Key Points
Multiple treatment approaches exist for HL, with similar and excellent efficacy.
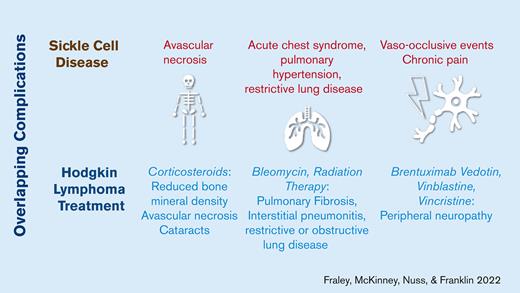
Oncologists should consider a patient’s comorbid conditions and related complications when selecting a treatment regimen to minimize the acute and late effects of therapy.
Abstract
Advances in treatment have reduced mortality from Hodgkin lymphoma; therefore, greater attention should be focused on minimizing the late effects. A variety of risk-adapted treatment regimens exist that prioritize disease presentation but not patient-specific comorbidities. Herein, we describe a patient with sickle cell disease diagnosed with Hodgkin lymphoma and the considerations made in treatment planning to minimize therapy-related acute toxicity and late effects that overlap with the patient’s preexisting sickle cell disease complications.
Introduction
Hodgkin lymphoma (HL) is among the most curable childhood cancers with 90% to 95% cure rates.1 A wide variety of regimens with similar excellent survival rates exist. Therapy intensity varies and is chosen on a risk-adapted basis with attention to stage, B symptoms, bulk, and extranodal involvement. Here, we report on a patient with newly diagnosed HL and comorbid sickle cell disease (SCD) wherein the greatest consideration given to regimen selection was to minimize morbidity and late effects in the setting of her comorbid SCD and related complications. Patients with SCD have more than a threefold risk of developing HL, and the outcomes in this unique population are understudied.2 Given the increased frequency with which patients with SCD are diagnosed with hematologic malignancies,2,3 and the advent of cellular therapies to cure SCD,4 we aimed to highlight disease-specific side effects and toxicities of chemotherapy experienced in this population.
Case description
A 17-year-old female with HbSβ+ thalassemia SCD presented for follow-up after hospitalization for acute chest syndrome (ACS). Her history included 2 additional episodes of ACS, 1 parvovirus-induced aplastic crisis, vaso-occlusive events (VOE), splenic sequestration, prematurity, and intubation at 2 weeks of life for respiratory syncytial virus infection. Her baseline hemoglobin was 12.9 g/dL and she had 4 prior hospitalizations.
Chest radiograph revealed mediastinal lymphadenopathy and laboratory studies revealed lymphopenia and elevated liver enzyme levels. Computed tomography (CT) of the neck, chest, abdomen, and pelvis revealed lymphadenopathy in the right supraclavicular, mediastinal, hilar, mammary chain, and axillary lymph nodes. Excisional biopsy of the right supraclavicular lymph node was positive for CD30, PAX5, and CD15 but negative for CD45, CD20, BCL6, and EBER, consistent with classical HL, mixed cellularity type.
Positron emission tomography (PET)-CT confirmed fluorodeoxyglucose-avid supradiaphragmatic lymphadenopathy and nonspecific uptake in the liver, spleen, shoulders, and iliac wings. Uptake in the shoulders was consistent with avascular necrosis (AVN), although uptake in the iliac wings raised concerns regarding marrow infiltration. The bone marrow biopsy results were negative for malignancy. Ultimately, the patient was diagnosed with Stage IIA HL, limited stage unfavorable based on 4 nodal sites and albumin of 2.4 g/dL.5
Given her underlying SCD, history of ACS, and AVN, our aim was to select a therapy that minimized compounding toxicities and we ultimately decided to forego traditional risk-adapted therapy and treat this limited stage patient with an approach usually reserved for advanced stage disease to achieve this end. Regimens considered are outlined in Table 1 and included Children’s Oncology Group AHOD1822 low risk group with doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD),7 and GPOH-HD-2002 treatment group 1 (vincristine, etoposide, prednisone, and doxorubicin).6 Both options were suboptimal because the former included bleomycin and the latter included corticosteroids and radiation therapy (RT) if the patient had not achieved a complete response (CR) after 2 cycles (which occurs in approximately 68% of patients).6 Pulmonary toxicity is a well-described late effect of both bleomycin and RT, with rates of pulmonary fibrosis as high as 10% for patients treated with bleomycin and 3.5% for patients treated with RT.10,11 Although the patient had normal pulmonary function testing, diffusion capacity for carbon monoxide, and echocardiogram, we sought to avoid pulmonary toxic therapies given her history and the high risk of morbidity and mortality associated with ACS.12,13 In addition, this patient carried an increased risk for stroke given her underlying hemoglobinopathy and we were concerned that RT scatter to the neck would compound this risk in the long term.14,15 Similarly, AVN is a well-described late effect of corticosteroids and there was concern this patient’s risk would be heightened.16
Instead, brentuximab vedotin (Bv), doxorubicin, vinblastine, and dacarbazine (A+AVD) was selected, as investigated in the ECHELON-1 trial for adults with stage III/IV HL.17 When comparing 6 cycles of A+AVD to ABVD, the 5 year progression free survival was 82.2% vs 75.3% (P = .0017). Of the 9 patients who did not achieve CR, 7 received salvage chemotherapy and the remaining 2 received RT. Rates of pulmonary toxicity were lower in the A+AVD group than in the ABVD group (2% vs 7%). However, the rates of peripheral neuropathy were higher with A+AVD given its known association with Bv (67% compared to 43%).9 Ultimately, we felt that the theoretical risk of acute and late pulmonary toxicity would be minimized using the A+AVD approach, as investigated in the ECHELON-1 trial, and obtained the patient and her mother’s verbal consent to treat with A+AVD. We excluded granulocyte colony stimulating factor (G-CSF) despite its inclusion in the investigational arm given its propensity to cause severe or even fatal crises in patients with SCD;18 she experienced mild delays in hematopoietic recovery in 2 out of 6 cycles.
