Key Points
Four doses of Aba can be safely added to standard 2-drug GVHD prophylaxis in URD HCT for pediatric bone marrow failure.
No severe acute or chronic GVHD was seen in pediatric patients with bone marrow failure with Aba-containing prophylaxis after URD HCT.
Abstract
Hematopoietic cell transplantation (HCT) is the only readily available cure for many life-threatening pediatric nonmalignant diseases (NMD), but most patients lack a matched related donor and are at higher risk for graft-versus-host disease (GVHD). Use of abatacept (Aba) to target donor T-cell activation has been safe and effective in preventing GVHD after unrelated donor (URD) HCT for malignant diseases (Aba2 trial). Our primary objective was to evaluate the tolerability of Aba added to standard GVHD prophylaxis (cyclosporine and mycophenolate mofetil) in pediatric patients with NMD undergoing URD HCT. In this single-arm, single-center phase 1 trial, 10 patients receiving reduced intensity or nonmyeloablative conditioning underwent URD HCT. Immune reconstitution was assessed longitudinally via flow cytometry and compared to pediatric patients on Aba2. Nine patients successfully engrafted, with 1 primary graft rejection in the setting of inadequate cell dose; secondary graft rejection occurred in 1 patient with concurrent cytomegalovirus viremia. Two deaths occurred, both unrelated to Aba. One patient developed probable posttransplant lymphoproliferative disease, responsive to rituximab and immune suppression withdrawal. No patients developed severe acute or chronic GVHD, and 8 patients were off systemic immunosuppression at 1 year. Immune reconstitution did not appear to be impacted by Aba, and preservation of naïve relative to effector memory CD4+ T cells was seen akin to Aba2. Thus, 4 doses of Aba were deemed tolerable in pediatric patients with NMD following URD HCT, with encouraging preliminary efficacy and supportive immune correlatives in this NMD cohort.
Introduction
Allogeneic hematopoietic cell transplantation (HCT) is the only standard-of-care curative therapy for many severe nonmalignant diseases (NMDs) which affect children.1-4 While a diverse group of diseases, including highly prevalent hemoglobinopathies and less prevalent diseases such as severe aplastic anemia (SAA) and Fanconi anemia (FA), they universally lead to significant morbidity and early mortality. These diseases can be cured with a HCT, without which patients face a myriad of complications, including progressive organ dysfunction and malignancy. For the transplant to succeed, patients must avoid several transplant-related complications, the most serious of which is graft-versus-host disease (GVHD). Activation of donor T cells drives GVHD, which is one of the leading causes of death following HCT. For children with an NMD receiving transplantation using a matched-related donor (MRD), GVHD can be effectively prevented with standard 2-drug calcineurin inhibitor–based prophylaxis, resulting in excellent outcomes.4-6 As the majority of children lack a MRD, unrelated donors (URDs) are used, increasing histoincompatibility and thus risk for GVHD7 as well as graft rejection.8 Thus, whereas URD HCT offers the hope of cure for most children with an NMD, GVHD poses a substantial barrier. There is a critical unmet need for a more efficacious, T-cell directed GVHD prevention that will more safely permit expansion of URD HCT to all children with life-threatening NMD lacking an MRD.
Donor T-cell activation occurs in part through CD28:CD80/86 costimulatory signaling,9 wherein T-cell CD28 signaling synergizes with signaling through the T-cell receptor, leading to enhancement of T-cell survival, proliferation, and secretion of inflammatory cytokines.10,11 Agents have been developed to selectively block this costimulatory interaction, including CTLA4-immunoglobulin (abatacept [Aba]), which is a fusion protein combining the CTLA4 binding domain and the immunoglobulin G1 Fc region.12 Aba was initially Food and Drug Administration (FDA) approved for the treatment of rheumatoid arthritis in adult and pediatric patients,13 with the related compound belatacept FDA approved for renal transplantation.14 Following demonstration of efficacy in preclinical models of GVHD,15,16 we completed a 10-patient, single-center, phase 1 trial of Aba (4 doses on days −1, 5, 14, and 28) in combination with standard 2-drug GVHD prophylaxis in URD HCT for malignant disease.17 In addition to demonstrating tolerability of Aba, pharmacokinetics were confirmed and possible efficacy seen, with no grade IV acute GVHD (aGVHD) and no GVHD-related deaths. In our subsequent phase 2, multicenter trial (Aba2), the safety and efficacy of Aba was further examined in 2 strata: 8 of 8 HLA-matched URD transplants randomized between Aba or placebo and 7 of 8 HLA-mismatched URD, all assigned to receive Aba. Compared to a prespecified matched cohort from the Center for International Blood and Marrow Transplant Research, patients with mismatched URD receiving Aba had significantly lower rates of severe (grade III-IV) aGVHD and transplant-related mortality, which translated into an overall and disease-free survival benefit.18,19 Based upon this phase 2 data, in December 2021, Aba received FDA approval for GVHD prophylaxis (combined with a calcineurin inhibitor and methotrexate [MTX]) in patients ≥2 years undergoing URD HCT.
