TO THE EDITOR:
The European Leukemia Network (ELN) classification, which is based on molecular and cytogenetic findings,1 and the Knowledge Bank approach, which is based on machine learning,2 are 2 recognized models that predict outcomes in acute myeloid leukemia (AML). However, there is discordance between these 2 prediction models, with a 20% difference in risk stratification between the Knowledge Bank approach and ELN model in one third of patients.2 Because AML is prevalent in older patients, there is a considerable need to develop robust stratification models to inform therapeutic decisions in the older population of patients with AML.
To address this gap, the Acute Leukemia French Association 1200 (ALFA-1200) group developed a model based on cytogenetics and 7 mutations to predict responses and outcomes of older patients (age 60 years or older) with AML who are receiving intensive chemotherapy with cytarabine continuously for 7 days, along with short infusions of an anthracycline on each of the first 3 days (7 + 3).3 Itzykson et al3 used an adaptive least absolute shrinkage and selection operator (LASSO)–penalized Cox model to screen out mutations in genes that are significantly associated with overall survival (OS) status. By rounding up the coefficients and summarizing the overall impact, their analysis classified patients with AML into 3 groups in order of decreasing benefit from intensive chemotherapy: “go-go,” “slow-go,” and “no-go.” We therefore sought to investigate whether the ALFA-1200 predictive model applied to 7 + 3 could also be validated in newly diagnosed patients with AML age 60 years or older and treated at our institution with intensive chemotherapy induction regimens (supplemental Table 1). This study has an institutional review board approval from the MD Anderson Cancer Center (MDACC) and was conducted in accordance with the Declaration of Helsinki.
At our institution, older patients with AML are usually treated with nonintensive chemotherapy. Nevertheless, we retrospectively identified 130 consecutive patients with AML who were age 60 years or older who did not receive myeloid-directed therapy (ie, hypomethylating agents, JAK2 inhibitors, or lenalidomide) before their diagnosis of AML and were treated at MDACC between January 2010 and October 2020. By focusing on patients who did not receive previous myeloid-directed therapy, we aimed to discern treatment responses independent of resistance to previous therapies. All 130 (100%) of 130 patients had complete cytogenetic, molecular, and clinical information, which allowed us to apply the ALFA-1200 model. Supplemental Table 2 summarizes the clinical and demographic characteristics of these patients. Briefly, the median age of the population was 64 years (range, 60-86 years); 60 (46%) of 130 were females, and 30 (23%) of 130 had secondary AML. ELN stratification was favorable in 37 (28%) of 130, intermediate in 64 (49%) of 130, or adverse in 29 (22%) of 130 patients. Core binding factor (CBF)–defining conventional cytogenetics, defined as patients who harbored any of t(8;21), inv(16), or t(16;16), were evident in 37 (28%) of 130 patients, whereas 16 (12%) of 130 patients had TP53 mutations. A total of 31 (24%) of 130 patients received allogeneic stem cell transplantation after their first-line intensive chemotherapy treatment. The median OS for the total population was 14.76 months.
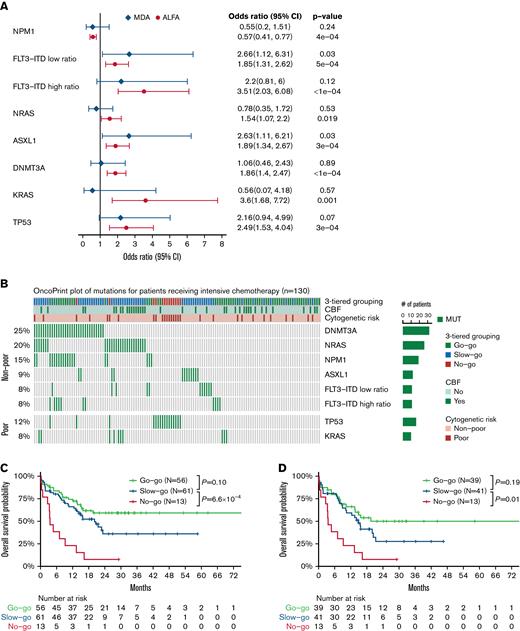
Compared with patients in the ALFA-1200 study, we had a similar distribution of patients attaining complete remission in the poor and non-poor cytogenetics groups: 48% (14 of 29; MDACC) compared with 56% (47 of 84; ALFA-1200) (χ2, 0.25; df, 1; P = .62) for the poor cytogenetic group and 80% (81 of 101; MDACC) compared with 76% (294 of 387; ALFA-1200) (χ2, 0.58; df, 1; P = .44) for the non-poor cytogenetic group (supplemental Table 2). We then conducted the multivariable Cox model for OS in patients based on poor and non-poor cytogenetic risk stratification (Figure 1A). The overall concordance of the multivariable Cox model is 0.66 for the non-poor cytogenetic group in our cohort, similar to the concordance of 0.72 in the ALFA-1200 study.
