Key Points
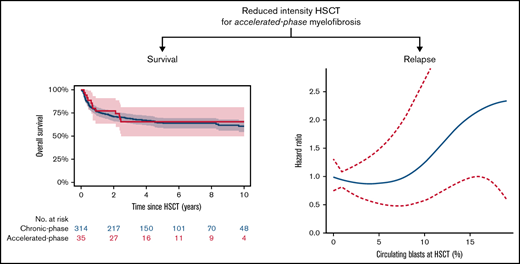
Results of this first report in accelerated-phase myelofibrosis may encourage clinicians to refer these patients for curative treatment.
Accelerated-phase myelofibrosis without prior cytoreduction showed excellent 5-year survival (65%) but higher relapse vs chronic phase.
Abstract
Accelerated-phase myelofibrosis, currently defined by circulating blasts 10% to 19%, usually confers very high risk for progression and poor outcome. The outcome of hematopoietic stem cell transplantation for accelerated-phase myelofibrosis has not been evaluated yet. We analyzed the outcome of 349 clinically and genetically annotated patients with primary or secondary myelofibrosis undergoing reduced intensity transplantation, of whom 35 had accelerated-phase myelofibrosis. In comparison with chronic-phase (<10% blasts) myelofibrosis, median leukocyte counts were higher, more patients had constitutional symptoms, and RAS mutations were detected more frequently in the accelerated-phase group. After a median follow-up of 5.9 years, estimated 5-year overall survival was 65% (95% confidence interval [CI], 49% to 81%) vs 64% (95% CI, 59% to 69%) for the chronic-phase group (P = .91), and median overall survival was not reached. In terms of relapse-free survival, estimated 5-year outcome for the accelerated-phase group was 49% (95% CI, 32% to 67%) vs 55% (95% CI, 50% to 61%) for the chronic-phase group (P = .65). Estimated 5-year nonrelapse mortality was 20% (95% CI, 8% to 33%) for the accelerated-phase group vs 30% (95% CI, 24% to 35%; P = .25) for the chronic-phase group. In terms of relapse, 5-year incidence was 30% (95% CI, 14% to 46%) for the accelerated-phase group vs 15% (95% CI, 11% to 19%) for the chronic-phase group (P = .02). Results were confirmed in multivariable analysis and propensity score matching. In conclusion, reduced intensity transplantation showed excellent survival but higher relapse for accelerated-phase myelofibrosis.
Introduction
Myelofibrosis is a Philadelphia-chromosome–negative myeloproliferative neoplasm with heterogenous clinical presentations and variable outcomes, with survival ranging from months to decades. Diagnostic criteria derive from atypical clonal myeloid proliferation and bone marrow fibrosis, resulting in ineffective hematopoiesis, anemia, increased lactate dehydrogenase, constitutional symptoms, splenomegaly, and leukoerythroblastosis.1 Altered JAK2, MPN, or CALR signaling (driver mutations) represents the major pathophysiologic hallmark of the disease.2
With respect to outcome, blasts from 10% to 19% define an accelerated phase with clearly inferior outcome from myelofibrosis diagnosis,3 challenging treatment considerations, especially because this population has been underrepresented in or even generally excluded from most studies on prognosis or interventions.4,5 In contrast to currently available risk scores using different cutoff points of circulating blasts ranging from ≥1% to ≥3%,6-9 no significant impact of circulating blasts was identified with respect to posttransplant outcome.10 A most recent evaluation in the nontransplant setting showed a more delineated outcome across the spectrum of circulating blasts <10% and marrow blasts.11 Notably, outcome of patients with accelerated-phase myelofibrosis has not been evaluated yet in patients undergoing stem cell transplantation, which is still the only curative treatment option for myelofibrosis but is also associated with relevant treatment-related morbidity and mortality.12
Here, we aimed to specifically characterize patients with accelerated-phase myelofibrosis and compare outcome with chronic-phase myelofibrosis. Next, we aimed to evaluate the role of (circulating and bone marrow) blasts in a homogenous cohort of myelofibrosis patients undergoing reduced intensity stem cell transplantation to facilitate patient counseling with respect to risks and benefits when considering a curative treatment approach.