The objective of this single-arm, phase 1 trial was to examine the safety and early efficacy of Aba added to standard 2-drug GVHD prophylaxis in URD HCT for NMD. We hypothesized that Aba would prevent GVHD while maintaining engraftment and protective immunity against infectious complications of transplant, thus, significantly improving cure rates for children with life-threatening NMD.
Methods
Study design and patients
We performed a single-center, phase 1 clinical trial in pediatric patients (age, 0-21 years) undergoing URD HCT for a life-threatening NMD. Patients were enrolled through the Aflac Cancer and Blood Disorders Center within Children’s Healthcare of Atlanta. The trial was approved by the Institutional Review Boards of Emory University and Children’s Healthcare of Atlanta and was registered at www.clinicaltrials.gov as #NCT01917708. Informed consent was obtained from patients and/or legal guardians. Patients were eligible if they (1) had a serious NMD, including acquired or inherited bone marrow failure (BMF); (2) lacked an MRD; and (3) had an available 7 or 8 of 8 HLA-matched URD, without antibodies directed to a disparate HLA molecule. Eligible stem cell sources included bone marrow (BM), peripheral blood, or cord blood; however, all enrolled patients received BM as their stem cell source. All patients were followed for 2 years post-HCT.
The trial originally included a randomization between 4 and 6 doses of Aba, with planned enrollment of 20 patients (10 patients per arm). Due to a theoretical concern that Aba could impact hematopoietic stem cell engraftment in a nonmalignant cohort, the trial was amended in April 2016 to include a single arm of 4 doses of Aba, the schedule previously evaluated in a malignant disease cohort. With this amendment, target enrollment was decreased to 10. Before this amendment, a single enrolled patient (patient ID 6) had been randomized to 6 doses of Aba; however, doses 5 and 6 were held in this patient due to Epstein-Barr virus (EBV) viremia. Consequently, data on all 10 patients were analyzed together.
Treatment protocol
Conditioning regimen
Patients received 1 of 3 reduced intensity conditioning (RIC) or nonmyeloablative (NMA) regimens based upon disease and/or physician preference. All patients with SAA received rabbit antithymocyte globulin (5 mg/kg per dose IV on days −10 to −8), fludarabine (25 mg/m2 per dose IV on days −7 to −2), cyclophosphamide (50 mg/kg IV on day −2), and total body irradiation (300 cGy as a single fraction on day −1; per Blood and Marrow Transplant Clinical Trials Network 0301). All patients with FA received rabbit antithymocyte globulin (5 mg/kg per dose IV on days −10 to −8), fludarabine (25 mg/m2 per dose IV on days −10 to −5), and cyclophosphamide (10 mg/kg per dose IV on days −5 to −2).20 Patients with other (non-FA and non-SAA) eligible diseases originally received the SAA conditioning regimen; however, an amendment in October 2015 permitted physicians to select between either this total body irradiation–based regimen or a chemotherapy-only regimen. This latter regimen consisted of alemtuzumab (3 mg IV test dose on day −22, followed by 10 mg/m2 on day −21, 15 mg/m2 on day −20, and 20 mg/m2 on day 19), fludarabine (30 mg/m2 per dose IV on days −6 to −2), thiotepa (8 mg/kg IV on day −3), and melphalan (140 mg/m2 IV on day −2).21
