cells have been reported to lose alloreactivity because of the downregulation of the endogenous αβTCR caused by the dominance of the introduced γδTCR.21 However, to formally exclude any activity of endogenous αβTCR within the TEG format, we introduced either FE11 γδTCR or αβTCR-WT1126-134 (as the control) into the TCRβ− Jurma cell line. The transduced Jurma cells were then coincubated with WT1126-134 peptide–loaded T2 or LCL-TM tumor cells, and target-specific activation of Jurma cells was determined by measuring the activation marker CD69 by flow cytometry. As anticipated, FE11 γδTCR-transduced Jurma cells were activated only by the HLA-A*24:02-expressing LCL-TM cells, whereas the αβTCR-WT1126-134-transduced Jurma cells were activated only by WT1126-134-loaded T2 cells (Figure 2G). In conclusion, target cell recognition by the FE11 γδTCR is critically dependent on and restricted to HLA-A*24:02.
FE11 γδTCR selectively recognizes HLA-A*24:02 expressed in malignant but not in healthy cells
Allo-HLA reactivity is a phenomenon that is usually restricted to HLA on all cells of an individual.27 To assess whether recognition is limited to HLA-A*24:02+-transformed cells, we coincubated TEG011 cells with healthy primary T cells that were either positive or negative for HLA-A*24:02. In contrast to HLA-A*24:02+ tumor cells, healthy primary cells were not recognized by TEG011 cells, even when they were positive for HLA-A*24:02. B cells isolated from multiple healthy donors did not activate the TEG011 cells, even after being stressed by irradiation or by combination treatment with cyclophosphamide and fludarabine. Activation of these B cells by administration of either LPS or CD40L and IL-4 also did not lead to recognition by TEG011 cells. These results indicate that the expression of the HLA-A*24:02 allele in combination with a malignant transformation is essential for the activation of TEG011 cells (Figure 3A; supplemental Figure 3A). To further exclude recognition of healthy tissues in the absence or presence of stress or infection in epithelial tissues, HLA-A*24:02+, fibroblasts were cocultured with either TEG011 or T cells transduced with the HLA-A*24:02-restricted NEF134-144 αβTCR.15 TEG011 cells did not recognize the HLA-A*24:02 fibroblasts stressed by either irradiation or administration of cyclophosphamide and fludarabine. In addition, cytomegalovirus (CMV) infection of these fibroblasts did not induce activation of the TEG011 cells, whereas the NEF134-144 αβTCR-transduced T cells recognized the fibroblasts in all conditions (Figure 3B; supplemental Figure 3B). To finally confirm that malignant transformation is essential for recognition by TEG011 cells in an autologous system, HLA-A*24:02+ B cells were immortalized by using EBV transformation and did activate TEG011 cells, whereas the nontransformed PBMCs of the very same donor were not recognized (Figure 3C).
Activation of FE11 γδTCR–transduced T cells is limited to HLA-A*24:0+malignant cells. (A) Activation of TEG011 cells by malignant and healthy hematological cells. B cells from multiple HLA-A*24:02+ donors were activated or stressed before the TEG011 cell coculture. (B) TEG011 or NEF134-144 αβTCR–engineered αβ T-cell recognition after coculture with HLA-A*24:02+ healthy tissues. When using NEF134-144 αβTCR–engineered αβ T cells, 10 μM NEF134-144 was added. (C) Healthy donor B cells (HD1) were EBV transformed and cocultured with TEG011. Recognition was assessed by measuring IFN-γ secretion using ELISA. Error bars represent the SD (n ≥ 2). *P < .05. Cyclo, cyclophosphamide; Fluda, fludarabine.
Activation of FE11 γδTCR–transduced T cells is limited to HLA-A*24:0+malignant cells. (A) Activation of TEG011 cells by malignant and healthy hematological cells. B cells from multiple HLA-A*24:02+ donors were activated or stressed before the TEG011 cell coculture. (B) TEG011 or NEF134-144 αβTCR–engineered αβ T-cell recognition after coculture with HLA-A*24:02+ healthy tissues. When using NEF134-144 αβTCR–engineered αβ T cells, 10 μM NEF134-144 was added. (C) Healthy donor B cells (HD1) were EBV transformed and cocultured with TEG011. Recognition was assessed by measuring IFN-γ secretion using ELISA. Error bars represent the SD (n ≥ 2). *P < .05. Cyclo, cyclophosphamide; Fluda, fludarabine.