Methods
Patients and transplants
Patients with primary or secondary myelofibrosis evolving from essential thrombocythemia or polycythemia vera undergoing reduced intensity allogeneic stem cell transplantation until 2018 were included. Myelofibrosis was diagnosed according to standard criteria.13,14 Patients who progressed to acute leukemia at time of transplantation or received cytoreductive therapy (eg, chemotherapy) for blast reduction prior to transplantation were not eligible for this study. All patients were assessed by using immunohistochemistry. Reduced intensity conditioning prior to transplantation was defined by using busulfan-fludarabine (given as 10 mg/kg bodyweight and 150 or 180 mg/m2), fludarabine-melphalan (given as 150 and 140 mg/m2), or 2-Gy total-body irradiation/fludarabine regimen (150 mg/m2).15,16
Clinical and molecular information
Clinical and transplant-specific information and samples for sequencing and cytogenetic analyses were collected prior to transplantation at each center. Prognostic scoring systems were calculated prior to transplantation. Mutations were detected using next-generation sequencing, as previously described.10,17,18 High-risk mutation profile and cytogenetic risk were categorized according to established systems.7,9,19 Cytogenetic reporting was performed according to the International System for Human Cytogenetic Nomenclature criteria, using standardized techniques. All Institutional Review Boards approved of the study, and it was conducted in accordance with the Declaration of Helsinki.
End points and statistical analysis
The primary end point was overall survival, defined as death from any cause. Survival probabilities were estimated by the Kaplan-Meier method, and the log-rank test was used for univariate comparison. Median follow-up was calculated according to the reverse Kaplan-Meier method. Secondary end points were nonrelapse mortality and relapse, treated as competing risks, for which cumulative incidence analysis was used.
Categorical variables were compared with the use of the Fisher’s exact test or the χ2 test, and continuous variables were analyzed using the Kruskal–Wallis or Mann-Whitney test for independent samples; correlations were assessed using the Pearson, Spearman, or Cramer V test, as appropriate.
For multivariable analysis on survival, we used the Cox proportional hazards model to estimate hazard ratios. Backward selection was used, and only significant variables, including blast group variable, remained in the final model. The model with the best Akaike information criterion was selected. For the competing risks framework on nonrelapse mortality and relapse, the Fine and Gray model was used. The proportional hazards assumption was verified using graphical methods. Scaled Schoenfeld residuals and graphical checks proposed by Klein and Moeschberger were performed to find evidence of violations.
Propensity score matching was applied when comparing accelerated-phase and chronic-phase myelofibrosis to account for potential selection bias. Propensity-matched cohorts were created using a greedy caliper algorithm.20 Patient characteristics were matched for diagnosis, age, leukocyte and platelet count, donor relation, and driver mutation genotype. For a continuous effect of blasts, spline function with different knots was used. All tests were two-sided, with the type I error rate fixed at 0.05. All analyses were performed using the statistical software R, version 4.0.3 packages survival, cmprsk, pspline, prodlim, and rms (R Foundation for Statistical Computing, Vienna, Austria).
Results
Patients
Three hundred forty-nine patients with primary (n = 252) or post–essential thrombocythemia/polycythemia vera myelofibrosis (n = 97), evolving from essential thrombocythemia (n = 54) or polycythemia vera (n = 43), from 4 centers receiving reduced-intensity allogeneic stem cell transplantation between 2004 and 2018 were included. Thirty-five patients had accelerated-phase myelofibrosis at time of transplantation. Reduced-intensity conditioning was busulfan/fludarabine (n = 293), melphalan/fludarabine (n = 55), or 2-Gy total-body irradiation/fludarabine (n = 1). Donor source was matched unrelated (n = 174), HLA-identical sibling (n = 89), or mismatch related or unrelated (n = 86). Median time in years between diagnosis and transplantation was 2.2 years for the entire study cohort and 3.2 years for the accelerated-phase group (P = .36).