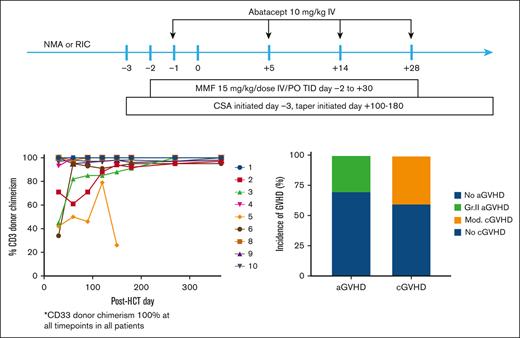
GVHD prophylaxis
All patients received Aba (study drug) in combination with standard 2-drug GVHD prophylaxis in an NMD cohort (cyclosporine [CSA] and mycophenolate mofetil [MMF]). CSA was initiated on day −3, with dose adjusted to maintain a level of 200 to 300 ng/mL (via mass spectrometry) and taper initiated between days +100 and +180. MMF was administered at 15 mg/kg per dose (maximum dose of 1000 mg) 3 times daily from days −2 to +30. Aba was administered IV at 10 mg/kg per dose based on actual weight, with a maximum dose of 1000 mg. In cases where the calculated dose was ≤110% of a simple multiple of a 250-mg vial, the dose could be rounded down to the nearest multiple. Aba was infused on days −1, +5, +14, and +28 over 1 hour, with diphenhydramine premedication.
Clinical end points
The primary objective of this study was to determine the tolerability of adding 4 doses of Aba (investigational) to standard 2-drug GVHD prophylaxis in pediatric patients undergoing URD HCT for a serious NMD. Tolerability was defined as success in administering all prescribed doses of Aba. Poor tolerability was defined as >1 dose of Aba being withheld per protocol, death from an infection within 30 days of last dose of Aba (without preceding systemic immunosuppression for GVHD), or posttransplant lymphoproliferative disease (PTLD) within 100 days of last dose of Aba (without preceding systemic immunosuppression for GVHD). Overall tolerability was defined as ≥7 of 10 patients tolerating Aba. In addition, infusion reactions, grade ≥2 regimen-related toxicities (through day +42, according to Bearman criteria), graft failure (primary and secondary), graft loss, aGVHD and chronic GVHD (cGVHD) (using National Institutes of Health consensus criteria), and unexpected serious adverse events (SAEs) were captured.
Immune monitoring
A secondary objective of this study was to assess the immunological effects of Aba. Longitudinal flow cytometry analysis included the enumeration of natural killer (NK) cells (CD3−/CD20−/CD16+/CD56hi/lo) and CD20−/CD3+/CD4+/CD8− and CD20−/CD3+/CD4−/CD8+ T cells, including naïve (CCR7+/CD45RA+), central memory (CCR7+/CD45RA−), effector memory (CCR7−/CD45RA−), and terminal effector memory subsets (CCR7−/CD45RA+). The antibody clones used for the flow cytometric analysis are as follows: CD3 (UCHT1; BD, Franklin Lakes, NJ), CD20 (H147; Invitrogen, Grand Island, NY), CD16 (3G8; BD), CD56 (B159; BD), CD8 (RPA-T8; eBioscience, San Diego, CA), CD4 (RPA-T4; BD), CD2 (RPA-2.10; BD), CD45RA (MEM-56; Invitrogen), and CCR7 (3D12; BD).
Immune studies were compared in patients <21 years treated on the separate phase 2 Aba URD HCT trial for malignant diseases (Aba2).19 Patients from the Aba2 trial received majority myeloablative conditioning (MAC) and received standard 2-drug GVHD prophylaxis for a malignant disease cohort (MTX and CSA), combined with Aba. Matched (8/8) recipients were randomized between Aba and placebo and mismatched (7/8) recipients received Aba.
Statistical analysis
Statistical analyses were performed using Prism version 8 for Mac OS (GraphPad Software, La Jolla, CA). Dunn's test was used to compare Aba NMD immune reconstitution to each Aba2 group, with significance level set at P < .05. Data were analyzed by E.O.S. and Y.S., with access to primary trial data available to all authors.