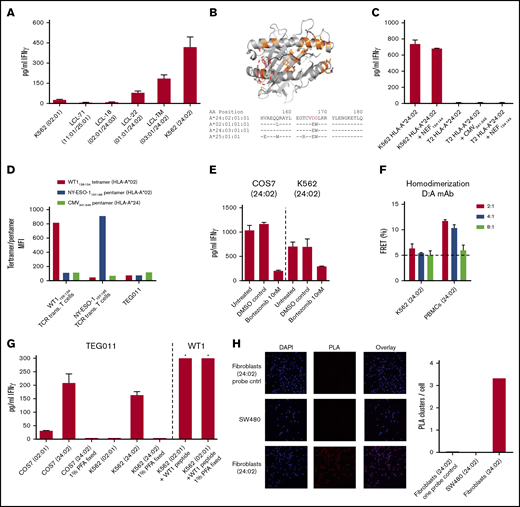
Identification of the putative binding site of the FE11 γδTCR
To further map the putative binding site of FE11, CEPH EBV-LCLs expressing HLA alleles from different supertypes were tested (ie, HLA-A*25:01 from supertype HLA-A01 and HLA-A*02:01 from supertype HLA-A02).28 In addition, CEPH EBV-LCLs expressing an HLA allele within the same supertype as HLA-A*24:02 (supertype HLA-A24; HLA-A*24:03) was tested. Reactivity of TEG011 cells was observed only toward the HLA-A*24:02+ cells, not toward the strong homologous HLA-A*24:03 present on EBV-LCL-71 (Figure 4A). Sequence alignment (Figure 4B, bottom) revealed that the 2 amino acids on the α2 helix at positions 168 and 169 (asparagine and glycine, respectively) are nonhomologous between HLA-A*24:02 and the nonrecognized HLA alleles, indicating that these residues are key for recognition of HLA-A*24:02 by TEG011 cells. Structural analyses of the putative binding sites at positions 168 and 169 indicated they were very close to the peptide binding groove (Figure 4B, top).
Activation of FE11 γδTCR–transduced T cells is dependent on the presence of a specific HLA-A*24:02-restricted peptide. (A) Activation of TEG011 by HLA-A*24:02-positive or -negative target cells. (B) The differences between HLA-A*02:01 and HLA-A*24:02 mapped on the structure of HLA-A*24:02 (Protein Data Bank: 3wl9), the 2 nonhomologous amino acids between HLA-A*24:02 and HLA-A*24:03 are show in the red circle (top). Alignment of HLA-A*24:02, 02:01, 24:03, and 25:01 with the 2 nonhomologous amino acids in red (bottom). (C) Activation of T cells, transduced with γδTCR-FE11, by HLA-A*24:02-transduced, TAP-deficient T2 cells not loaded or loaded with the A*24-restricted viral peptides NEF134-144 or CMV341-349 (pp65 341-349). (D) WT1126-134 tetramer, NY-ESO1157-165 pentamer, and CMV341-349 pentamer binding to WT1126-134-specific TCR, NY-ESO1157-165-specific TCR, and FE11 TCR–transduced T cells. (E) The effect of bortezomib treatment of HLA-A*24:02–transduced target cells COS-7 (left) and K562 (right) on the activation of FE11 γδTCR–transduced T cells. (F) Homodimerization was assessed on HLA-A*24:02+ cells, recognized and not recognized by flow cytometry FRET. (G) Activation of TEGs (left) or T cells transduced with the WT1126-134-specific αβTCR (control) (right), by HLA-A*24:02-transduced COS-7 and K562 cells or HLA-A*02:01 (control). *Out of range. (H) Proximity Ligation Assay (PLA) was performed on HLA-A*24:02+ fibroblasts and the SW480 cell line. Cells were stained for 4′,6-diamidino-2-phenylindole and PLA signal. Where indicated, target cells were fixed before coincubation; target cells were coincubated with WT1126-134. Error bars represent the SD (n ≥ 1).
