Key Points
An incidental histologic diagnosis of DLBCL was identified during temporary interruption of ibrutinib treatment in patients with CLL.
In contrast to an aggressive clinical course typical of Richter transformation, these patients responded to reinitiation of ibrutinib alone.
Introduction
Ibrutinib, a Bruton tyrosine kinase inhibitor approved for treatment of patients with chronic lymphocytic leukemia (CLL), is administered as continuous therapy until unacceptable toxicity or disease progression. However, temporary interruptions in treatment are common, often due to surgical procedures or toxicities.1-4 Although studies evaluating the impact of drug interruption on long-term outcomes have been reported,1,5,6 information pertaining to the immediate clinical consequences associated with temporary interruption of ibrutinib is lacking. Here, we describe 3 patients who were incidentally discovered to have evidence of Richter transformation with diffuse large B-cell lymphoma (DLBCL) histology in association with temporary interruption of ibrutinib.
Methods
Electronic medical records were reviewed for patient and CLL disease characteristics, treatment, follow-up, and pathological findings. Subsequent pathology review was performed by expert hematopathologists (P.L., E.D.M., and R.N.M.). One additional expert hematopathologist performed a central, independent, and blinded review of all cases. Laboratory method details are available in the supplemental Methods.
Results and discussion
Case 1
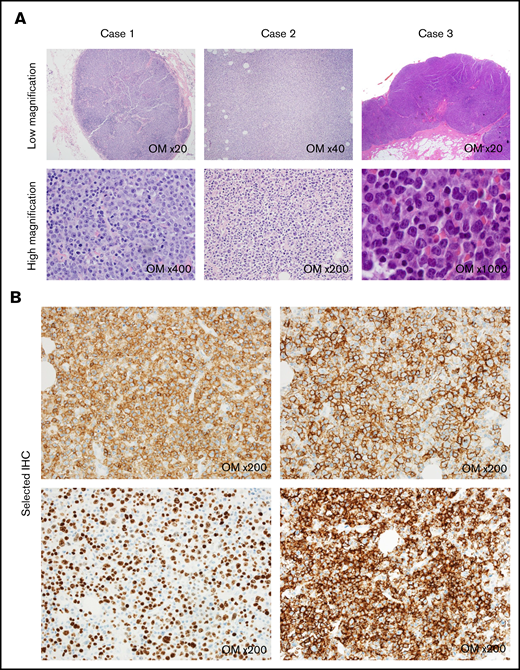
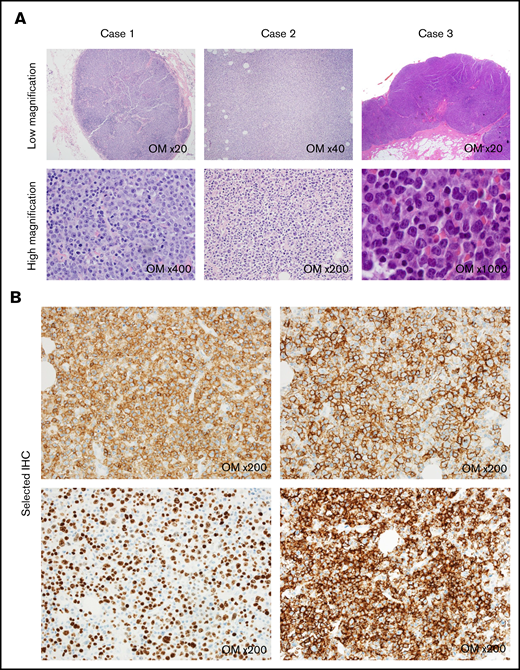
A 73-year-old man with relapsed CLL was on treatment with ibrutinib for 17 months (see Table 17 for a list of patient characteristics) when he was found to have a sigmoid colon mass on routine colonoscopy. In anticipation for sigmoidectomy, ibrutinib was held 1 week before surgery, as per package insert.8 Pathology from the colon confirmed adenocarcinoma; regional lymph nodes resected during surgery were negative for adenocarcinoma. Unexpectedly, the lymph nodes demonstrated involvement by DLBCL with a non–germinal center B-cell phenotype by Hans algorithm9 arising in the background of CLL, consistent with Richter transformation (Figure 1A). Results of fluorescence in situ hybridization (FISH) for MYC rearrangement were negative. The neoplastic large cells expressed programmed death-1 by immunohistochemistry (90%), suggesting that the DLBCL was clonally related to the underlying CLL.10 His postoperative course was complicated by fatigue and fever with no infectious etiology identified. Ibrutinib was restarted 7 days postoperatively. A 18Ffluorodeoxyglucose positron emission tomography (PET) scan performed 1 month after resumption of ibrutinib revealed no abnormalities. Results of a bone marrow biopsy and another PET scan 2 months later were negative for Richter transformation. The patient developed gradually progressive CLL 6 months after sigmoidectomy and was treated with venetoclax and rituximab. The patient remains without any further evidence of Richter transformation with 2.5 years of follow-up beyond the initial finding of DLBCL.