Results
Patient characteristics
From June 2014 to September 2019, 10 patients were enrolled and underwent transplantation at a median age of 6 years (Table 1) (range, 0.5-18 years). All patients underwent transplant for inherited or acquired BMF, most commonly SAA (n = 3) and FA (n = 3). Conditioning for patient IDs 1 through 8 was protocol-defined; patient IDs 9 and 10 received chemotherapy-only conditioning according to treating physician preference. All patients received BM as their stem cell source, and half of the grafts were HLA mismatched (7/8). A majority of the recipients were cytomegalovirus (CMV) negative (n = 7) and EBV+ (n = 6). Major ABO mismatch was present in 4 donor-recipient pairs. Median infused cell doses were 4.1 × 108 total nucleated cells (TNCs) per kg (range, 0.6 × 108 to 7.6 × 108) and 7.1 × 106 CD34+ cells per kg (range, 2.0 × 106 to 13.0 × 106).
Engraftment and survival outcomes
Engraftment was successful in 9 of 10 patients, with median time to neutrophil engraftment of 20 days and to platelet engraftment of 16 days. Primary graft failure occurred in 1 patient (patient ID 7) who had refractory SAA and whose graft contained an inadequate TNC dose of 0.6 × 108/kg (though CD34+ dose of 3.8 × 106/kg); despite a second transplant (haploidentical, 63 days from first), this patient died on day +73 from marrow aplasia and disseminated Fusarium infection. Secondary graft failure occurred on day +146 in 1 patient (patient ID 5), who had congenital dyserythropoietic anemia and concurrent CMV reactivation; this patient is doing well following a second URD transplant. In the 8 patients with successful long-term engraftment, myeloid (CD33) donor chimerism was 100% at day ≥30; T-cell (CD3) donor chimerism was mixed initially (day +30: median, 95% donor; range, 34% to 100%), but it reached ≥95% in all patients by day +270. Patient ID 1 died from Wilms tumor 1.5 years after successful transplant, which was assessed as related to a constitutional chromosome abnormality and as being unrelated to study drug.
Tolerability of Aba administration and SAEs
All evaluable patients received the 4 scheduled doses of Aba. Patient ID 7 was not evaluable for the primary outcome of tolerability as she was taken off protocol due to confirmed primary graft failure (with dose #4 of Aba subsequently held). No evaluable patients died from infection within 30 days of last Aba dose. One patient (patient ID 6) was diagnosed with probable PTLD within 100 days of last Aba dose (Table 2; further details in "Infections" below). Thus, 8 of 9 evaluable patients tolerated Aba, and Aba was deemed tolerable.
Patient ID 7 was febrile at the time of the third dose of Aba, otherwise no infusion reactions occurred. Regimen-related toxicity was grade I-II, except for grade III stridor that developed in patient ID 1, which improved with racemic epinephrine. SAEs were expected following URD HCT and included: grade 3 fever, dehydration, respiratory distress, anorexia, and weight loss; grade 4 fever and neutropenia (possibly related), sepsis (possibly related), sinusitis, acute kidney injury, and seizure.
Infections
As shown in Table 2, CMV and EBV viremia occurred in 3 patients each, with 1 patient (patient ID 5) having reactivation of both viruses. Viremia responded in all patients to standard antiviral therapy. No patients developed CMV disease. Patient ID 6 was diagnosed with probable EBV-driven PTLD in setting of viremia with cervical lymphadenopathy (maximum 1 cm, with no computed tomography scan or biopsy performed), which responded to rituximab (4 weekly doses) and withdrawal of immune suppression. Maximum EBV polymerase chain reaction was 106 372 IU/mL, following 2 doses of rituximab; lymphadenopathy resolved following 1 dose of rituximab.
Aside from patient ID 7 who had recurrent infections (genital herpes simplex virus with viremia, invasive fungal infection, Escherichia coli and Enterobacteriaceae species bloodstream infections, and Clostridium difficile colitis) in the setting marrow aplasia, other infections were expected for a transplant cohort: upper respiratory infection due to rhinovirus/enterovirus (n = 3), human metapneumovirus (n = 1), and coronavirus (n = 1); BK cystitis/viremia (n = 1); central-line associated bloodstream infection (n = 2); and C difficile colitis (n = 2, both following systemic antimicrobials).