Activation of FE11 γδTCR–transduced T cells is dependent on the presence of a specific HLA-A*24:02-restricted peptide. (A) Activation of TEG011 by HLA-A*24:02-positive or -negative target cells. (B) The differences between HLA-A*02:01 and HLA-A*24:02 mapped on the structure of HLA-A*24:02 (Protein Data Bank: 3wl9), the 2 nonhomologous amino acids between HLA-A*24:02 and HLA-A*24:03 are show in the red circle (top). Alignment of HLA-A*24:02, 02:01, 24:03, and 25:01 with the 2 nonhomologous amino acids in red (bottom). (C) Activation of T cells, transduced with γδTCR-FE11, by HLA-A*24:02-transduced, TAP-deficient T2 cells not loaded or loaded with the A*24-restricted viral peptides NEF134-144 or CMV341-349 (pp65 341-349). (D) WT1126-134 tetramer, NY-ESO1157-165 pentamer, and CMV341-349 pentamer binding to WT1126-134-specific TCR, NY-ESO1157-165-specific TCR, and FE11 TCR–transduced T cells. (E) The effect of bortezomib treatment of HLA-A*24:02–transduced target cells COS-7 (left) and K562 (right) on the activation of FE11 γδTCR–transduced T cells. (F) Homodimerization was assessed on HLA-A*24:02+ cells, recognized and not recognized by flow cytometry FRET. (G) Activation of TEGs (left) or T cells transduced with the WT1126-134-specific αβTCR (control) (right), by HLA-A*24:02-transduced COS-7 and K562 cells or HLA-A*02:01 (control). *Out of range. (H) Proximity Ligation Assay (PLA) was performed on HLA-A*24:02+ fibroblasts and the SW480 cell line. Cells were stained for 4′,6-diamidino-2-phenylindole and PLA signal. Where indicated, target cells were fixed before coincubation; target cells were coincubated with WT1126-134. Error bars represent the SD (n ≥ 1).
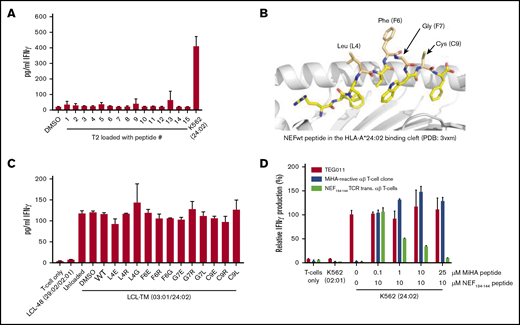
Promiscuous peptides are necessary for HLA-A*24:02 recognition by γδTCR-FE11
Because of the proximity of the putative binding site to the peptide binding groove, we explored the role of a peptide in the recognition of HLA-A*24:02 by γδTCR FE11. The cell line T2, which is deficient in TAP-dependent endogenous peptide processing and presentation in HLA molecules, was transduced with HLA-A*24:02 and HLA-A*02:01 (control) and loaded with HLA-A*24:02-restricted NEF134-144 and HLA-A*02:01-restricted WT1126-134 peptides, respectively. To confirm the successful loading of HLA molecules with peptides, stabilization of HLA on the surface of T2 cells was assessed by flow cytometry (supplemental Figure 4A). HLA-A*24:02-transduced T2 cells externally loaded with NEF134-144 or CMV341-349 did not lead to activation of TEG011, indicating that the presence of HLA-A*24:02 alone is not sufficient when expressed on T2 cells, but that the presentation of an endogenously processed peptide could be key to establishing reactivity (Figure 4C). To confirm this hypothesis, we co-incubated TEG011 with a CMV341-349 HLA-A*24:02–restricted pentamer. Whereas the controls, WT1126-134 and NY-ESO1157-165 αβTCR–transduced T cells with their respective tetramer or pentamer stained positive (Figure 4D), TEG011 cells were not stained by the HLA-A*24:02 pentamer. These data suggest that the observed recognition is not caused by classic alloreactivity and most likely involves either promiscuous peptides to stabilize the complex or a specific peptide as a critical determinant for recognition.
