Background
Each year, >230 000 children with sickle cell disease (SCD) are born in sub-Saharan Africa compared with 2600 in North America and 1300 in Europe. Yet, the natural history of SCD in sub-Saharan Africa remains largely unknown.
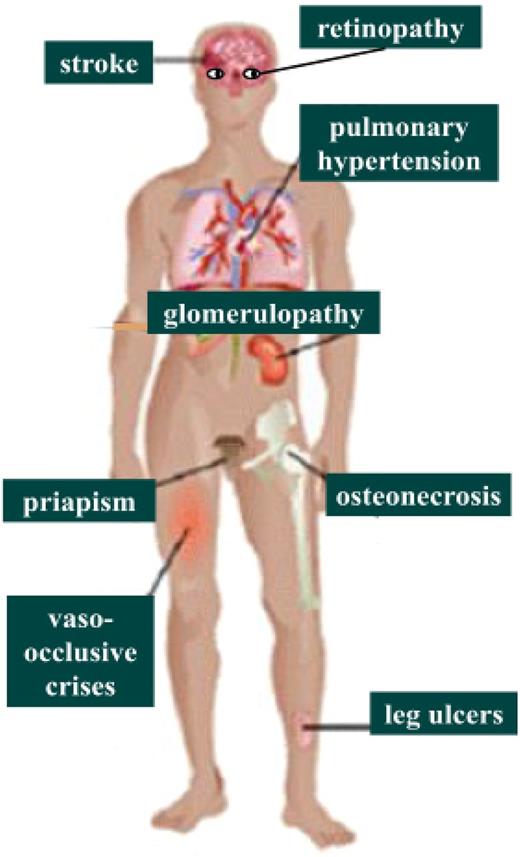
SCD associates episodes of acute illness (acute vaso-occlusive events) and progressive multiorgan damages, which encompass many macro- or microvascular events, such as stroke, heart failure, pulmonary hypertension, kidney disease, bone infarcts, leg ulcers, priapism, etc.
The high interindividual variability of SCD clinical manifestations is notorious, including in patients with similar genotypes. The reasons for this variability are poorly understood, although clearly both genetic and environmental factors are involved.
Although the sub-Saharan African population is the most afflicted by SCD in the world, most clinical studies concerning SCD chronic complications involve patients from developed countries, where the socioeconomic, environmental and medical contexts are dramatically different.
Objectives of the CADRE study
To build up the first multinational cohort of patients with SCD in West and Central Africa.
To assess the prevalence and incidence of the main SCD-related chronic vascular complications in Africa.
To look for clinical, biological, and functional risk factors of SCD-related vascular complications and death that can be used in the African setting to ameliorate the long-term monitoring of patients.
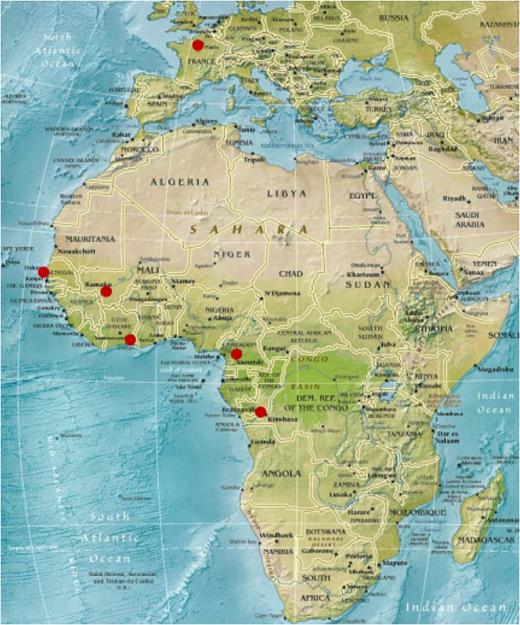
Consortium (Figure 1)
Methodological coordination in Paris, France (UMR 970, INSERM, Université Paris Descartes).