GVHD
No patients developed severe aGVHD (grade III-IV) or severe cGVHD (Table 3). Maximum grade II aGVHD developed in 3 patients, which was treated with topical steroids in 1 patient (patient ID 8) and systemic steroids in 2 patients. Moderate cGVHD (all involving skin) occurred in 4 patients, 3 of whom had prior aGVHD. Only 1 patient required systemic treatment (patient ID 9), with others responding to topical steroids alone (patient ID 10 received systemic steroids but only for 2 days). Aside from patient ID 9 who required systemic immune suppression for treatment of cGVHD through 3.6 years, all other patients were off systemic immune suppression by 1-year posttransplant (median, 238 days). Lansky score at 1 year was 100% in all patients, except for patient IDs 1 and 3 with score of 80%, both of whom had baseline score of 80% to 90%.
Immune monitoring
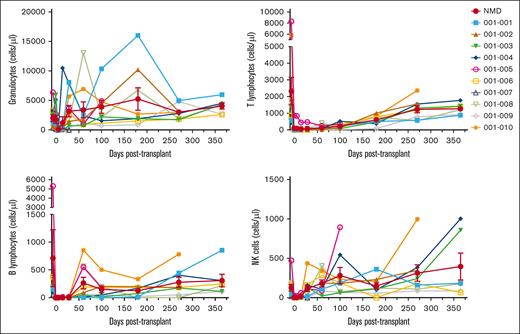
Longitudinal immune reconstitution via flow cytometry was performed, with individual and summary data shown in Figures 1 and 2. Mean granulocyte count returned to pre-HCT baseline and NK cell count normalized by day 30, with mean B- and T-cell counts normalizing by day 60 and between days 180 and 270, respectively. CD8+ T cells recovered before CD4+, with preservation in the proportion of naïve CD4+ T cells relative to effector memory T cells.
Longitudinal immune reconstitution following URD HCT with Aba GVHD prophylaxis in pediatric patients with NMD. By day 30 post-HCT, mean granulocyte count was 3171 cells per μL and mean NK cell count was 118 cells per μL. B-cell recovery preceded T cell, with mean B-cell count of 264 cells per μL on day 50 and mean T-cell count of 603 cells per μL on day 180 and 1238 cells per μL on day 270. Data shown as individual patient and mean with standard error of the mean (red line).
Longitudinal immune reconstitution following URD HCT with Aba GVHD prophylaxis in pediatric patients with NMD. By day 30 post-HCT, mean granulocyte count was 3171 cells per μL and mean NK cell count was 118 cells per μL. B-cell recovery preceded T cell, with mean B-cell count of 264 cells per μL on day 50 and mean T-cell count of 603 cells per μL on day 180 and 1238 cells per μL on day 270. Data shown as individual patient and mean with standard error of the mean (red line).
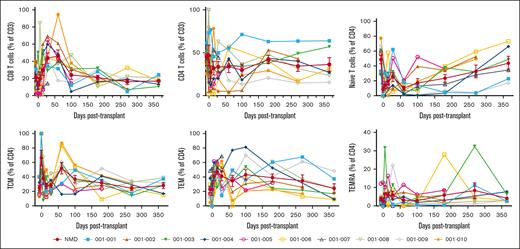
Preservation of naïve CD4+ T cells in pediatric patients with NMD receiving Aba GVHD prophylaxis. Within CD3+ T cells, the CD8+ fraction proportionally recovered before CD4+ T cells. Within the CD4+ T-cell fraction, central memory T cells (TCM) were the dominant population early post-HCT, and an increasing proportion of naïve T cells were seen over time. The proportion of effector memory T cells (TEM) within the CD4+ fraction decreased during the period of Aba administration, and the T effector memory CD45RA+ cells (TEMRA) proportion remained low throughout the follow-up period. Data shown as individual patient and mean with standard error of the mean (red line).
