Key Points
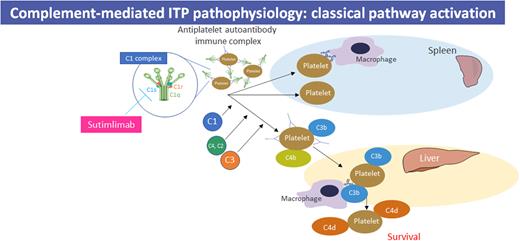
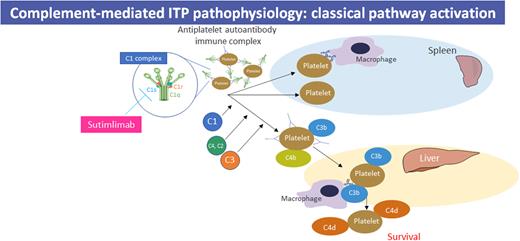
Classical complement pathway activation contributes to the pathophysiology and clinical heterogeneity of immune thrombocytopenia (ITP).
Sutimlimab rapidly and durably increased platelet count in patients with chronic ITP by selectively blocking C1s in the classical pathway.
Abstract
Chronic/refractory immune thrombocytopenia (ITP) is a rare and pathophysiologically heterogeneous disorder with variable responsiveness to available treatments. Sutimlimab, a first-in-class humanized monoclonal anti-C1s IgG4 antibody, selectively inhibits the classical pathway. This phase 1 study (NCT03275454) assessed the safety, efficacy, pharmacokinetics, and pharmacodynamics of biweekly sutimlimab in patients with chronic/refractory ITP with an inadequate response to ≥2 therapies (platelet count ≤ 30 × 109/L). Twelve patients (median age 42 years) received sutimlimab for a median of 20.5 weeks followed by a median 2-week washout period (part A). In part B, 7 of the 12 eligible patients received sutimlimab retreatment for a median of 113 weeks. In part A, the mean (standard deviation) platelet count increased from 25 × 109/L (17) to 54 × 109/L (60) 24 hours after starting sutimlimab, maintaining ≥50 × 109/L throughout part A. Five patients (42%) achieved durable platelet count responses (≥50 × 109/L in ≥50% of follow-up visits) and 4 achieved complete response (platelet count ≥100 × 109/L). The mean platelet count returned to baseline during washout and increased upon retreatment in part B. The mean platelet count improvements accompanied the rapid inhibition of the classical pathway. There were 74 treatment-emergent adverse events in part A (n = 10) and 70 in part B (n = 6). Five serious adverse events were observed; 1 event (migraine) was assessed by the investigator as related to sutimlimab. These results demonstrated that in some patients with ITP, autoantibodies activate the classical complement pathway, accelerating platelet destruction or impairing platelet production and contributing to treatment failure. Thus, C1s inhibition may be a safe and beneficial therapeutic approach for patients with chronic/refractory ITP.
Introduction
Immune thrombocytopenia (ITP) is a rare autoimmune disease with an estimated prevalence of 23.6 cases per 100 000 individuals in the United States1 and is characterized by increased platelet destruction and/or impaired platelet production.2,3 ITP is associated with a high risk of bleeding, a mortality rate of up to 14%, a high economic burden, and a reduced quality of life for patients due to fatigue, cognitive impairment, fear of bleeding, and a negative impact on social and work activities.3,4 The goal of current therapies for patients with chronic ITP (≥12 months) is to prevent and resolve bleeding and to improve quality of life. Multiple pathways may contribute to thrombocytopenia in primary ITP (∼80% of cases), including pathogenic antiplatelet immunoglobulin G (IgG) autoantibodies that target surface antigens (eg, glycoproteins αIIbβ3 [GPIIbIIIA] and GPIb-IX-V), T-cell-mediated cytotoxicity, and impaired megakaryocyte function.5,6 Despite therapeutic options targeting several of these mechanisms, a subset of patients (6%-20%) remains unresponsive to treatment and at high risk of morbidity and mortality.7-9 This unresponsiveness suggests that further unidentified mechanisms may be implicated in the pathogenesis of ITP.
One such mechanism that may contribute to the disease refractoriness is antigen-antibody complex-mediated activation of the complement system, a cascade of proteins mediating both innate and adaptive immunity.10 Specific IgG-antigen complexes are capable of activating the C1 complex, ultimately culminating in the generation of C3a and C3b via the classical pathway. C3b deposition on platelets may trigger phagocytosis by macrophages, mostly in the liver and, to a lesser extent, the spleen.11 Preclinical and clinical evidence supports the role of classical pathway activation in ITP. Approximately 50% of patients with ITP have autoantibodies that activate complement or have complement proteins detectable on the platelet surface.12 Disease severity has been demonstrated to correlate with both the deposition of complement on the platelet surface and low C4 levels.13,14 Platelet destruction has been observed to be mediated by complement, and low C3 levels have been shown to be linked to reduced platelet count.14 It has been hypothesized, and demonstrated in a case report,11 that anticomplement therapies such as a C1 esterase inhibitor may increase platelet count in patients with ITP, especially those with severe or refractory disease.14
Sutimlimab (formerly BIVV009) is a first-in-class, humanized monoclonal IgG4 antibody designed to selectively inhibit C1s and prevent classical complement pathway activation. Both single and multiple infusions of sutimlimab were well tolerated in healthy volunteers.15 In the published results of both CARDINAL and CADENZA, sutimlimab was reported to rapidly halt hemolysis, increase hemoglobin levels, and reduce fatigue in patients with cold agglutinin disease.16
Here, we present the results of a phase 1 study designed to assess the safety and efficacy of sutimlimab in patients with chronic ITP.