Representative hematopathology findings of incidentally discovered Richter transformation. (A) Images of hematoxylin and eosin–stained slides for each case. Original magnification (OM) is listed in each panel. (B) Immunohistochemistry (IHC) demonstrating CD5-positive (top left panel) and CD23-positive (top right panel) large atypical lymphocytes, as well as a Ki-67 proliferation index of 80% to 90% (bottom left panel) and strongly positive programmed death 1 staining (bottom right panel) in case 2.
Representative hematopathology findings of incidentally discovered Richter transformation. (A) Images of hematoxylin and eosin–stained slides for each case. Original magnification (OM) is listed in each panel. (B) Immunohistochemistry (IHC) demonstrating CD5-positive (top left panel) and CD23-positive (top right panel) large atypical lymphocytes, as well as a Ki-67 proliferation index of 80% to 90% (bottom left panel) and strongly positive programmed death 1 staining (bottom right panel) in case 2.
Case 2
A 63-year-old man received ibrutinib for 39 months for relapsed CLL when a colonoscopy evaluating hematochezia revealed rectal adenocarcinoma. He received 5 weeks of neoadjuvant radiation and capecitabine (ibrutinib was continued through this time). After holding ibrutinib for 7 days, rectosigmoid resection was performed. Lymph nodes were negative for adenocarcinoma but unexpectedly demonstrated DLBCL that expressed CD5, CD23, and programmed death 110 (Figure 1 A-B) and had an activated B-cell phenotype by Lymph2CX molecular profiling.11 MYC rearrangement was not detected by FISH. No co-occurring CLL cells were present in the specimen. Ibrutinib was restarted, and the patient did not experience any new constitutional symptoms or laboratory abnormalities. The perioperative course was uncomplicated. He initiated adjuvant chemotherapy and continued concurrent ibrutinib. The patient had progressive CLL 9 months and 26 months following the identification of DLBCL, for which idelalisib and venetoclax were started, respectively. At the most recent follow-up 32 months after the DLBCL diagnosis, the patient has no evidence of recurrent Richter transformation.
Case 3
A 44-year-old man with previously untreated CLL had been on ibrutinib for 14 months when he was scheduled for a thigh lipoma resection. Two days into his preoperative ibrutinib hold, he experienced low-grade fevers, malaise, and swelling in his axilla and groin that quickly resolved after restarting ibrutinib. His surgery was delayed by 2 weeks, and ibrutinib was successfully held for 7 days before his rescheduled surgery without recurrence of symptoms. Intraoperatively, an abnormal-appearing inguinal lymph node was excised. Unexpectedly, the excised lymph node demonstrated DLBCL with a non–germinal center B-cell phenotype on the background of small lymphocytes of co-occurring CLL consistent with Richter transformation (Figure 1A). FISH was negative for MYC rearrangement. He restarted his ibrutinib 1 week after surgery. A PET scan did not show any 18Ffluorodeoxyglucose-avid lymph nodes but showed a 1.4-cm lung nodule with a standardized uptake value of 7.9. The patient underwent a diagnostic wedge resection of this lesion and the histopathology revealed bronchial malignant melanoma. He started adjuvant immunotherapy with ipilimumab and nivolumab for his resected melanoma and continued ibrutinib for CLL. Subsequent blood work and cross-sectional imaging after 7 months of follow-up after his diagnosis of DLBCL have not demonstrated evidence of progression of CLL or recurrent transformation.
Richter transformation of CLL into an aggressive lymphoma occurs in ∼2% to 10% of patients12 and has been described as an early event in ibrutinib-treated patients.13,14 DLBCL is the most common type of Richter transformation and has a poor prognosis with median overall survival of 12 months.15 Outcomes are particularly dismal when occurring on ibrutinib therapy.13,14 In contrast to an aggressive presentation of Richter transformation at the time of disease progression, we describe a unique presentation when ibrutinib is temporarily interrupted in patients who have stable disease at the time of ibrutinib hold. Importantly, the favorable clinical courses of these patients with response to reintroduction of ibrutinib emphasize this as a critical first step in management, as opposed to starting chemoimmunotherapy.