Preservation of naïve CD4+ T cells in pediatric patients with NMD receiving Aba GVHD prophylaxis. Within CD3+ T cells, the CD8+ fraction proportionally recovered before CD4+ T cells. Within the CD4+ T-cell fraction, central memory T cells (TCM) were the dominant population early post-HCT, and an increasing proportion of naïve T cells were seen over time. The proportion of effector memory T cells (TEM) within the CD4+ fraction decreased during the period of Aba administration, and the T effector memory CD45RA+ cells (TEMRA) proportion remained low throughout the follow-up period. Data shown as individual patient and mean with standard error of the mean (red line).
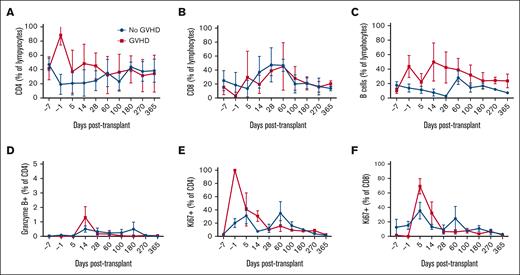
Additionally, data were compared between patients with NMD and the 3 treatment groups on the Aba2 HCT for malignant diseases trial (limited to patients aged <21 years): (1) 8 of 8 URD randomized to receive Aba, (2) 7 of 8 URD who all received Aba, and (3) 8 of 8 URD randomized to receive placebo (supplemental Figures 1 and 2). Patients with NMD had higher baseline T- and B-cell counts compared to those of 7 of 8 (P = .005 and P = .001, respectively) and 8 of 8 Aba groups (P = .046 and P = .005, respectively). Although lower T-cell counts were seen at day 28 in patients with NMD (P = .02 for 7/8 Aba and P < .0001 for 8/8 placebo), no difference was seen at or beyond day 100. NK cells were significantly lower in patients with NMD at day 28 (P = .04 for 7/8 Aba and P = .03 for 8/8 Aba) and day 365 (P = .005 for 7/8 Aba). Finally, as was seen in an analysis of all patients from the Aba2 trial,19 patients with NMD receiving Aba had preservation of naïve relative to effector memory CD4+ T cells, with statistically significant differences seen when compared to patients from the Aba2 trial aged <21 years who received 7 of 8 URD and 8 of 8 placebo (naïve T cells: P = .02 for day +365; effector memory T cells: P = .002 for day +180, P = .02 for day +270, and P = .0003 for day +365).
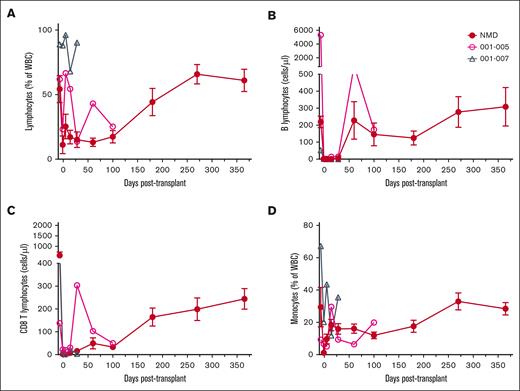
In patients with NMD receiving Aba, comparisons were made between patients with and without graft rejection (Figure 3) and GVHD (Figure 4). In patient ID 5 who had secondary graft rejection in the setting of CMV reactivation, there was a baseline and persistent lymphocytosis, with predominance of B cells and CD8+ T cells. A higher number of T cells in patient ID 5 expressed markers of proliferation (Ki67+) and cytotoxicity (Granzyme B+), particularly in CD8+ T cells (data not shown). In the patient with primary graft failure presumed due to low TNC cell dose (patient ID 7), a predominance of lymphocytes and monocytes was seen at baseline, despite leukopenia. In patients with aGVHD (patient IDs 1, 8, and 9), a higher percentage of CD4+ T cells was seen within lymphocytes (data not shown). Percentage of proliferating (Ki67+) CD4+ or CD8+ and cytotoxic (Granzyme B+) CD4+ T cells were higher in patients with any GVHD (acute or chronic). Specific to those with cGVHD (patient IDs 1, 8, 9, and 10), higher number and percent of B cells were seen.