Methods
Study design
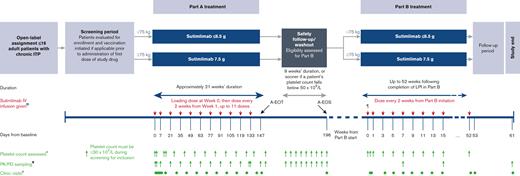
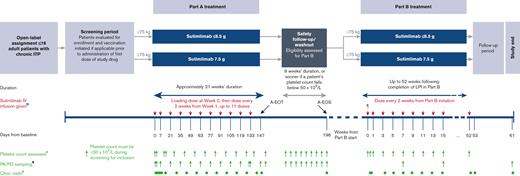
A phase 1, open-label, single-arm, multicenter, 2-part study (NCT03275454) was designed to assess the safety, tolerability, efficacy, pharmacokinetics (PK), and pharmacodynamics (PD) of multiple doses of sutimlimab in adult patients with chronic ITP. This study was sponsored by Bioverativ USA Inc, a Sanofi company. The study was divided into 2 parts (Figure 1). Part A comprised an initial 11-dose treatment period (up to 21 weeks) followed by a safety follow-up/washout period (up to 9 weeks). Part B was an extension period during which eligible patients received sutimlimab until the last patient enrolled in part B had received at least 52 additional weeks of treatment.
Study design. ∗Platelet counts were assessed in part A on days 0 (4 and 8 hours after the first dose), 4, 11, 14, 28, 42, 56, 70, 84, 98, 112, 126, 134, 140, and 154; weekly throughout the washout period; and in part B at 4 and 8 hours after the first dose, on day 4, and then every 2 weeks before each sutimlimab dose. Additional platelet monitoring was performed as needed for safety monitoring or at the discretion of the investigator. If the patient’s platelet count exceeded 450 × 109/L, their next dose of sutimlimab was withheld and dosing resumed when the platelet count was <150 × 109/L. Dosing of concomitant ITP medications could be reduced at any time in patients with elevated platelet counts. ¶Patients entering part B received an additional loading dose if >17 days had elapsed since the last dose received in part A. ¤Dosing may be delayed due to high platelet levels; an additional loading dose was considered if resumption of sutimlimab treatment occurred more than 17 days after the last dose. ¥Blood samples for PK and PD analysis were taken before every sutimlimab dose and at 0.5, 1, 4, 8, and 24 hours after the first and last dose in part A. Blood was sampled weekly during washout, every 4 doses during part B, and 9 weeks after dose completion (last sample not shown on diagram). øDuring part A, clinic visits with full assessments occurred on days 0, 1, 4, 7, 11, 14 and then every 2 weeks through to the end-of-treatment visit (day 147; week 21) and the end-of-washout visit (day 196). During part B, clinic visits were on days 0 and 4 and every 2 weeks thereafter, with end-of-treatment and end-of-study visits occurring 1 week and a maximum of 9 weeks after dose completion, respectively. A-EOS, part A end of study; A-EOT, part A end of treatment; ITP, immune thrombocytopenia; IV, intravenous; LPI, last patient in; PD, pharmacodynamic; PK, pharmacokinetic.
Study design. ∗Platelet counts were assessed in part A on days 0 (4 and 8 hours after the first dose), 4, 11, 14, 28, 42, 56, 70, 84, 98, 112, 126, 134, 140, and 154; weekly throughout the washout period; and in part B at 4 and 8 hours after the first dose, on day 4, and then every 2 weeks before each sutimlimab dose. Additional platelet monitoring was performed as needed for safety monitoring or at the discretion of the investigator. If the patient’s platelet count exceeded 450 × 109/L, their next dose of sutimlimab was withheld and dosing resumed when the platelet count was <150 × 109/L. Dosing of concomitant ITP medications could be reduced at any time in patients with elevated platelet counts. ¶Patients entering part B received an additional loading dose if >17 days had elapsed since the last dose received in part A. ¤Dosing may be delayed due to high platelet levels; an additional loading dose was considered if resumption of sutimlimab treatment occurred more than 17 days after the last dose. ¥Blood samples for PK and PD analysis were taken before every sutimlimab dose and at 0.5, 1, 4, 8, and 24 hours after the first and last dose in part A. Blood was sampled weekly during washout, every 4 doses during part B, and 9 weeks after dose completion (last sample not shown on diagram). øDuring part A, clinic visits with full assessments occurred on days 0, 1, 4, 7, 11, 14 and then every 2 weeks through to the end-of-treatment visit (day 147; week 21) and the end-of-washout visit (day 196). During part B, clinic visits were on days 0 and 4 and every 2 weeks thereafter, with end-of-treatment and end-of-study visits occurring 1 week and a maximum of 9 weeks after dose completion, respectively. A-EOS, part A end of study; A-EOT, part A end of treatment; ITP, immune thrombocytopenia; IV, intravenous; LPI, last patient in; PD, pharmacodynamic; PK, pharmacokinetic.