To further assess whether endogenously processed peptides are essential for reactivity, we interfered with the cellular peptide-processing machinery by inhibiting the proteasome of recognized tumor cells by pretreatment with bortezomib.29 Bortezomib treatment led to a strong decrease in recognition of both HLA-A*24:02-transduced COS-7 and K562 cells (Figure 4E) by TEG011 cells, suggesting that peptides are at least needed for stabilization of the complex. To explore whether transformation-associated peptides are involved in recognition, we selected 15 transformation-associated peptides30-35 to load HLA-A*24:02-transduced T2 cells (supplemental Figure 4B; supplemental Table 2) and assessed the recognition by TEG011 cells. None of the 15 peptides led to activation of TEG011 cells (Figure 5A). In contrast, we outcompeted the putative endogenous peptide recognized by TEG011 cells with NEF134-144 wild-type (WT) peptide and NEF134-144 mutants. NEF134-144 mutants were designed by changing the 4 amino acids that face out of the HLA-binding groove (Figure 5B). The 4 amino acids were substituted for the negatively charged amino acid glutamic acid (E), the positively charged amino acid arginine (R), and the smallest amino acid glycine (G). At least part of these modified peptides could be loaded onto the LCL-TM cells (supplemental Figure 5). Next, WT NEF134-144 peptide and all different NEF134-144 mutants were loaded on LCL-TM cells after which they were coincubated with TEG011 cells, followed by measurement of IFN-γ. None of the peptides were able to decrease the recognition, indicating that the recognition mechanism is more elaborate than a standard αβTCR peptide-HLA interaction (Figure 5C) implying that recognition is not mediated by a specific peptide, but rather that promiscuous peptides are involved as stabilizers of the complex. To assure that peptide loading truly outcompetes HLA-A*24:02-bound peptides, HLA-A*24:02-transduced K562 cells were first loaded with WT NEF134-144 peptide and were subsequently loaded with different concentrations of an HLA-A*24:02-restricted minor histocompatibility antigen (MiHA) peptide (K.F., unpublished data). Peptide-loaded cells were then coincubated with TEG011 cells, αβT cells engineered with an HLA-A*24:02-restricted NEF134-144-specific, or a T-cell clone expressing a defined HLA-A*24:02-restricted, MiHA-specific αβTCR. With increasing concentrations of MiHA peptides, αβT cell–engineered NEF134-144-specific TCRs showed reduced cytokine release, whereas TEG011 cell activity was not effective against the very same target (Figure 5D).
Recognition of LCL-TM cells cannot be outcompeted by peptides. (A) T2 cells were transduced with HLA-A*24:02 and loaded with 10 µM of 15 different transformation-associated peptides (supplemental Table 1), after which they were coincubated with TEG011 cells. Activation of TEG011 cells was assessed by measuring IFN-γ production. (B) The 4 residues of NEF134-144 that are pointed out of the peptide binding groove of HLA-A*24:02 are indicated. (C) Ten micromoles of the generated NEF134-144-derived mutant peptides were loaded on LCL-TM cells, after which they were coincubated with TEG011 cells. (D) HLA-A*24:02-transduced K562 cells were loaded with 10 µM NEF134-144 before loading with increasing concentrations of an HLA-A*24:02-restricted MiHA peptide (K.F., unpublished data). The peptide-loaded loaded cells were coincubated with TEG011 cells, αβT cells engineered with an HLA-A*24:02-restricted NEF134-144-specific TCR or a MiHA-specific αβT cell clone. T-cell activation was assessed by measuring IFN-γ. Error bars represent the SD (n ≥ 2).
Recognition of LCL-TM cells cannot be outcompeted by peptides. (A) T2 cells were transduced with HLA-A*24:02 and loaded with 10 µM of 15 different transformation-associated peptides (supplemental Table 1), after which they were coincubated with TEG011 cells. Activation of TEG011 cells was assessed by measuring IFN-γ production. (B) The 4 residues of NEF134-144 that are pointed out of the peptide binding groove of HLA-A*24:02 are indicated. (C) Ten micromoles of the generated NEF134-144-derived mutant peptides were loaded on LCL-TM cells, after which they were coincubated with TEG011 cells. (D) HLA-A*24:02-transduced K562 cells were loaded with 10 µM NEF134-144 before loading with increasing concentrations of an HLA-A*24:02-restricted MiHA peptide (K.F., unpublished data). The peptide-loaded loaded cells were coincubated with TEG011 cells, αβT cells engineered with an HLA-A*24:02-restricted NEF134-144-specific TCR or a MiHA-specific αβT cell clone. T-cell activation was assessed by measuring IFN-γ. Error bars represent the SD (n ≥ 2).