Association between immune reconstitution and graft rejection in pediatric patients with NMD following URD HCT with Aba GVHD prophylaxis. Compared to nongraft failure patients, patient ID 5 (with secondary graft failure in setting of early CMV reactivation) had baseline and persistent lymphocytosis driven primarily by B and CD8 T cells, with high Ki67 and Granzyme B expression (data not shown). Patient ID 7 (with primary graft failure with low infused TNC dose) had leukopenia at baseline, with lymphocytic/monocytic dominance. WBC, white blood cell.
Association between immune reconstitution and graft rejection in pediatric patients with NMD following URD HCT with Aba GVHD prophylaxis. Compared to nongraft failure patients, patient ID 5 (with secondary graft failure in setting of early CMV reactivation) had baseline and persistent lymphocytosis driven primarily by B and CD8 T cells, with high Ki67 and Granzyme B expression (data not shown). Patient ID 7 (with primary graft failure with low infused TNC dose) had leukopenia at baseline, with lymphocytic/monocytic dominance. WBC, white blood cell.
Association between immune reconstitution and GVHD in pediatric patients with NMD following URD HCT with Aba GVHD prophylaxis. Patients with aGVHD (patient IDs 1, 8, and 9) had an early dominance of CD4 T cells within lymphocytes (data not shown). Patients with any GVHD had higher percentage of proliferating (Ki67) or cytotoxic (Granzyme B) T cells. Those with cGVHD (patient IDs 1, 8, 9, and 10) had higher total number (data not shown) and percentage of B cells.
Association between immune reconstitution and GVHD in pediatric patients with NMD following URD HCT with Aba GVHD prophylaxis. Patients with aGVHD (patient IDs 1, 8, and 9) had an early dominance of CD4 T cells within lymphocytes (data not shown). Patients with any GVHD had higher percentage of proliferating (Ki67) or cytotoxic (Granzyme B) T cells. Those with cGVHD (patient IDs 1, 8, 9, and 10) had higher total number (data not shown) and percentage of B cells.
Discussion
These preliminary data suggest that Aba can be safely added to CSA and MMF GVHD prophylaxis in pediatric patients with NMD undergoing URD HCT with NMA or RIC. Despite half of the patients having a mismatched (7/8) donor, rates of GVHD were encouraging, with no severe aGVHD (grade III-IV) or cGVHD and 7 of 8 fully engrafted patients off systemic immune suppression and with excellent performance score at 1 year. Addition of Aba to standard GVHD prophylaxis does not appear to significantly impact overall immune reconstitution in pediatric patients following URD HCT for NMD, including when compared to pediatric Aba2 groups. Comparison between Aba NMD and Aba2 groups may be impacted by differences in conditioning intensity or GVHD prophylactic agents given with Aba, however, preservation of naïve CD4+ T cells (over effector memory) in patients with Aba NMD mirrored data from the overall Aba2 trial.19 Overall, these data support continued evaluation of Aba for GVHD prophylaxis in the NMD setting.
Our findings are consistent with published results from the pilot trial17 and the phase 2, multicenter, and randomized trial19 of Aba in URD HCT for malignant diseases, who notably received predominantly MAC compared to all NMA or RIC in our NMD cohort. Specifically, addition of 4 doses of Aba to standard 2-drug GVHD prophylaxis (CSA/MTX in malignant diseases and CSA/MMF in NMD) appears to be safe in patients with NMD, without increase in infections or SAEs above those expected following URD HCT. One patient did have probable PTLD, with PTLD being a known complication of costimulation blockade (particularly with second generation belatacept). Notably, rates of PTLD on the Aba2 trial did not differ significantly between 8 of 8 URD Aba and placebo groups (2.8% vs 0%, P = .18). Given known higher risk of graft rejection in patients with NMD, it is important to note that Aba does not appear to increase this risk; rejection events could be multifactorial, with low graft TNC in 1 primary graft rejection event and concurrent CMV viremia in 1 secondary graft rejection event.