The study protocol and amendments were prepared according to the Declaration of Helsinki and International Council on Harmonisation guidelines for Good Clinical Practice and were approved by local/central independent ethics/medicine regulatory committees. All participants provided written, informed consent before enrollment in the study. Data were analyzed by Jennifer Wang, and all authors had access to the primary clinical data.
Study eligibility criteria
Adult patients aged ≥18 years with a confirmed diagnosis of chronic ITP (per the definition of ITP diagnosis by the International Working Group [IWG]17) were eligible for study entry. Other inclusion criteria included a platelet count of ≤30 × 109/L during screening, lack of an adequate platelet response (defined as maintenance of sustained platelet count ≥30 × 109/L in the absence of bleeding) to at least 2 prior therapies, a hemoglobin level of >10 g/dL, normal white blood cell and neutrophil counts, and no prior history of a coagulation disorder. Concurrent ITP medications (corticosteroids, IV immunoglobulin [IVIg], azathioprine, danazol, cyclosporin A, mycophenolate mofetil, or thrombopoietin receptor agonists [TPO-RAs]) were permitted, provided the patient had been on a stable dose for ≥1 month. If previously treated with rituximab, ≥12 weeks had to have elapsed between the last dose of rituximab and the first dose of sutimlimab.
Patients were eligible to continue into part B if they met all of the following criteria: had received ≥1 dose of sutimlimab in part A and had evidence of treatment efficacy (defined as a platelet count >30 × 109/L on ≥1 occasion or a doubling of the platelet count from baseline) in part A. In addition, patients were also eligible to enroll in part B if they had completed the part A treatment period and had evidence of ongoing or recurrent thrombocytopenia during the part A safety follow-up/washout period (defined as a platelet count <50 × 109/L or a ≥50% decrease in platelet count over a period of <1 week). Patients were excluded if they reported severe hypersensitivity or anaphylaxis due to sutimlimab. A detailed list of study inclusion and exclusion criteria is provided in supplemental Table 1.
Interventions
All patients received fixed biweekly doses of sutimlimab (6.5 g if <75 kg, 7.5 g if ≥75 kg) administered by intravenous infusion. Initial versions of the protocol permitted the use of a 5.5 g dose. The timing of doses given and assessments are shown in Figure 1. Patients who needed rescue ITP therapy were required to discontinue from the study. Rescue therapies included platelet infusion or IVIg, high-dose corticosteroids, or anti-D immunoglobulin infusion, which were used by the investigator with the intention to increase platelet count or prevent bleeding due to low platelet count.
Outcome measures
Safety outcomes
The primary objective of this study was to evaluate the safety and tolerability of multiple doses of sutimlimab. The primary end point included the incidences of serious and nonserious treatment-emergent adverse events (TEAEs), premature study terminations, and clinical laboratory abnormalities of special interest (systemic lupus erythematosus [SLE] panel) during both part A and part B. Bleeding episodes in part A were assessed via review of TEAEs. In part B, active surveillance for bleeding was conducted according to the IWG Bleeding Assessment Tool.18
Efficacy outcomes
The efficacy objective was to evaluate the platelet response to sutimlimab by measuring the change in blood platelet count from baseline during and at the end of treatment (EOT) in parts A (EOT-A) and B (EOT-B). Additional efficacy end points related to the blood platelet response were the number of patients who achieved a complete response, response, durable response, and stable response to EOT-A, and time to first response; these outcomes are defined in supplemental Table 2.
PK and PD outcomes
PK end points included plasma concentrations of sutimlimab and positivity to antidrug antibodies (ADA) against sutimlimab. ADA levels were assessed using a validated electrochemiluminescence immunoassay with antisutimlimab antibodies. The PD end points included changes in classical complement pathway activity (measured using the Wieslab assay), total C4 levels, and C1q levels over the study period.
Statistical analysis
No formal sample size calculation or statistical hypothesis testing was performed. All outcomes were analyzed using descriptive statistics. In general, continuous variables were summarized using mean, standard deviation (SD), median, and range. Categorical variables were summarized using counts and percentages per category. The baseline platelet count was defined as the average of all nonmissing values obtained during the screening visit and day 0 before the first sutimlimab administration in part A and part B, respectively.