Outcomes of MD Anderson cohort in comparison to ALFA-1200 cohort. (A) Comparison of odds ratios between ALFA-1200 and MDACC models. Classifications by cytogenetic risks, odds ratios, and P values were calculated in multivariable Cox models. The OS-fitting model was constructed on the data sets from the ALFA-1200 study group and MDACC. Error bars indicate 95% confidence intervals. (B) OncoPrint plot of relevant factors among all patients (n = 130). Mutations detected by the ALFA-1200 model, status of 3-tier grouping, CBF, and cytogenetic risks were included. (C-D). OS curves of 3-tier grouping for all patients (n = 130) and patients without CBF (n = 93). Kaplan-Meier analysis and pairwise log-rank test were conducted, and P values were adjusted by the Benjamini-Hochberg method in multiple comparisons.
Outcomes of MD Anderson cohort in comparison to ALFA-1200 cohort. (A) Comparison of odds ratios between ALFA-1200 and MDACC models. Classifications by cytogenetic risks, odds ratios, and P values were calculated in multivariable Cox models. The OS-fitting model was constructed on the data sets from the ALFA-1200 study group and MDACC. Error bars indicate 95% confidence intervals. (B) OncoPrint plot of relevant factors among all patients (n = 130). Mutations detected by the ALFA-1200 model, status of 3-tier grouping, CBF, and cytogenetic risks were included. (C-D). OS curves of 3-tier grouping for all patients (n = 130) and patients without CBF (n = 93). Kaplan-Meier analysis and pairwise log-rank test were conducted, and P values were adjusted by the Benjamini-Hochberg method in multiple comparisons.
Similar to the non-poor cytogenetic group in the ALFA-1200 study, mutations in NPM1 were associated with improved outcomes, whereas mutations in FLT3-ITD (low and high allelic ratios) and ASXL1 were associated with worse outcomes. However, unlike the findings in the ALFA-1200 study, DNMT3A mutations in our patients were not significantly associated with outcomes (P = .89), which is consistent with other studies demonstrating that DNMT3A mutations may not have prognostic significance in AML.4,5 Not surprisingly, TP53 mutations were associated with worse outcomes in the poor cytogenetics group. However, mutations in NRAS in the non-poor cytogenetics group and KRAS in the poor cytogenetic group tended to be associated with improved outcomes in contrast to the results of the ALFA-1200 study. Our findings were limited by the small sample size of our cohort. However, a previous study by Cancer and Leukemia Group B demonstrated that patients with AML who had RAS mutations were likely to benefit from high-dose cytarabine,6 which was the backbone of intensive chemotherapy regimens in our cohort and may have influenced the improved outcomes in patients with RAS mutations in our cohort. Sensitivity to deoxycytidine analogs was previously shown in in vitro AML cell lines with RAS mutations.7 Specifically, mutated RAS synergizes with higher doses of cytarabine in AML, leads to failure of arrest in the S phase of the cell cycle, activation of the TP53-dependent DNA damage response programs, and increased myeloid differentiation, and it ultimately leads to a cytotoxic response.7,8
We then performed 3-tier cluster analysis based on the criteria for responses proposed in the ALFA-1200 study (Figure 1B; supplemental Table 3). A total of 56 (43%) of 130 patients were classified in the go-go group, 61 (46%) of 130 were classified in the slow-go group, and 13 (10%) of 130 were classified in the no-go group (Figure 1B). The average 2-year OS was 20.54 months for the go-go group, 15.57 months for the slow-go group, and 7.17 months for the no-go group (P < .0001) (Figure 1C). The inferior outcomes of the no-go group may be largely driven by the TP53 mutant phenotype. However, unlike the discovery cohort in the ALFA-1200 study, the 3-tier survival analysis did not demonstrate significant differences between the go-go and slow-go groups in our population of patients age 60 years or older who were treated with higher-dose cytarabine-based induction therapies. Our data were more consistent with the ALFA-1200 validation cohorts (Hauts-de-France and Studien Allianz Leukämie), in which the differences in outcomes for the go-go and slow-go groups were more subtle. Although these differences could be related to relatively shorter follow-up time in the validation cohorts of the ALFA-1200 study, our patient cohort had a relatively long follow-up (median follow-up, 20.1 months), with median OS time reaching 28.53 months for the go-go group and 20.09 months for the slow-go group. One of the limitations in our study was the enrichment of CBF patients with AML because intensive chemotherapy is typically reserved for older patients with AML at our institution. We therefore hypothesized that the lack of significance in outcomes in the go-go and slow-go groups is a result of their enrichment with CBF AML (30% and 33%, respectively), which are subsets of patients with AML known to have better outcomes when treated with intensive chemotherapy.8 However, when we excluded the CBF patients from our analysis, the differences in outcomes between go-go and slow-go groups were still subtle (P = .191) (Figure 1D).