Two previous studies have evaluated Aba GVHD prophylaxis in NMD, first in mismatched related donor (haploidentical) HCT for SAA and the second in URD (BM and cord blood) for sickle cell disease.22,23 In the SAA trial, conditioning was reduced intensity and Aba was given ×9 doses (through day +180), combined with sirolimus and posttransplant cyclophosphamide. In the sickle cell disease trial, conditioning was reduced intensity and Aba was given ×4 (through day +100; cord) or 8 doses (through day +365; BM, aside from first 2 patients), combined with tacrolimus + MTX (BM) or MMF (cord). Overall, both studies demonstrated low rates of severe aGVHD, cGVHD, and transplant-related mortality, thus provide support for extended dosing of Aba (beyond 4 doses). Our results expand into inherited BMF (FA, Diamond-Blackfan anemia, severe congenital anemia, and congenital dyserythropoietic anemia), URD for SAA, and NMA conditioning (for patients with FA), while providing further support for Aba combined with RIC.
Limitations of our trial include it being limited to 10 patients at a single center; however, akin to our initial evaluation of Aba in patients with malignant disease,17 it was important to first evaluate Aba’s safety in this NMD cohort with different risks including higher risk for graft rejection. Given our single-arm design and lack of a historical control group for immune correlatives, comparisons were limited to pediatric age patients (<21 years) on the Aba2 trial who received primarily MAC and Aba in combination with CSA and MTX, which may have impacted our findings. Nonetheless, immunophenotyping from patients with Aba NMD is consistent with findings in the entire Aba2 cohort and interesting hypothesis-generating findings were seen comparing groups with and without graft rejection or GVHD.
In conclusion, the addition of 4 doses of Aba to standard 2-drug GVHD prophylaxis with CSA and MMF in pediatric patients with NMD undergoing URD HCT appears to be safe, with encouraging efficacy signal including lack of severe GVHD. Given the 2 cases of graft rejection in this NMD cohort, rejection (in addition to GVHD) is a primary focus in our subsequent ongoing multicenter, phase 2 trial (#NCT03924401), which additionally incorporates extended Aba dosing (×8 doses) to better prevent cGVHD and which has been supported by other trials.22
Acknowledgments
This work was supported, in part, by research funding from the National Heart, Lung, and Blood Institute, National Institutes of Health (award number K23HL133446 [E.O.S.]) and a grant from the Pediatric Hematology Oncology Research Group (E.O.S.).
Authorship
Contribution: E.O.S., L.K., and J.H. designed the trial; E.O.S., B.W., K.R., K.-Y.C., A.H., K.L., M.Q., Y.S., and J.H. participated in trial execution and data collection; E.O.S. and Y.S. analyzed the data; and all authors interpreted the data, critically reviewed the manuscript, provided final approval for submission, and agree to be accountable for all aspects of the work, ensuring the accuracy and integrity of the publication.
Conflict-of-interest disclosure: M.Q. reports grants and personal fees from Bristol Myers Squibb (BMS) during the conduct of the study; consulting fees from Medexus, Jazz Pharmaceuticals, and Mesoblast; and a patent “Method to prevent relapse after transplant” that is pending. B.W. reports personal fees from BMS during the conduct of the study and has a patent “Method to prevent relapse after transplant” that is pending. J.H. reports grants and personal fees from BMS during the conduct of the study and a patent “Method to prevent relapse after transplant” that is pending. L.K. is on the scientific advisory board for HiFiBio; reports research funding from Kymab Limited, Magenta Therapeutics, BlueBird Bio, and Regeneron Pharmaceuticals; reports consulting fees from Equillium, FortySeven Inc., Novartis Inc., EMD Serono, Gillead Sciences, and Takeda Pharmaceuticals; reports grants and personal fees from BMS, managed under an agreement with Harvard Medical School, during the conduct of the study and outside the submitted work; and has a patent “Method to prevent relapse after transplant” that is pending and a patent “Method to prevent GVHD after transplant” with royalties paid. The remaining authors declare no competing financial interests.
Correspondence: Elizabeth O. Stenger, Aflac Cancer and Blood Disorders Center, Children's Healthcare of Atlanta, Emory University, 1405 Clifton Rd NE, Atlanta, GA 30322; e-mail: estenge@emory.edu.
References
Author notes
Deidentified individual participant data from this clinical trial will be made available, upon request, 3 months after publication and for a period of up to 5 years.
Data are available on request from the corresponding author, Elizabeth O. Stenger (estenge@emory.edu).
The study protocol is included as a data supplement available with the online version of this article.
The full-text version of this article contains a data supplement.