The study was initially designed to evaluate 10 subjects who were administered a fixed dose of 5.5 g of sutimlimab. After the initial recruitment of 6 subjects at this dose level, PK/PD analysis supported a weight-based approach to dose selection, as described previously. The sponsor amended the protocol to allow the recruitment of up to 16 subjects.
Results
Patient disposition
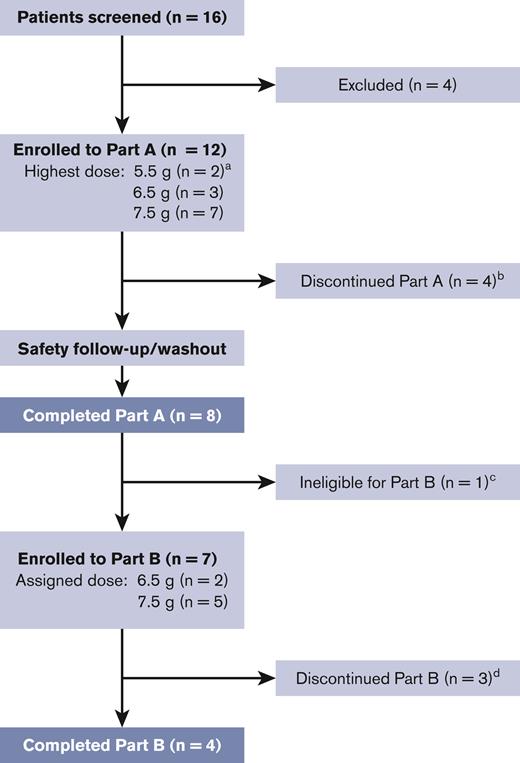
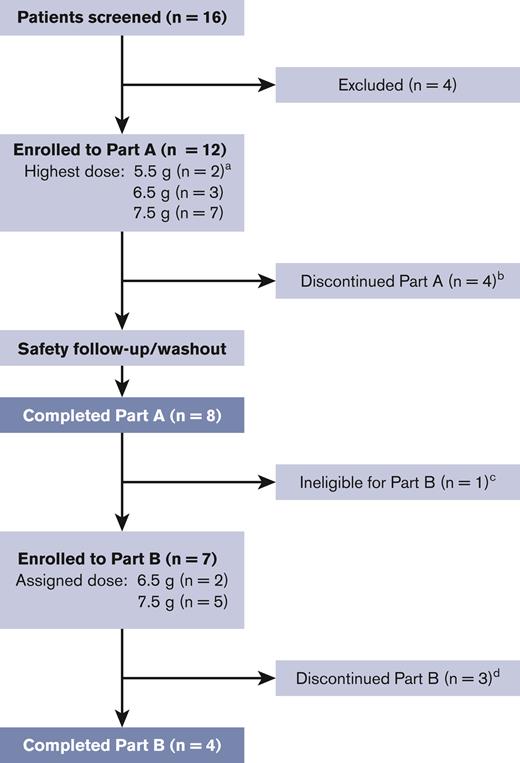
Of the 16 screened patients, 12 were enrolled in part A and received ≥1 dose of sutimlimab (Figure 2). Four patients discontinued the study during part A based on the investigator’s decision of unresponsiveness and/or the need for rescue therapy. The treatment duration in part A ranged from 2 weeks to 23 weeks, and the washout period was up to 7 weeks. Of the 8 patients who completed part A, 7 met the eligibility criteria for continuing treatment and were enrolled in part B. Three patients discontinued from the study during part B, 2 based on the investigator’s decision of unresponsiveness, and 1 withdrew by the subject’s decision. The median treatment duration in part B was 113 weeks.
Patient disposition.aTwo patients received a maximum dose of 5.5 g sutimlimab in accordance with versions 1 and 2 of the protocol and completed part A only; 1 patient received doses of 5.5 g and 6.5 g, and 2 patients received doses of 5.5 g and 7.5 g. bFour patients discontinued part A due to reasons unrelated to sutimlimab; 3 discontinued due to the need for rescue therapy or unresponsiveness as per the investigator’s decision, and 1 discontinued due to reasons unknown. cOnly patients with evidence of treatment efficacy in part A were eligible for part B. One durable responder from part A did not enroll in part B because part B was not included in the study protocol at that time. dThree patients discontinued due to reasons unrelated to sutimlimab: 2 discontinued due to the need for rescue therapy or unresponsiveness as per the investigator’s decision, and 1 patient chose to withdraw (the participant required rescue therapy for severe thrombocytopenia and then withdrew consent at the early terminated visit).