The median of circulating blasts in the accelerated-phase group was 14% (range, 10% to 19% blasts). The median age at time of transplantation was 58 years (range, 39-72 years), and 37% of patients were female. Diagnosis at time of transplantation was primary myelofibrosis in 60% (n = 21) and secondary myelofibrosis in 40% (n = 14). JAK2 driver mutation genotype was present in 54%, and high molecular risk (presence of ASXL1, EZH2, SRSF2, IDH1/2) was detected in 40%. Most patients were at intermediate-2 or high risk according to current risk stratification.
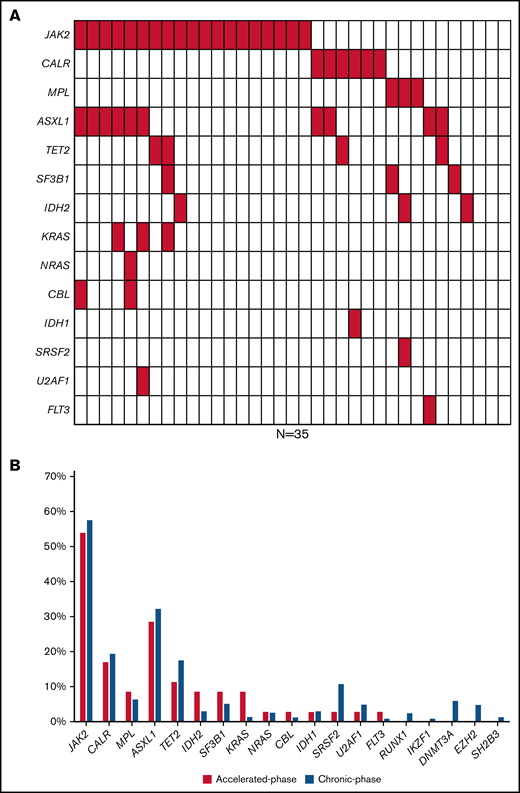
The median absolute hemoglobin levels were slightly lower within the accelerated-phase group (median, 9 g/dL) compared with 9.5 g/dL for chronic phase. White blood cell counts appeared to be higher for the accelerated-phase group (median, 13.6 × 109/L) than the chronic-phase group (P = .08), and constitutional symptoms appeared to be more frequent in the accelerated-phase group (71%; P = .10). Forty-three percent of patients received ruxolitinib before transplantation. Neutrophil engraftment was seen in 92% in both accelerated- and chronic-phase myelofibrosis, within a median of 16 days, respectively. Patients and transplant characteristics are summarized in Table 1, and mutation profile is depicted in Figure 1A-B.
Mutation profile and outcome in accelerated-phase myelofibrosis. (A) Waterfall plot on mutation pattern in 35 patients with accelerated-phase myelofibrosis, of whom 3 patients showed no detectable mutation. (B) Percentage of patients with detected mutation in accelerated-phase (N = 32) and chronic-phase myelofibrosis (N = 307) for a panel of 19 sequenced genes.
Mutation profile and outcome in accelerated-phase myelofibrosis. (A) Waterfall plot on mutation pattern in 35 patients with accelerated-phase myelofibrosis, of whom 3 patients showed no detectable mutation. (B) Percentage of patients with detected mutation in accelerated-phase (N = 32) and chronic-phase myelofibrosis (N = 307) for a panel of 19 sequenced genes.
Outcomes of accelerated-phase myelofibrosis
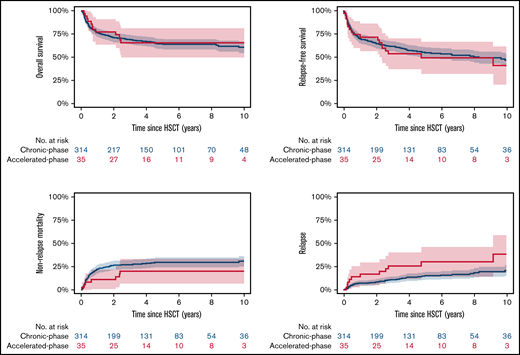
The median follow-up was 5.9 years (95% CI, 2.8-9.0 years). Estimated 5-year overall survival was 65% (95% CI, 49% to 81%), and median overall survival was not reached (Figure 2). Long-term follow-up at 10 years showed an estimated overall survival rate of 68%. In comparison, 5-year overall survival for chronic-phase myelofibrosis (<10% peripheral blasts) was 64% (95% CI, 59% to 69%; P = .91). Other factors on overall survival in the accelerated-phase group were CALR/MPL-unmutated genotype, showing 5-year outcome of 61% vs 89% for presence of CALR/MPL; RAS mutations (n = 5), showing 5-year outcome of 0% vs 76% for absence of RAS mutations; Karnofsky performance status <90%, showing 5-year outcome of 58% vs 78% for performance status 90% to 100%; age at transplantation ≥57 years, showing 5-year outcome of 56% vs 82% for patients <57 years.