The treatment course was complicated by VOE in 4 of 6 cycles (1 precipitated by coronavirus disease 2019 [COVID-19]), requiring inpatient admission lasting 7 to 17 days. The patient required a maximum of 2 liters oxygen during the COVID-19 infection. VOE were thought to be precipitated by increased red cell sickling from nausea, leading to dehydration and acidosis, and chemotherapy-induced generation of reactive oxygen species. The patient required 9 red blood cell transfusions, all of which were administered as treatment for refractory VOE, not myelosuppression. The patient’s pain was acute, severe, and in the proximal extremities, most consistent with VOE, although neuropathic pain from the Bv may have played a role as well.
Methods
This case was written retrospectively using chart review. The discussion was guided by a review of the literature using a PubMed search using the following medical subject headings and keywords: “sickle cell anemia,” “hemoglobin S disease,” “sickle cell disorder,” “sickling disorder due to hemoglobin S,” “HbS disease,” “SCD” together with “neoplasm,” “neoplasia,” “tumor,” “cancer,” “malignancy,” “malignant,” “malignant neoplasm,” “Hodgkin disease,” “Hodgkin(s) granuloma,” “malignant lymphogranuloma(s),” “HL,” “malignant granuloma(s),” “nodular lymphocyte predominant HL,” “nodular sclerosing HL,” “lymphocyte rich cHL,” “mixed cellularity HL,” or “lymphocyte depletion HL” performed with and without pediatric age range filters.
Results and discussion
Underlying SCD can make the diagnosis and treatment of malignancy challenging. First, this patient’s atypical fluorodeoxyglucose-avidity on PET-CT was difficult to interpret and there was little literature to guide interpretation; PET-CT in SCD has primarily been used to characterize cerebral vasculopathy, ACS and osteomyelitis.19-22
To guide our treatment decisions and anticipate complications given the concern for pulmonary toxicity, we performed the aforementioned literature search and found population-level retrospective cohort studies and case reports suggesting that hematologic malignancies occur at higher rates in patients with SCD. Epidemiological studies from the United Kingdom and California suggest that patients with SCD have more than a threefold risk of developing HL than the general population.2,3 Importantly, these data do not show an increased risk for malignancy following the Food and Drug Administration approval of hydroxyurea (HU) in 1998.3 Notably, these population based studies estimated malignancy rates, but did not provide data on treatment outcomes in this unique population.
Case reports of SCD and cancer were also reviewed to examine therapeutic choices and treatment outcomes. Swede et al examined adverse events experienced by children and adults with SCD or sickle cell trait diagnosed with malignancy by synthesizing relevant case reports.23 The toxicities experienced were not unique to SCD but instead were adverse events commonly experienced by patients treated for cancer (eg, delayed methotrexate clearance).23 Case reports describing treatment and complications among patients diagnosed with cooccurring SCD and HL are described in Table 2. Two case reports described treatment with ABVD and RT, with 1 case complicated by asymptomatic hemolytic anemia.24,25 Other treatment approaches have been used, including treatment with cyclophosphamide, vincristine, procarbazine, and prednisone (COPP); and vinblastine, bleomycin, etoposide, and prednisone (VBVP) plus RT.26-28 Complications in these cases included VOE, fever, bacteremia, and iron overload (Table 2). Interestingly, no cases reported acute pulmonary toxicities such as ACS, despite the inclusion of pulmonary toxic therapies; however, it is noteworthy that patients were not followed longitudinally to adequately describe the late effects or sequelae of SCD. Ultimately, our decision to treat a patient in limited stage with A+AVD, a therapy normally reserved for patients in advanced stage, was guided by a desire to avoid the theoretical risks of pulmonary toxicity and exacerbation of AVN. These risks are theoretical because malignancy outcomes in the population with SCD are poorly studied. Although this discussion may prove instructive in weighing the risks and benefits of various regimens available for the treatment of HL, oncologists and families should keep in mind our strategy to treat HL was not standard and may be viewed as “over treating.”
After 2 cycles of chemotherapy, PET-CT showed a Deauville score of 3, indicating CR.29 PET-CT after 6 cycles, demonstrated further improvement with a Deauville score of 1. The patient remained in CR 18 months after therapy, but magnetic resonance imaging of the hip demonstrated AVN with unilateral subchondral collapse. In conclusion, the A+AVD regimen was efficacious in allowing for CR while minimizing pulmonary toxicity; however, hematologists/oncologists should be prepared for the possibility of VOE.
Acknowledgment
The authors thank the patient for allowing us to write this interesting case report.
Authorship
Contribution: C.E.F. wrote the report; and A.R.K.F., C.M., and R.N. assisted in editing the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Claire E. Fraley, University of Colorado Anschutz Medical Campus, 13123 East 16th Ave, Aurora, CO 80045; e-mail: claire.fraley@childrenscolorado.org.
References
Author notes
Data are available on request from the corresponding author, Claire E. Fraley (claire.fraley@childrenscolorado.org).