Patient disposition.aTwo patients received a maximum dose of 5.5 g sutimlimab in accordance with versions 1 and 2 of the protocol and completed part A only; 1 patient received doses of 5.5 g and 6.5 g, and 2 patients received doses of 5.5 g and 7.5 g. bFour patients discontinued part A due to reasons unrelated to sutimlimab; 3 discontinued due to the need for rescue therapy or unresponsiveness as per the investigator’s decision, and 1 discontinued due to reasons unknown. cOnly patients with evidence of treatment efficacy in part A were eligible for part B. One durable responder from part A did not enroll in part B because part B was not included in the study protocol at that time. dThree patients discontinued due to reasons unrelated to sutimlimab: 2 discontinued due to the need for rescue therapy or unresponsiveness as per the investigator’s decision, and 1 patient chose to withdraw (the participant required rescue therapy for severe thrombocytopenia and then withdrew consent at the early terminated visit).
Baseline demographic and patient characteristics
Patients were enrolled in 3 global centers (9 patients in the United States, 2 patients in the United Kingdom, and 1 patient in Germany). The median (range) age of the enrolled patients was 42 (27-66) years and 75% were female (Table 1). The baseline disease characteristics and prior ITP-related treatment were indicative of chronic ITP. Median (range) disease duration and baseline platelet count were 4.7 (2.0-36.4) years and 19 (1-57) × 109/L, respectively. All patients had received ITP treatment before (median [range] number of treatments 5.5 [2-10]). The most common treatments were rituximab (83%), TPO-RA (83%), corticosteroids (67%), and IVIg (58%). Nine patients had an inadequate response to TPO-RA and 8 to rituximab. Four patients had undergone splenectomy.
Safety outcomes
During part A, 74 TEAEs were reported in 10 patients (83%). The most frequently reported TEAE was fatigue (n = 3). No serious TEAEs of infection or meningococcal infection were reported. No bleeding episodes were reported as a TEAE. Twenty-one TEAEs in 6 patients were assessed as sutimlimab-related by the investigator (Table 2). Four serious TEAEs were experienced by 3 patients (supplemental Table 3).
During part B, 70 TEAEs were reported in 6 patients (86%). Of these, 10 events in 3 patients were assessed as sutimlimab-related by the investigator (Table 2). One serious TEAE of infection (diverticulitis) was reported but not considered related to sutimlimab treatment (supplemental Table 3). No patient was diagnosed with SLE during the study.
None of the patients discontinued the study treatment because of TEAE. No deaths or thromboembolic events were reported during the study. One patient developed thrombocytopenia during the washout period and received TPO-RA treatment. Two days after receiving the TPO-RA, the patient restarted treatment with sutimlimab without concomitant TPO-RA. This patient experienced thrombocytosis (platelet count >450 × 109/L) 1 week after receiving the TPO-RA and 5 days after receiving sutimlimab. Thrombocytosis was assessed by the investigator as related to sutimlimab treatment, the dosing of which was interrupted per protocol. The patient resumed sutimlimab treatment without concomitant TPO-RA when his/her platelet count fell below 150 × 109/L and there was no further occurrence of thrombocytosis.
Efficacy outcomes
Platelet count responses (part A)
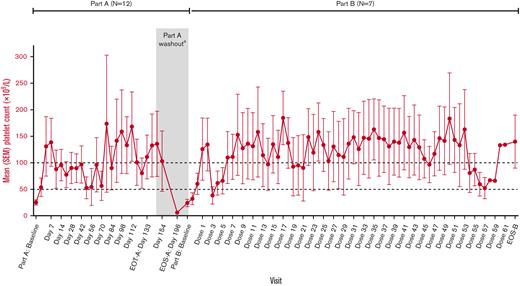
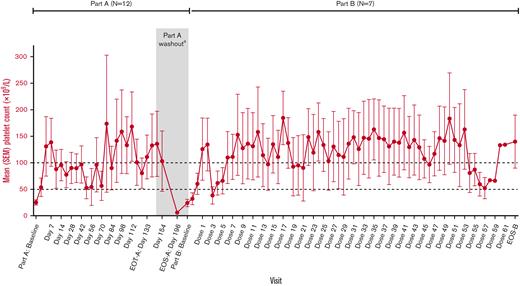
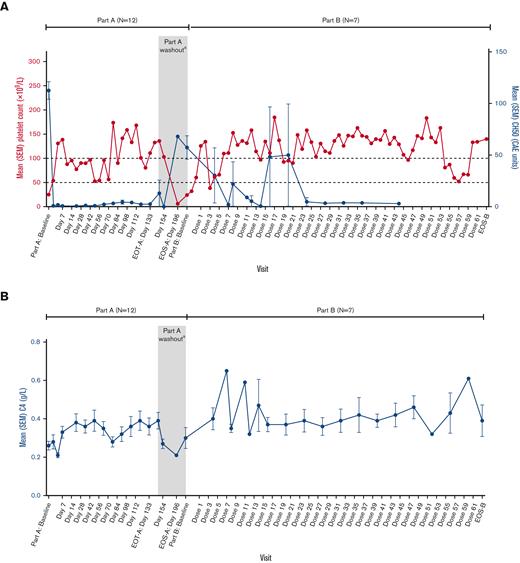
The mean platelet count increased to 54 × 109/L by 24 hours after the first dose of sutimlimab and was sustained above 50 × 109/L throughout part A (Figure 3; Table 3). Four patients (33%) had a platelet count of ≥30 × 109/L and a greater than twofold increase from baseline after 24 hours. Of these patients, 2 (17%) had a platelet count of ≥100 × 109/L after 24 hours. The median (interquartile range) time to the first platelet count response (as defined by a platelet count ≥50 × 109/L with a greater than twofold increase from baseline on 2 consecutive visits at least 1 week apart and without ITP rescue therapy before, on, or between these 2 visits) after the first dose of sutimlimab was 22 (15-36) days. After the sutimlimab washout period, platelet count returned to the pretreatment level in all patients (mean [range], 24 [5-57] × 109/L) (Figure 3; Table 3).