Conformational change as an additional distinguishing factor for recognition
The hypothesis that promiscuous peptides are involved as stabilizers of the complex was supported by the observations that HLA-A*24:02 was also recognized within the context of another species (monkey, COS-7 cell line). In addition, as small amounts of endogenously processed and presented peptides are usually sensed by TCRs, doubling the amount of HLA in a homozygous target, as compared with a heterozygous one, should not substantially affect recognition. However, increased amounts of HLA in homozygous individuals nearly doubled functional activity of the TEG011 cells, suggesting that the HLA-complex rather than the individual peptide-HLA combination was recognized. Therefore, we hypothesized that an additional key spatial or structural conformational change in HLA-A*24:02 occurs as a result of transformation of a healthy cell into a tumor cell. To elaborate on this hypothesis, we used FRET-based flow cytometry, as described before,17 to determine if HLA-A*24:02 clusters in the membrane of tumor cells. In line with this assumption, FRET analysis suggested different behavior of HLA in tumor and healthy tissues with HLA-A*24:02 homodimers on PBMCs and monomers on tumor cells (Figure 4F). To formally test whether membrane mobility of HLA-A*24:02 is key for recognition by γδTCR-HLA but not αβTCR-HLA, we assessed the effect of paraformaldehyde fixation on the sensing of target cells. Whereas the recognition of αβTCR WT1126-134–transduced T cells and WT1126-134 peptide–loaded target cells was not affected by fixation, the interaction of TEG011 cells and HLA-A*24:02-transduced target cells was completely abolished, indicating that there are different requirements for TCR activation (Figure 4G). Altered HLA clustering on tumor cells, as compared with healthy cells, was also supported by a proximity ligation assay of HLA class I molecules that showed reduced HLA clustering in SW480 cells compared with HLA-A*24:02 fibroblasts (Figure 4H). In summary, our data support the notion that malignant transformation of cells leads to alterations in HLA clustering on the cell surface, which may be an additional factor sensed by TEG011 cells.
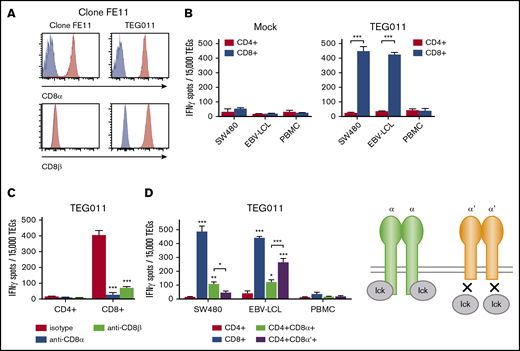
FE11 γδTCR critically depends on the CD8 coreceptor for tumor recognition
To further support the idea that indeed the γδTCR-HLA interaction differs from classic HLA–αβTCR interactions, we investigated the potential role of coreceptors. One obvious candidate, related to HLA class I restriction, was CD8αα. First, we formally confirmed CD8 expression on the original clone, in line with previous reports (Scheper et al2 and Figure 6A). Next, we assessed whether TEG011 is dependent on the coexpression of CD8, similar to the original clone, by sorting TEG011 cells according to CD4 and CD8 expression before coculturing them with SW480 cells, LCL-TM cells, or PBMCs (Figure 6B). In contrast to the γδT-cell clone FE11, most αβT cells expressed CD8 as a heterodimer of CD8α and CD8β for providing costimulation. The role of the CD8αβ heterodimer on TEG011 cells was assessed by using blocking antibodies for either the CD8α or CD8β chain. Not only CD8α-, but also CD8β-blocking antibodies completely inhibited recognition of SW480 cells (Figure 6C), indicating that either CD8αα or CD8αβ is essential for recognition. For costimulation of HLA class I–restricted αβTCRs, CD8αβ can play 2 different roles: it serves as an adhesion molecule that stabilizes the TCR-HLA interaction, and it can play an activating role by signaling via LCK.36 On the other hand, CD8αα on αβT cells has been described as a corepressor rather than a coreceptor by competing with CD8αβ for the LCK signaling molecule.37 To investigate the role of CD8αα for TEG011, we used a truncated variant of CD8α that is signaling deficient because of its inability to bind LCK.38 After introducing both FE11 γδTCR and truncated CD8α (CD8α′) in CD4+ αβT cells, we cocultured the TEG cells with SW480 cells. A decrease in the number of IFN-γ spots of the CD8α′ variant compared with the CD8α WT variant was observed (Figure 6D), indicating that CD8αα indeed plays a costimulatory role in TEG011 cells.