Outcome after transplantation of accelerated-phase vs chronic-phase myelofibrosis. Estimated 5-year overall survival was 65% (95% CI, 49% to 81%) for the accelerated-phase group vs 64% (59% to 69%) for the chronic-phase group (P = .91). Relapse-free survival was 49% (32% to 67%) vs 55% (50% to 61%; P = .65). Median relapse-free survival was 4.8 years for the accelerated-phase group. Estimated 5-year nonrelapse mortality was 20% (8% to 33%) vs 30% (24% to 35%; P = .25), and 5-year incidence of relapse was 30% (14% to 46%) vs 15% (11% to 19%; P = .02).
Outcome after transplantation of accelerated-phase vs chronic-phase myelofibrosis. Estimated 5-year overall survival was 65% (95% CI, 49% to 81%) for the accelerated-phase group vs 64% (59% to 69%) for the chronic-phase group (P = .91). Relapse-free survival was 49% (32% to 67%) vs 55% (50% to 61%; P = .65). Median relapse-free survival was 4.8 years for the accelerated-phase group. Estimated 5-year nonrelapse mortality was 20% (8% to 33%) vs 30% (24% to 35%; P = .25), and 5-year incidence of relapse was 30% (14% to 46%) vs 15% (11% to 19%; P = .02).
In terms of relapse-free survival, estimated 5-year outcome for the accelerated-phase group was 49% (95% CI, 32% to 67%), and median relapse-free survival was 4.8 years. In comparison, outcome of chronic-phase myelofibrosis was 55% (95% CI, 50% to 61%; P = .65). Estimated 5-year cumulative incidence of nonrelapse mortality was 20% (95% CI, 8% to 32%), and 5-year cumulative incidence of relapse was 31% (15% to 47%) for the accelerated-phase group compared with 30% (95% CI, 24% to 35%; P = .25) and 15% (95% CI, 11% to 19%; P = .02) for the chronic-phase group. Median time to relapse was 2.4 years for chronic-phase and 1.4 years for accelerated-phase myelofibrosis (P = .46). Death after relapse occurred in an overall 58% of patients with accelerated-phase and 32% of patients with chronic-phase myelofibrosis, and the 3-year postrelapse survival was 50% (95% CI, 23% to 77%) and 61% (95% CI,47% to 75%; P = .28), respectively.
Multivariable analysis and matched comparison
We evaluated the effect of circulating blasts on outcome after adjusting for possible confounders affecting outcome itself and accounting for differences in patient characteristics. Outcome according to blast group was analyzed after including age, mutation status, performance, and blood levels. In terms of overall survival, relapse-free survival, and nonrelapse mortality, no significant association between outcome and blast group was observed; results of other risk factors are shown in Table 2. In contrast, accelerated-phase myelofibrosis was significantly and independently associated with increased risk for relapse, showing a hazard ratio (with the chronic-phase group as reference) of 2.29 (95% CI, 1.15-4.55; P = .02). No other independent risk factors were identified.
We then compared results of this cohort with patients in chronic-phase myelofibrosis in a matched analysis to account for possible selection bias. In terms of overall survival, no significant association of outcome and blast group was seen, showing a hazard ratio (with chronic-phase as reference) of 0.88 (95% CI, 0.40-1.94; P = .76) for the accelerated-phase group. For nonrelapse mortality, no significant difference was seen according to blast group, showing a hazard ratio of 0.54 (95% CI, 0.22-1.34; P = .18) for the accelerated-phase group. In terms of cumulative incidence of relapse, the accelerated-phase group appeared to be associated with increased risk for relapse, showing a hazard ratio of 2.34 (0.84-6.55; P = .11). Relapse-related death appeared to be increased in the matched comparison, showing absolute rates of 58% for the accelerated-phase and 10% for the chronic-phase group (P = .03). Survival curves for matched comparison are depicted in the supplement.