Mean platelet count from baseline to end-of-study treatment with sutimlimab. The value at part A baseline is the average of all platelet counts during the screening period, including day 0 before dosing. The value at part B baseline is the average of all platelet counts during the screening period in part B. N numbers at each point vary according to data availability. In part A, data were available for 5 to 12 patients at each time point, except as follows: n = 4 on days 70, 84, and 154 and n = 1 on day 196. In part B, data were available for 5 to 7 patients at each time point, except as follows: n = 4 for doses 15 to 49, 51, and 53; n = 3 for doses 52, 54, and 55; n = 2 for doses 56 and 57; and n = 1 for doses 58 to 61. OS, end of study; EOT, end of treatment; SEM, standard error of the mean. aFor patients enrolled in protocol version 3 or higher, the washout period starts on day 147 and ends on day 196.
Mean platelet count from baseline to end-of-study treatment with sutimlimab. The value at part A baseline is the average of all platelet counts during the screening period, including day 0 before dosing. The value at part B baseline is the average of all platelet counts during the screening period in part B. N numbers at each point vary according to data availability. In part A, data were available for 5 to 12 patients at each time point, except as follows: n = 4 on days 70, 84, and 154 and n = 1 on day 196. In part B, data were available for 5 to 7 patients at each time point, except as follows: n = 4 for doses 15 to 49, 51, and 53; n = 3 for doses 52, 54, and 55; n = 2 for doses 56 and 57; and n = 1 for doses 58 to 61. OS, end of study; EOT, end of treatment; SEM, standard error of the mean. aFor patients enrolled in protocol version 3 or higher, the washout period starts on day 147 and ends on day 196.
Responder analysis (part A)
Five of the 12 patients (42%) achieved a platelet count response; in all 5 cases, the response was durable (maintained for ≥50% of visits) and was stable in 4 (maintained for ≥70% of visits). In 4 of the 5 durable responders, the platelet count response was complete (≥100 × 109/L on 2 consecutive occasions, ≥7 days apart) (supplemental Figure 1). All durable responders (n = 5) had previously failed TPO-RA and rituximab. One durable responder had also been splenectomized. Median (range) disease duration at screening for durable responders was 6.9 (2.4-21.3) years and for all other patients was 4.7 (2.0-36.3) years.
At baseline, 8 patients were receiving at least 1 concomitant ITP therapy, most frequently TPO-RA (n = 8), IVIg (n = 2), or prednisone (n = 2). After the second dose of sutimlimab, all responders discontinued concomitant therapy and continued treatment with sutimlimab alone (monotherapy). At entry into part A of the study, 4 of the 5 responders were on concomitant ITP medication with an inadequate platelet response (each was on TPO-RA; 1 subject additionally was on IVIg and another was also on corticosteroids). Additional individual details of clinical characteristics, concomitant medications, and platelet values for responders and nonresponders are detailed in supplemental Table 3.
In addition to the patients with objective platelet count response, 3 patients who did not fulfill the response criteria were considered by the investigators to have had meaningful clinical responses and were eligible for part B based on (a) fulfilling the eligibility criteria for part B, (b) having a clinically meaningful and sustained increase in platelet count compared with baseline, and (c) the absence of bleeding or need for rescue therapy or concomitant ITP medication. The baseline and peak platelet counts (parts A and B) of individual patients are provided in supplemental Table 3.
Platelet count responses (part B)
After restarting the sutimlimab treatment, the mean platelet count increased rapidly (Figure 3; Table 3). This improvement in the mean platelet count was observed in the absence of concomitant ITP therapy. Patients achieved their previous level of response to treatment, with mean platelet counts generally sustained above 50 × 109/L and often above 100 × 109/L until EOT-B (Figure 3).
PK outcomes
One patient tested positive for ADA before receiving sutimlimab. This patient had a similar PK profile to other patients in the study. Upon receiving sutimlimab, no patient had treatment-boosted or treatment-induced ADA.