The FE11 γδTCR critically depends on the CD8 coreceptor for tumor recognition. (A) CD8α or CD8β expression on clone FE11 cells and FE11 γδTCR–transduced αβ T cells. (B) CD4+ and CD8+ αβT cells transduced with the FE11 γδTCR were sorted and cocultured with mock (left) and TEG011 (right) target cells. (C) TEG011 T-cell activation was assessed by IFN-γ ELISPOT. CD4+ and CD8+ αβT cells expressing the FE11 γδTCR were coincubated with SW480 target cells as in panel B, but in the presence of a control antibody or blocking antibodies against CD8α or CD8β. (D) αβT cells were transduced with WT CD8α or a truncated, signaling-deficient CD8α variant (CD8α′), alongside the γδTCR-FE11, after which the CD4+, CD8+, CD4+CD8α+, and CD4+CD8α′+ T-cell populations were sorted. Recognition of healthy PBMCs and SW480 tumor target cells was assessed by measuring IFN-γ secretion using ELISPOT. Error bars represent the standard error of the mean (n ≥ 1). *P < .05; **P < .01; ***P < .001.
The FE11 γδTCR critically depends on the CD8 coreceptor for tumor recognition. (A) CD8α or CD8β expression on clone FE11 cells and FE11 γδTCR–transduced αβ T cells. (B) CD4+ and CD8+ αβT cells transduced with the FE11 γδTCR were sorted and cocultured with mock (left) and TEG011 (right) target cells. (C) TEG011 T-cell activation was assessed by IFN-γ ELISPOT. CD4+ and CD8+ αβT cells expressing the FE11 γδTCR were coincubated with SW480 target cells as in panel B, but in the presence of a control antibody or blocking antibodies against CD8α or CD8β. (D) αβT cells were transduced with WT CD8α or a truncated, signaling-deficient CD8α variant (CD8α′), alongside the γδTCR-FE11, after which the CD4+, CD8+, CD4+CD8α+, and CD4+CD8α′+ T-cell populations were sorted. Recognition of healthy PBMCs and SW480 tumor target cells was assessed by measuring IFN-γ secretion using ELISPOT. Error bars represent the standard error of the mean (n ≥ 1). *P < .05; **P < .01; ***P < .001.
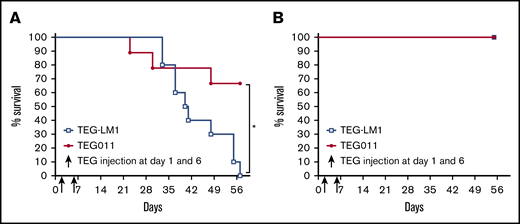
Improved overall survival of TEG011 cells
To determine the safety and efficacy of TEG011 cells in vivo, we set up a humanized HLA-A*24:02 transgenic NSG mouse model for adoptive transfer of TEG011 cells. The irradiated mice were injected with luciferase labeled HLA-A*24:02-transduced K562, and either TEG011 or LM1 transduced T cells as the control. Mice were taken out of the study when the human end point was reached. Overall survival significantly increased, as observed in the TEG011-treated group, when compared with mice treated with LM1-transduced T cells (Figure 7A). TEG011-treated mice also had a significantly lower tumor burden when assessed by bioluminescent imaging (supplemental Figure 6). Importantly, surviving TEG011-treated, tumor-bearing mice showed no further signs of discomfort. Pathology in 3 selected tumor-bearing mice treated with TEG011 cells showed no histological features of toxicity of TEG011 cells, altogether indicating that HLA-A*24:02+ tumor cells but not healthy cells were targeted by TEG011 cells. Lack of toxicity of TEG011 cells in vivo in an HLA-A*24:02 host was further substantiated by injecting non-tumor–bearing mice with TEG011- and LM1-engineered, transduced T cells in humanized HLA-A*24:02 transgenic NSG mice, which without showing any signs of discomfort (Figure 7B).