The role of circulating blasts
We next aimed to evaluate the whole spectrum of circulating blasts as continuous variable and its association with phenotype, genotype, and outcomes. The median count in the entire cohort was 1% (range, 0% to 19%). In terms of phenotype, higher counts of circulating blasts correlated with lower hemoglobin levels (P = .04), higher white blood cell counts (P = .07), and higher grade of marrow fibrosis (P = .03). Increased circulating blasts were associated with the presence of constitutional symptoms at time of transplantation (P = .04). In terms of genotype, increasing circulating blasts were associated with presence of RAS mutations (P = .05). No other association between blasts and specific mutations was identified, and no correlation of circulating blasts and number of mutations was identified (P = .54).
Taking circulating blasts as continuous variable, regression analysis on overall survival, relapse-free survival, and nonrelapse mortality showed no significant effect of increasing blasts, with a hazard ratio of 1.00 (95% CI, 0.97-1.05; P = .66), 1.01 (95% CI, 0.98-1.05; P = .58), and 0.99 (95% CI, 0.94-1.03; P = .53), respectively. Stratifying the chronic-phase group according to presence of 0%, 1% to 4%, and 5% to 9% showed no difference in outcome with respect to overall survival, relapse-free survival, nonrelapse mortality. Estimated 5-year overall survival was 66% (95% CI, 58% to 73%) for the 0% group, 62% (95% CI, 53% to 71%) for the 1% to 4% group, and 66% (95% CI, 50% to 81%) for the 5% to 9% group. The 10-year, long-term follow-up showed survival rates of 64% for the 0% group, 58% for the 1% to 4% group, and 66% for the 5% to 9% group.
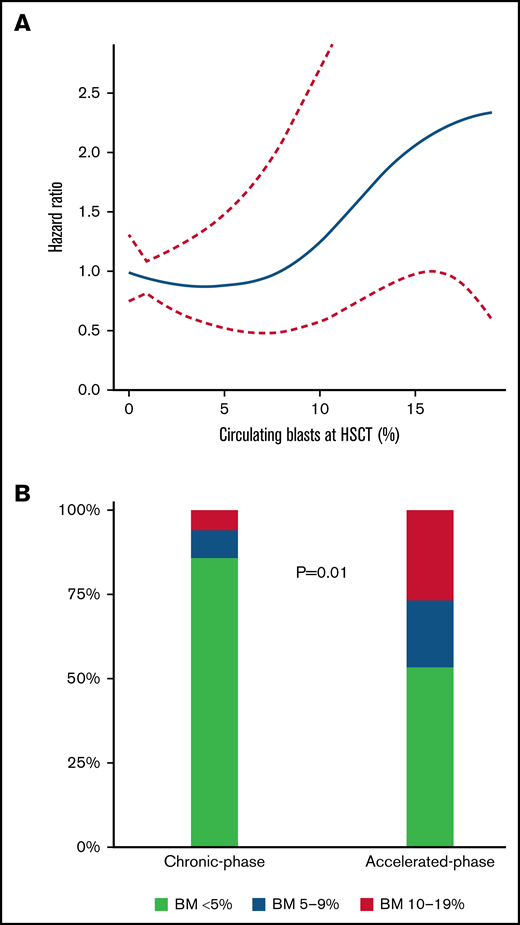
In contrast, in terms of relapse incidence, increase in circulating blasts appeared to be associated with increased risk for relapse in regression analysis, showing a hazard ratio of 1.05 (95% CI, 0.99-1.11; P = .08). No difference according to different blast groups in chronic-phase myelofibrosis was identified. We then aimed to further dissect the effect on relapse by applying spline analysis, identifying increasing risk for >7% circulating blasts and the strongest increased risk for relapse for ≥10% circulating blasts (Figure 3A).