Local investigator team, including 1 hematologist, 1 pediatrician, and 1 cardiologist by center in:
Yaoundé, Cameroon,
Dakar, Senegal,
Bamako, Mali,
Abidjan, Ivory Coast, and
Libreville, Gabon, replaced by Kinshasa, Democratic Republic of Congo, in 2016.
Funding by the French National Institute for Medical Research (INSERM) and the Sorbonne Paris Cité University.
Patients and methods
Recruitment in hematology and pediatric centers in the capital cities of Cameroon, Mali, Senegal, Ivory Coast, and Gabon (replaced by Democratic Republic of Congo in 2016).
Inclusion criteria
SCD patients ≥3 years old (SCD confirmed by hemoglobin electrophoresis and high-performance liquid chromatography) investigated at a steady state (no recent vaso-occlusive crisis, infection or transfusion) plus age- and country-matched controls (1 control for 4 patients).
Monitoring of clinical, biological and functional data every 5 years.
Studied complications (Figure 2):
clinically defined: priapism, leg ulcers, stroke, osteonecrosis (confirmed by radio), retinopathy,
biologically defined: nephropathy (serum creatinine: eGFR, urine albumin:creatinine ratio), and
echocardiography: tricuspid regurgitation jet velocity >2.5 m/s (screening for pulmonary hypertension).
State of progress
Initial recruitment from February 2011 to October 2013.
4300 SCD patients with different phenotypes and 950 healthy controls in 5 African countries.
Inclusion data have been reported in different publications (see frame above).
Second (5-year) visits pending since June 2016.
Scientific strengths
CADRE is the first large-scale and multinational prospective African cohort of SCD patients.
Different subpopulations of SCD patients are studied, both in terms of hemoglobin phenotype and ethnicity. This will help to evidence the genetic contribution in clinical variability.
A multidisciplinary approach has been chosen, mixing epidemiologists, hematologists, pediatricians, cardiologists, and ophthalmologists and using clinical, functional, and biological data collection.
Among all potential vasculopathy predictors, simple physiological and biological techniques that are feasible in Africa have been favored to ensure good interoperator reproducibility for the study, as well as to allow for future use by African physicians.
The very large size of the cohort allows the study of various endophenotypes at an epidemiological scale and therefore lead powerful statistical analyses.
The cohort includes healthy controls from the same ethnicity and environment, allowing the determination of African normal ranges for our study parameters and limiting genetic and environmental bias.
Research capacity building
Strengthening of the international collaboration in the field of SCD in Africa
Reinforcing of the North-South research cooperation with bilateral exchanges regarding the methodology and the implementation of the study.
Reinforcing of the South-South research cooperation with creation of the first operative multinational research network in West and Central Africa.
Facilitation of the unification of clinical practices in the participating centers by mutual agreement on the data to be recorded and the definition of every item in the database.
Initiation of a culture of clinical research in the participating centers
New organization of the nurses’ and doctors’ schedules to allow clinical research.
Education of clinical practitioners to reach the standards and quality requirements of a prospective study.
Systematic collection of clinical and biological data, using a standardized clinical form.
Collaboration with diverse local specialists interested in the field of SCD (hematologists, pediatricians, ophthalmologists, cardiologists, geneticists, etc.).
Training of 1 local research assistant in each center to help the clinical team.
Regular local meetings with the local principal investigator to inform and motivate the clinical team.
Close monitoring by the Internet as well as regular visits on site from the Paris coordinating team to ensure the maintenance of high-quality data collection.
Scientific training of 2 young African investigators in France (Master’s and PhD level).
Facilitation of and training for high-quality research reporting
Supervision of medical theses and specialty essays: at least 2 by centers.
Submission of posters and oral communications presented by the local investigators in national, French, and international meetings.
Redaction of original articles submitted in international journals.
Conclusions
The CADRE study is the first project that has been able to build a large and multinational cohort of patients with SCD in Africa. It has allowed a strong reinforcing of both North-South and South-South cooperation regarding training and clinical research in this field, between France and 5 African countries, as well as among these African countries.
Authorship
Conflict-of-interest disclosure: No competing financial interests declared.
Correspondence: Saliou Diop; e-mail: saliou2_diop@hotmail.com.