TEG011 treatment leads to efficient tumor control of K562-HLA*A24 tumors, whereas it shows no toxicity in vivo in NSG-A24 transgenic mice. NOD.Cg-Prkdc Il2rg Tg(HLA-A24)3Dvs/Sz (NSG-A24) mice were injected with 1 × 105 K562 HLA-A*24:02 Luciferase cells on day 0 followed by 1 × 107 TEG011 or LM1 transduced T cells on days 1 and 6 (n = 10 per group). In parallel, non-tumor–bearing mice also received 1 × 107 TEG011 or LM1 transduced T cells on days 1 and 6 (n = 5 per group). Overall survival of treated K562-HLA*A24 luciferase tumor-bearing mice for monitoring efficacy (A) and overall survival of non-tumor–bearing mice for monitoring toxicity (B) was recorded for 57 days. Data represent the mean ± SD of all mice in each group. Statistical significance was calculated by log-rank (Mantel-Cox) test; *P < .05.
TEG011 treatment leads to efficient tumor control of K562-HLA*A24 tumors, whereas it shows no toxicity in vivo in NSG-A24 transgenic mice. NOD.Cg-Prkdc Il2rg Tg(HLA-A24)3Dvs/Sz (NSG-A24) mice were injected with 1 × 105 K562 HLA-A*24:02 Luciferase cells on day 0 followed by 1 × 107 TEG011 or LM1 transduced T cells on days 1 and 6 (n = 10 per group). In parallel, non-tumor–bearing mice also received 1 × 107 TEG011 or LM1 transduced T cells on days 1 and 6 (n = 5 per group). Overall survival of treated K562-HLA*A24 luciferase tumor-bearing mice for monitoring efficacy (A) and overall survival of non-tumor–bearing mice for monitoring toxicity (B) was recorded for 57 days. Data represent the mean ± SD of all mice in each group. Statistical significance was calculated by log-rank (Mantel-Cox) test; *P < .05.
Discussion
The major finding of the study is that we identified an alloreactive γδTCR, which can distinguish between healthy and tumor tissues. Furthermore, we elucidated the molecular interface of the investigated Vγ5Vδ1TCR clone FE11 and provided evidence that, although the binding site is close to the peptide-binding groove of HLA-A*24:02, transformation-associated HLA peptides do not distinguish between healthy and cancerous tissues. Most likely, other key conformational changes within the membrane selectively occurring in HLA on tumor cells but not on healthy tissues in vitro and in vivo, are responsible for the differential recognition between tumor and healthy cells.
Allo-HLA type of recognition by γδTCRs has been suggested for HLA-A*02,39 HLA-A*24,40 and HLA-B*27.41 These data suggest that our observation reflects a broader phenomenon that may be linked to unique γδTCR sequences, as we could not find the sequence used for TEG011 in many other HLA-A*24:02-positive and -negative donors (n = 7 HLA-A*24:02, total n = 23; data not shown). The underlying molecular mechanism has not been defined so far, in contrast to alloreactivity of αβTCRs.42,-44 Considering this, a γδTCR selectively recognizing tumor cells in an allo-HLA context seems to be plausible; however, our data suggest that the mode of action differs between alloreactive αβTCRs. We characterized the essential contact residues of FE11 γδTCR with HLA-A*24:02, which appeared to be in proximity to the peptide-binding groove. Our data suggest that the FE11 γδTCR recognizes amino acids 168 and 169 on the α2-helix of HLA-A*24:02, given that these are the only nonhomologous amino acids between recognized HLA-A*24:02 and non-recognized HLA-A*24:03.45 Differences in recognition of the same peptide presented by HLA-A*24:02 and HLA-A*24:03 by CD8+ αβT cells has been observed before.46 Thus, not only αβTCRs, KIRs, LILRs, and CD8 molecules,47 but also γδTCRs can bind to a specific part of HLA class I. However, our data also imply that, in contrast to recognition of HLA by an allopeptide-reactive αβTCR, promiscuous peptides are involved in mediating recognition by γδTCR FE11. This assumption would also be an explanation for the activity of TEG011 against a very broad range of tumor cells, even though it is a rare TCR sequence in humans.