Association of circulating blasts with survival and distribution of bone marrow blasts. (A) Spline analysis of association of circulating blasts and hazard for death with 95% CI, showing increasing risk >7% circulating blasts and an exponential increase ≥10% circulating blasts. (B) Distribution of bone marrow (BM) blasts in chronic-phase vs accelerated-phase myelofibrosis. More patients in the accelerated-phase group had 5% to 9% or 10% to 19% bone marrow blasts before transplantation (P = .01). Distribution according to <5%, 5% to 9%, and 10% to 19% for accelerated-phase vs chronic-phase was 53% vs 86%, 20% vs 9%, and 27% vs 6%, respectively.
Association of circulating blasts with survival and distribution of bone marrow blasts. (A) Spline analysis of association of circulating blasts and hazard for death with 95% CI, showing increasing risk >7% circulating blasts and an exponential increase ≥10% circulating blasts. (B) Distribution of bone marrow (BM) blasts in chronic-phase vs accelerated-phase myelofibrosis. More patients in the accelerated-phase group had 5% to 9% or 10% to 19% bone marrow blasts before transplantation (P = .01). Distribution according to <5%, 5% to 9%, and 10% to 19% for accelerated-phase vs chronic-phase was 53% vs 86%, 20% vs 9%, and 27% vs 6%, respectively.
The role of bone marrow blasts
Last, we conducted a subanalysis to identify certain interactions by the source from which blasts were measured: bone marrow or peripheral blasts. Given that bone marrow biopsies in myelofibrosis represent a challenge to reliable measurements due to often dry aspirations, patient numbers with adequate reports of bone marrow blasts before transplantation were expected to be significantly lower. We identified 86 patients who had adequate information on bone marrow blasts. The median number of bone marrow blasts was 2% (range, 0% to 16%). Stratified by <5%, 5% to 9%, and 10% to 19% bone marrow blasts, the distribution in these 86 patients was 79% (n = 68), 13% (n = 10), and 9% (n = 8), respectively. Sixteen patients in the accelerated-phase and 70 patients in the chronic-phase group had available information. More patients in the accelerated-phase group had 5% to 9% or 10% to 19% bone marrow blasts before transplantation (P = .01; Figure 3B), and in analysis of bone marrow and circulating blasts as continuous measures, a significant correlation was identified (P = .001), with a Pearson index of 0.346.
With respect to outcome in all 86 patients, 5-year overall survival according to the 3 bone marrow blast groups was 78% (95% CI, 67% to 89%) for the <5% group, 60% (95% CI, 30% to 90%) for the 5% to 9% group, and 75% (95% CI, 45% to 100%) for the 10% to 19% group (P = .29). Estimated 5-year relapse-free survival, nonrelapse mortality, and cumulative incidence of relapse were 61%, 14%, and 25% for the <5% group, 60%, 20%, and 20% for the 5% to 9% group, and 63%, 0%, and 38% for the 10% to 19% group, respectively.
Discussion
The provisionally defined subgroup of accelerated-phase myelofibrosis used a 10% blast cutoff arbitrarily based on limited retrospective data.21 Some studies suggest that accelerated-phase myelofibrosis should be treated more aggressively, for example, including hypomethylating agents,11,22,23 aiming to delay the time to leukemic transformation, and implementing curative therapies (stem cell transplantation) in fit patients.
This is the first study to evaluate outcome for accelerated-phase myelofibrosis undergoing curative treatment with reduced-intensity allogeneic stem cell transplantation. First, we identified excellent survival in this cohort, which was similar compared with patients having chronic-phase myelofibrosis (<10% circulating blasts), with median overall survival not reached after long-term follow-up of >10 years. Second, further exploration of circulating blasts as a continuum showed no impact on survival but increased risk for relapse, particularly for patients with ≥10% circulating blasts. Third, increased bone marrow blasts appeared to be associated with increased circulating blasts and did not affect survival.
Notably, the overall outcome of accelerated-phase myelofibrosis in our study appeared to be markedly better compared with current reports of nontransplanted patients, in whom 5-year overall survival was <30% and significantly worse for patients who did not respond to previous therapy, including ruxolitinib.11,23-25 While such indirect comparisons of small numbers of patients should be interpreted with caution, our results clearly support timely evaluation of these patients for the possibility of receiving curative treatment.