The plasma concentrations of sutimlimab increased rapidly after dose. The mean (SD) plasma concentration at 0.5 hours after dose on day 0 was 2309 (37) μg/mL (6.5 g dose) and 2298 (406) μg/mL (7.5 g dose). The mean (SD) plasma concentration at 0.5 hours after dose on day 133 (EOT-A) was 2979 (670) μg/mL (6.5 g dose) and 3420 (1135) μg/mL (7.5 g dose).
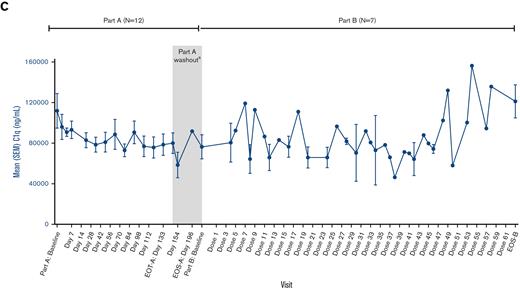
PD outcomes
Sutimlimab treatment rapidly inhibited mean classical complement pathway activity as measured with the Wieslab Complement Classical Pathway assay, which was coincident with the effects of sutimlimab on mean platelet count (Figure 4). The classical complement pathway activity rapidly increased during sutimlimab washout and then decreased again after restarting sutimlimab in part B (Figure 4). The changes in the total C4 levels were consistent with this pattern of complement pathway inhibition. C1q levels remained unchanged (Figure 4).
Discussion
This study demonstrated that sutimlimab administration was associated with a rapid increase in the mean platelet count that was sustained for the duration of treatment in 42% (5/12) of the patients treated. Although the enrolled patients lacked an adequate response (defined as maintenance of a sustained platelet count ≥30 × 109/L in the absence of bleeding) to previous treatment, 75% (8/12) experienced clinically meaningful responses to sutimlimab and maintained platelet counts above 50 × 109/L without concomitant ITP therapy. Overall, sutimlimab was well tolerated, and none of the patients discontinued the study owing to TEAE. One patient experienced thrombocytosis after receiving 1 dose of TPO-RA during an interruption of sutimlimab a day before resuming sutimlimab treatment, which resolved rapidly by pausing sutimlimab treatment.
The selectivity of sutimlimab for classical complement pathway inhibition leaves the alternative and lectin complement pathways intact and able to perform their normal functions in the host defense. The occurrence of infections was consistent with the patient population, medical history, and concomitant medications. Inhibition of C1q may increase the risk of developing symptoms consistent with autoimmune diseases, such as SLE.15,19 However, no changes in C1q levels were observed in this study. In addition, there were no reports of SLE and no clear trend in SLE laboratory parameters.
The subset of ITP that remains unresponsive to treatment suggests there are pathophysiological mechanisms not yet targeted by approved therapies that contribute to thrombocytopenia in these patients. Here, it was demonstrated that treatment with sutimlimab effectively inhibited Weislab-CP activity and CH50, with a decrease from baseline sustained through the treatment period and return to baseline following treatment discontinuation. The complement system has been proven to contribute to immune regulation and tissue damage in a variety of autoimmune disorders.20 It is also known to be involved in immune cytopenias such as autoimmune hemolytic anemia.21 However, limited information is available regarding the possible contribution of the complement system in ITP pathophysiology. In a recent retrospective study of over 100 patients with ITP, one-third had substantial reductions in C3 and C4 and/or total complement compared with healthy individuals, consistent with increased classical complement pathway activity.14 In this study, it was demonstrated that treatment with sutimlimab effectively inhibited Weislab-CP activity and CH50 with a decrease from baseline sustained through the treatment period and a return to baseline following treatment discontinuation. The platelet count among responders was highly correlated with CP activity. The results of the current study provide further clinical support for the role the classical complement pathway plays in a subset of patients with ITP.
Our study population was representative of patients with chronic/refractory ITP. Most patients had previously failed TPO-RA and/or rituximab therapy and one-third had undergone splenectomy. The rapid onset and sustained effect of sutimlimab suggest that at least a subset of patients with chronic/refractory ITP may have complement-mediated ITP and that C1s inhibition may be beneficial in these patients. The responder analysis revealed that 5 out of 12 patients (42%) achieved a durable response with sutimlimab as monotherapy; each of these patients had previously failed to respond to TPO-RA. Further exploration of patient characteristics such as disease duration, splenectomy status, and complement biomarkers may help to reveal potential predictors of clinical response to sutimlimab.
Although the main limitations of our study were its single-arm design and small sample size, both of which reflect the rarity of ITP, the study population was representative of difficult-to-treat patients with chronic and refractory disease course. All patients were required to have failed at least 2 prior ITP treatments. Data were not collected on whether patients ever had responded to previously received therapy, which may be of interest for future studies. The lack of a control group was addressed, in part, by the inclusion of a washout period and retreatment if the patients experienced severe thrombocytopenia. The loss of platelet count response during sutimlimab washout and its rapid restoration upon retreatment is strong evidence of a direct clinical benefit of sutimlimab in ITP.