Our HLA membrane topology data suggest that, instead of a defined tumor-derived peptide, another key spatial or conformational change, such as differences in clustering of HLA-A*24:02-molecules between tumor cells and healthy cells, plays a role in mediating tumor specificity. HLA clustering has mainly been studied within the context of HLA class II on antigen-presenting cells, which does not necessarily depend on the presence of a T cell.48 Clustering of HLA has been reported to be essential for the recognition of HLA-B*27 recognition through leukocyte immunoglobulinlike receptors B2 and killer cell immunoglobulinlike receptors 3DL2.49,50 HLA behavior on tumor cells has mainly been studied within the context of tumor immune escape by loss or downregulation of HLA class I expression.51 The preferential monomeric form of HLA at the cell membrane of tumor cells suggested herein could be part of classic tumor escape mechanisms for αβT cells, which can be sensed by the described alloreactive γδTCR.
A major concern for using the alloreactive FE11 γδTCR in a therapeutic scenario would be that, because of the nature of promiscuous peptides as part of the recognition complex, safety is difficult to assess. To partially address this concern, we performed tumor control experiments in HLA-A*24:02 transgenic mice. In histological analyses, we did not observe pathological evidence for autoimmunity in the investigated organs. Our observation is also supported by the clinical observation that αβT-cell–depleted haplotransplantations associate with very good tumor control and limited toxicity.52,-54 Though in therapeutic scenarios, the administration of TEG is more feasible because generating high numbers of TEGs for patients is superior over using expanded alloreactive γδT-cell clones, the new wave of haplotransplantations55 most likely benefits from a better understanding of allotumor-reactive γδT-cell immune repertories, as described here. This knowledge would allow, for example, the development of cellular vaccines expressing tumor-HLA to boost allotumor reactive γδT cell clones in vivo.
In summary, we report on the very interesting nature of alloreactivity of a γδTCR which is able to distinguish between healthy and malignant cells. This observation extends the use of γδTCR for the TEG concept as next-generation CAR-T cells as it opens an avenue to a completely new set of tumor targets seeing conformational and spatial changes at the cell membrane.8 ,56 ,57 This observation emphasizes that γδT cells, within the context of haplotransplantation, not only possess classic antitumor reactivity but also benefit from allotumor reactivity.20 In addition, such γδTCR, within the context of TCR gene therapies, can be an interesting addition to tumors expressing HLA-A*24:02.
The full-text version of this article contains a data supplement.
Acknowledgments
This work was supported by Grants ZonMW 43400003 and VIDI-ZonMW 917.11.337, KWF Grants UU 2013-6426, UU 2014-6790, UU 2015-7601, and Gadeta (J.K.); Grant UU2017-11393 (Z.S. and J.K.); Marie Curie Grant 749010 (D.X.B.); National Institutes of Health, National Institute of Allergy and Infectious Diseases Grant R01AI29543 (M.N.); and National Cancer Institute Grant CA34196 (L.D.S.). A.J.R.H., D.V.-D., and M.A. received funding through Proteins@Work, a program of the Roadmap Facilities of The Netherlands (project number 184.032.201).
Authorship
Contribution: G.J.J.K., W.S., A.D.M., I.J., A.J., M.S., T.A.-R., D.X.B., L.K., T.S., S.H., J.H.W.L., E.S.J., A.d.B., D.V.-D., M.A., A.J.R.H., Z.S., and J.K. designed and analyzed the experiments; G.J.J.K., W.S., A.D.M., I.J., M.S., T.A.-R., D.X.B., L.K., E.S.J., D.V.D., and Z.S. performed the experiments; K.F., M.G., J.H.F., L.B., L.D.S., F.I., and M.I.N. contributed vital components; G.J.J.K., Z.S., J.K. and A.D.M. wrote the manuscript; and all authors agreed on the final manuscript.
Conflict-of-interest disclosure: G.J.J.K., D.X.B., Z.S., and J.K. are inventors on different patents with γδTCR sequences, recognition mechanisms, and isolation strategies. G.J.J.K. is employed by Kiadis Pharma. J.K. is scientific advisor and shareholder of Gadeta. The remaining authors declare no competing financial interests.
Correspondence: J. Kuball, UMC Utrecht, Lundlaan 6, 3584 EA Utrecht, The Netherlands; e-mail: j.h.e.kuball@umcutrecht.nl.
References
Author notes
G.J.J., W.S., A.D.M., and I.J. contributed equally to this work.
Z.S. and J.K. are joint senior authors.