Together with current risk stratification tools, our characterization of patients with accelerated-phase myelofibrosis can facilitate patient identification. In line with a most recent evaluation in the ruxolitinib era and nontransplant setting,11 the accelerated-phase group in our cohort showed higher leukocyte counts, more frequently had constitutional symptoms prior to transplantation, and appeared to have lower hemoglobin levels. Nonetheless, hemoglobin was not associated with outcome; in multivariable analyses adjusting for various clinical-molecular features, including leukocytes and constitutional symptoms, no significant difference between accelerated-phase and chronic-phase groups was identified with respect to survival and nonrelapse mortality.
The characteristics of the full spectrum of circulating blasts are also not well defined yet. A recent evaluation in a large population concluded that both circulating and marrow blasts ≥5% appeared to be associated with unfavorable-risk disease and suggested even overlap with currently established accelerated phase.11 Here, we showed similar outcome of various circulating blasts groups (0% vs 1% to 4% vs 5% to 9%). Moreover, circulating blasts correlated with bone marrow blasts, whereas subanalysis of the latter also showed no significant impact on survival while number of patients with sufficient information on bone marrow blasts was small, generally owing to onset of high fibrosis grade in patients referred for transplantation.15
Previous studies on genomic integrity of myeloproliferative neoplasms in chronic phase and during disease progression showed that aberrations of chromosomes 1q and 9p were associated with accelerated phase.26 In our study, no differences were found comparing blast groups according to cytogenetics, driver mutation genotype, or currently defined high-risk mutations. Because previous analyses specifically in patients undergoing transplantation found no association of high molecular risk with survival,10,27 we further evaluated distribution of the transplant-specific risk mutation in ASXL1 according to blast group. Again, no significant difference was seen, showing 29% in the accelerated-phase group and 32% in the chronic-phase group harboring this mutation. Moreover, an extended exome-sequencing analysis of more than 2000 patients indicated that RAS mutations, among others, had a strong association with accelerated-phase myelofibrosis.28 In line with this, the accelerated-phase group in our study showed higher rates of RAS mutations (N = 5, 14.3%) compared with the chronic-phase group (N = 19, 6.5%). Furthermore, another small study suggested that for patients with progressive disease, basophilia as well as a CALR-mutated genotype may be found more frequently.29 In our study, however, information on differential blood levels was not available in all patients with no difference was found for CALR mutation rates.
Furthermore, similarities in clinical-molecular profiles can be found between accelerated-phase and blast-phase myelofibrosis (≥20% blasts) given that accelerated phase precedes blast phase in most patients.21 Simultaneously, marked differences from that of both de novo acute myeloid leukemia and chronic-phase myelofibrosis exist, resembling the complex landscape with respect to treatment decisions, timing, and clinical trial inclusions as that for myelodysplastic syndromes.30 A recent retrospective multicenter study investigated combination therapy with venetoclax and hypomethylating agents (azacytidine or decitabine) in 32 patients with blast-phase myelofibrosis, either up front or after failing another induction.31 Complete remission was achieved in 44% of patients, especially in the absence of RAS mutations. In comparison with historical controls only treated with hypomethylating agents, complete remission rate and median survival appeared to be higher for combination therapy (8 vs 5.5 months). In this analysis, we only included patients with accelerated-phase myelofibrosis without cytoreductive pretreatment to avoid selection bias. However, in line with these and other results, frequencies of RAS mutations appeared to be higher compared with patients with chronic phase, and overall survival appeared to be lower in cases of accelerated-phase myelofibrosis harboring RAS mutations (median, 0.7 years vs not reached).32,33 These results need to be interpreted with caution due to the small sample size of only 5 patients with RAS mutations in accelerated-phase myelofibrosis. Strategies to reduce disease burden before (including novel approaches of venetoclax or hypomethylating agents) or after transplantation as preemptive or prophylactic approaches (including donor lymphocyte infusion) may be explored specifically in this cohort to further reduce risk for relapse.34,35 Postrelapse therapy was out of scope of the present analysis, but patients were censored for whom application of second transplant or lymphocyte infusions was identified. Interestingly, more patients in chronic phase received donor lymphocyte infusions (17% vs 6%). Updated analysis on the value of donor lymphocyte infusions is ongoing.33,34
In terms of pretreatment with ruxolitinib, multivariate analysis of a recent study on outcome of >500 patients with myelofibrosis showed that patients pretreated with ruxolitinib with ongoing spleen response at time of transplantation had a significantly lower risk of relapse (8% vs 19%) and better 2-year event-free survival (69% vs 54%) compared with patients without pretreatment.36 In our cohort, 43% of patients with accelerated phase and 33% of patients with chronic phase received ruxolitinib before transplantation, and outcome for patients who received ruxolitinib pretreatment was similar with respect to overall survival as well as relapse incidence, whereas response data to ruxolitinib were not systematically available for this analysis. Moreover, no significant difference in 5-year nonrelapse mortality and relapse incidence was seen for ruxolitinib (25% and 18%) or no ruxolitinib pretreatment (31% and 16%), respectively.