Patients who stop ibrutinib due to progressive disease can experience rapid disease progression before subsequent therapy is started.16 Additionally, in a retrospective analyses of 143 patients treated at Mayo Clinic who interrupted ibrutinib temporarily, 35 patients experienced “disease flare,” manifested by symptoms, laboratory abnormalities, or radiographic findings of progressive disease.3 The patients described in the current series had incidental histopathological examination of lymph nodes for a concomitant malignancy, which allowed us to identify DLBCL as the underlying pathology (see supplemental Figures 1-3 for additional hematopathology images of each case). All patients responded to reintroduction of ibrutinib with no evidence of recurrent DLBCL after 7, 30, and 32 months of follow-up. These findings suggest that the Richter transformation described in this report likely represents an unstable B-cell clone and that sudden release of B-cell receptor signaling inhibition during interruption of ibrutinib therapy may be responsible for this clinical manifestation.
Interestingly, all patients had unmutated immunoglobulin heavy chain genes and TP53 disruption, which are frequently observed with Richter transformation.17 Two of the 3 patients also had trisomy 12, a genomic aberration associated with increased incidence of Richter transformation as well.18 Given this is a small case series, we are unable to draw broad conclusions about which patients might be at risk for developing this complication or if these patients are at a higher risk of progressive disease eventually.
In summary, we provide a novel description of incidentally discovered Richter transformation during ibrutinib hold and an associated transient clinical course with resuming ibrutinib treatment. Given that ∼40% patients on ibrutinib therapy require a temporary hold of ibrutinib during the course of therapy,4 this observation warrants awareness among clinicians and further investigation of the underlying biological mechanisms.
Requests for data sharing should be e-mailed to the corresponding author, Paul J. Hampel (hampel.paul@mayo.edu).
Acknowledgment
The authors thank Paul J. Kurtin for the independent pathology review of the cases included in this study.
Authorship
Contribution: P.J.H., H.-J.J.C., N.J., and S.A.P. designed the study, collected and analyzed data, and wrote the manuscript; T.G.C., W.D., H.A.T., A.F., and W.G.W. cared for patients and critically reviewed the manuscript; M.K., E.D.M., R.N.M., and P.L. collected and analyzed data, performed pathology review, and critically reviewed the manuscript; and all authors approved the manuscript in its final format.
Conflict-of-interest disclosure: W.D. reports research funding has been provided to the institution from Merck and DTRM, and has participated in advisory board meetings of Octapharma and Alexion (she was not personally compensated for her participation). R.N.M. received honorarium from Allergan for participating at 1 advisory board conference. H.A.T. served as a consultant or an advisory board member for Bristol-Myers Squibb, Novartis, Merck & Co., Genentech, and Array and has received commercial research grants from Bristol-Myers Squibb, Merck & Co., Genentech, GlaxoSmithKline, and Celgene. A.F. reports research funding Celgene, Acerta, Beigene. W.G.W. reports grants from AbbVie, GlaxoSmithKline, Novartis, Genentech, Pharmacyclics, Gilead, Acerta, JUNO (Celegene), KITE Pharma (Gilead), Sunesis, Miragen, Oncturnal Therapeutics, LOXO Oncology, Cyclacel, Janssen, and Xencor, and nonfinancial support from AbbVie, Genentech, Pharmacyclics, Gilead, Acerta, JUNO (Celgene), KITE Pharma (Gilead), Sunesis, Oncturnal Therapeutics, LOXO Oncology, and Janssen outside the submitted work. N.J. reports research funding has been provided to the institution from Pharmacyclics, AbbVie, Genentech, AstraZeneca, BMS, Pfizer, ADC Therapeutics, Incyte, Servier, Cellectis, Verastem, Adaptive Biotechnologies, and Precision Biosciences for clinical studies in which N.J. is a principal investigator, and has participated in advisory board meetings and received honoraria from Pharmacyclics, Janssen, AbbVie, Genentech, AstraZeneca, Verastem, Adaptive Biotechnologies, Servier, and Precision Biosciences. S.A.P. reports research funding has been provided to the institution from Pharmacyclics, MorphoSys, Janssen, AstraZeneca, TG Therapeutics, Celgene, AbbVie, and Ascentage Pharma for clinical studies in which S.A.P. is a principal investigator, and has also participated in advisory board meetings of Pharmacyclics, AstraZeneca, Genentech, Gilead, GlaxoSmithKline, Verastem Oncology, and AbbVie (he was not personally compensated for his participation). The remaining authors declare no competing financial interests.
Correspondence: Paul J. Hampel, Division of Hematology, Mayo Clinic, 200 First St SW, Rochester, MN 55905; e-mail: hampel.paul@mayo.edu.
References
Author notes
P.J.H. and H.-J.J.C. contributed equally to this study.
The full-text version of this article contains a data supplement.