In summary, in patients with ITP, sutimlimab treatment was well tolerated with no new safety signals. Sutimlimab was associated with a rapid, sustained, and repeatable increase in the mean platelet count in 42% of the patients with chronic/refractory ITP. These results demonstrated that C1s inhibition can be an effective therapeutic approach for patients who have failed other therapies and support the hypothesis that activation of the classical complement pathway contributes to the clinical heterogeneity of ITP. Furthermore, the findings of this study support the further development of anti-C1s inhibitors for patients with ITP who are not responsive to currently available therapies.
Acknowledgments
The authors thank all study participants. Medical writing and editorial assistance were provided by Rhutika Dessai and Francis John Golder of Fishawack Health and Fiona Woodward of Lucid Group; all were funded by Sanofi.
This study was funded by Sanofi.
Authorship
Contribution: C.M.B., A.R., W.H., and A.D. contributed to study concept and/or design; M.S., D.J.K., A.R., and R.S. contributed to data acquisition; and all authors contributed to data analysis and/or interpretation. The authors had access to clinical trial data, full editorial control of the manuscript and provided their final approval of all content.
Conflict-of-interest disclosure: C.M.B., Alexion Pharmaceuticals, Inc: honoraria, research funding; Bioverativ: honoraria, research funding; Cellphire: honoraria, research funding; Incyte: honoraria, research funding; Rigel: honoraria, research funding; Sanofi Genzyme: honoraria, research funding. A.R., Sanofi: consultancy, honoraria; Roche: consultancy, honoraria, research funding; Novartis: consultancy, honoraria; Biocryst: consultancy, honoraria; Apellis: consultancy, honoraria; Alexion Pharmaceuticals, Inc: consultancy, honoraria, research funding. D.J.K., UpToDate: consultancy, honoraria, patents, royalties; Shionogi: consultancy, honoraria; Momenta: consultancy, honoraria; Merck Sharp & Dohme: consultancy, honoraria; Kyowa-Kirin: consultancy, honoraria; Kezar Life Sciences, Inc: other, research funding; CRICO: consultancy, honoraria; Caremark: consultancy, honoraria; Immunovant: other: travel expenses, research funding; Bristol-Myers Squibb: consultancy, honoraria, other: travel expenses, research funding; Argenx: consultancy, honoraria, other: travel expenses, research funding; Sanofi (Genzyme): consultancy, honoraria; Zafgen: consultancy, honoraria; Protalex: consultancy, honoraria, research funding; Shionogi: consultancy; Protalix Biotherapeutics: consultancy; Shire: consultancy, honoraria; Principia: consultancy, research funding; Dova: consultancy, honoraria; Takeda: consultancy, honoraria, other, research funding; Rigel: consultancy, honoraria, other, research funding; Protalex: consultancy, honoraria, other, research funding; Principia Biopharma: consultancy, honoraria, other, research funding; Incyte: consultancy, honoraria; Immunovant: consultancy, honoraria; Genzyme: consultancy, honoraria; Amgen: consultancy, honoraria, other: travel expenses, research funding; Alnylam: consultancy, honoraria, other: travel expenses, research funding; Agios: consultancy, honoraria, other: travel expenses, research funding; Daiichi Sankyo: consultancy, honoraria; Actelion (Syntimmune): consultancy, honoraria, other: travel expenses, research funding; UCB: consultancy, honoraria; Platelet Disorder Support Association: consultancy, honoraria; Pfizer: consultancy, honoraria; Novartis: consultancy, honoraria. M.S., Takeda: consultancy, speakers bureau; Takeda: speakers bureau; Novartis: other: advisory board, speakers bureau; Alexion: consultancy, speakers bureau; Shire/Takeda: other: advisory board, research funding, speakers bureau; Ablynx/Sanofi: consultancy, other: advisory board, speakers bureau; Sanofi: consultancy, speakers bureau. R.S., Bioverativ: honoraria; Alnylam: honoraria. J.W., Sanofi: current employment. C.R., Sanofi: employment at the time of the study (ended employment in the past 24 months). W.H., Sanofi: employment at the time of the study (ended employment in the past 24 months). A.D., Sanofi: current employment, current equity holder in publicly traded company.
Correspondence: Catherine M. Broome, Division of Hematology and Oncology, MedStar Georgetown University Hospital, 3800 Reservoir Rd NW, Washington, DC 20007; e-mail: catherine.m.broome@gunet.georgetown.edu.
References
Author notes
Qualified researchers may request access to patient-level data and related study documents, including the clinical study report, study protocol with any amendments, blank case report form, statistical analysis plan, and data set specifications. Patient-level data will be anonymized, and study documents will be redacted to protect the privacy of our trial participants. Further details on Sanofi’s data sharing criteria, eligible studies, and process for requesting access can be found at https://vivli.org/.
The full-text version of this article contains a data supplement.