We acknowledge several shortcomings that are mainly due to the retrospective nature of our study. This may include potential selection bias of fit patients. We carefully aimed to control for such bias by applying multivariable adjustments and matched comparisons, showing similar results. However, such analysis is also prone to biases; therefore, selection bias cannot be fully ruled out in the present study. This may be further suggested by differences in nonsignificant results in univariate and significant results for increased relapse for accelerated phase in multivariate analysis, indicating selection effect for the end point of relapse. This is the first report of patients with accelerated-phase myelofibrosis, and our results in only 35 patients need to be reevaluated in larger studies. Data on spleen size were not available in most patients, and patients who received splenectomy before transplantation did not differ between both groups (11%). More stringent spleen size assessment and documentation are imperative for future studies. Another limitation might have been introduced by a center effect with difference in existing treatment (including conditioning intensity) or diagnostic approaches. Studies comparing reduced intensity with myeloablative conditioning suggested similar nonrelapse mortality but slightly higher relapse incidence with reduced intensity conditioning (23% at 5 years).37 However, overall prognosis with respect to survival was similar for both conditioning intensities.10,37,38 To minimize this bias, we limited our cohort to patients undergoing reduced-intensity stem cell transplantation (84% busulfan-fludarabine, 15% fludarabine-melphalan, 1% total-body irradiation/fludarabine), finding no differences in outcome between center cohorts. Furthermore, although nonrelapse mortality rates of 30% after 5 years require adequate and careful patient counseling to balance risk and benefits of each patient with respect to curative treatment, by taking transplant-specific risk factors into account, our results compare favorably with most reported rates of nonrelapse mortality, with no significant difference noted between reduced-intensity and myeloablative conditioning.37 In our study, all samples were gathered before start of conditioning, and most samples were analyzed centrally, as previously described.17,39
In conclusion, reduced-intensity stem cell transplantation showed excellent outcome for accelerated-phase myelofibrosis. Whether novel agents aimed at blast reduction prior to stem cell transplantation will reduce the risk of relapse should be investigated in clinical studies. The results presented here may facilitate offering these patients evaluation for curative treatment together with current risk stratification tools although close screening for relapse will be needed.
Authorship
Contribution: N.G. and N.K. designed the study, collected and analyzed data, interpreted analyses, and wrote the first draft of the manuscript; M.D., V.P., M.R., and B.L.S. collected data; A.B. and V.P. analyzed samples; C.W., R.B.S., T.S., M.D., V.P., F.T., M.R., H.C.R., F.A., M.H., and B.L.S. interpreted analyses and wrote the paper; and B.C. analyzed samples.
Conflict-of-interest statement: H.C.R. received consulting and lecture fees from AbbVie, AstraZeneca, Vertex, and Merck, received research funding from Gilead Pharmaceuticals, and is a co-founder of CDL Therapeutics GmbH. The remaining authors declare no competing financial interests.
Correspondence: Nicolaus Kröger, Department of Stem Cell Transplantation, University Medical Center Hamburg-Eppendorf, Martinistr 52, 20246 Hamburg, Germany; e-mail: nkroeger@uke.uni-hamburg.de.
References
Author notes
Requests for data sharing may be submitted to Nicolaus Kröger (nkroeger@uke.uni-hamburg.de).
The full-text version of this article contains a data supplement.