The main advantage of the ALFA-1200 model is its simple approach in categorizing older patients with AML with respect to benefit from intensive chemotherapy using only baseline genomic factors. Our validation cohort suggests that the ALFA-1200 3-tiered model confirms that TP53 mutations in AML portend worse outcomes and lower responses to intensive chemotherapy in the older population of patients with AML as has been published by many groups. Furthermore, the findings are consistent with expectations that patients with AML who have CBF alterations which were enriched in the go-go and slow-go groups have better outcomes when treated with intensive chemotherapy. However, the cytogenetic and molecular characteristics that may differentiate the go-go and slow-go groups (ie, non–TP53-mutated tiers) may benefit from further refining before widespread applicability. For example, similar to the way the ALFA-1200 group separated out poor and non-poor cytogenetics, one may also consider a completely separate group for patients with CBF AML. Of note, our validation cohort suggests that patients with RAS mutations may benefit from high-dose cytarabine induction regimens, and RAS mutations may not be adverse. Nevertheless, the current model by the ALFA-1200 group provides a promising and easy-to-use tool to build on as we move toward precision oncology in AML. A multicenter, prospective study that incorporates the cytogenetic risk stratification in predicting responses to intensive chemotherapy can help confirm these results. Importantly, integrating more recently recognized characteristics associated with outcomes such as subclonal architecture9 and minimal residual disease10 may provide additional insightful information in predicting outcomes in AML.
Contribution: H.A.A. designed, supervised, wrote, and analyzed the study; H.S. and Z.L. co-analyzed the study; S.P. performed data collection; R.K.S. performed hematopathology confirmation; M.Y., G.B., A.J.P.D., E.J., M.K., N.J.S., C.D., N.D., F.R., and T.M.K. contributed to the study design, writing, and analysis; and all authors reviewed the manuscript.
Conflict-of-interest disclosure: E.J. received research grants from Amgen, AbbVie, Adaptive Biotechnologies, Pfizer, Takeda, and Johnson & Johnson and served as a consultant for Amgen, AbbVie, Adaptive Biotechnologies, Pfizer, Takeda, Johnson & Johnson, Bristol Myers Squibb, Novartis, Genentech, and Incyte. C.D. received research grants from AbbVie, Agios/Servier, Astex, Calithera, Celgene/Bristol Myers Squibb, Cleave, Daiichi-Sankyo, ImmuneOnc, and Loxo and honoraria from AbbVie, Agios/Servier, Astellas, Celgene/Bristol Myers Squibb, Cleave, Foghorn, Genentech, ImmuneOnc, Novartis, Notable Labs, and Takeda. The remaining authors declare no competing financial interests.
Correspondence: Hussein A. Abbas, Department of Leukemia and Department of Genomic Medicine, MD Anderson Cancer Center, 1515 Holcombe Blvd, Houston, TX 77030; e-mail: habbas@mdanderson.org.
References
Author notes
The full-text version of this article contains a data supplement.
H.A.A. and H.S. contributed equally to this work.