Abstract
Acute monoblastic leukemia (acute myeloid leukemia [AML], French-American-British type M5a) with leukemia cutis developed in a patient 6 weeks after the initiation of erythropoietin (EPO) therapy for refractory anemia with ringed sideroblasts. AML disappeared from both marrow and skin after the discontinuation of EPO. Multiparameter flow cytometric analysis of bone marrow cells demonstrated coexpression of the EPO receptor with CD45 and CD13 on the surface of blasts. The incubation of marrow cells with EPO, compared to without, resulted in 1.3- and 1.6-fold increases, respectively, in tritiated thymidine incorporation and bromodeoxyuridine incorporation into CD13+ cells. Clinical and laboratory findings were consistent with the EPO-dependent transformation of myelodysplastic syndrome (MDS) to AML. It is concluded that leukemic transformation in patients with MDS treated with EPO may be EPO-dependent and that management should consist of the discontinuation of EPO followed by observation, if clinically feasible.
Introduction
The myelodysplastic syndromes (MDS) are heterogeneous clonal bone marrow (BM) disorders characterized by ineffective hematopoiesis.1 Anemia develops in 90% of patients. Erythropoietin (EPO) therapy stimulates erythropoiesis in approximately 25% of patients.2,3 Decreased sensitivity of erythroid precursors to EPO at the initial level of signal transduction may contribute to anemia in MDS4; EPO therapy may overcome this decreased sensitivity.
The risk for transformation of MDS to acute myeloid leukemia (AML) correlates with the percentage of BM myeloblasts, cytogenetic abnormalities, and number of cytopenias.5 Marrow blasts may increase, albeit infrequently, in MDS patients receiving granulocyte-monocyte or granulocyte colony-stimulating factor.6-9 Leukemic transformation of MDS is rare during EPO therapy, is seen primarily in patients with refractory anemia with excess blasts or refractory anemia with excess blasts in transformation,3,10,11 and is thought to reflect natural history rather than EPO effect. AML has also developed in patients with end-stage renal failure treated with EPO12 13; the role of EPO in this setting is unknown. We report a patient with clinical and laboratory findings consistent with EPO-dependent transformation of MDS to AML.
Study design
Clinical course
A 66-year-old man was evaluated for mild anemia; BM morphology was diagnostic of MDS; the French-American-British (FAB) type was refractory anemia with ringed sideroblasts (RARS). Two years later stage IIA Hodgkin disease was diagnosed. Hemoglobin level was 9.7 g/dL, white blood cell (WBC) count was 7.6 × 109/L with a normal differential count, and platelet count 145 × 109/L. BM aspirate and biopsy showed dysplastic erythroid hyperplasia with 90% ringed sideroblasts and 1.6% myeloblasts, again consistent with RARS. A B-cell clone expressing CD45, HLADr, CD5, CD19, and λ light chain was detected by multiparameter flow cytometry (MFC), consistent with early chronic lymphocytic leukemia.14 Karyotype was normal. Six courses of Adriamycin, bleomycin, vinblastine, and dacarbazine combination chemotherapy were administered, with clinical and radiologic resolution of Hodgkin disease. Anemia worsened 3 months later, necessitating monthly red blood cell transfusions. WBC and platelet counts remained normal, and BM again showed RARS with a normal karyotype and a B-cell clone by MFC. Serum EPO level was 9.6 mIU/mL. EPO therapy was initiated at a dose of 10 000 IU subcutaneously 3 times per week. Anemia improved, and transfusions were no longer required.
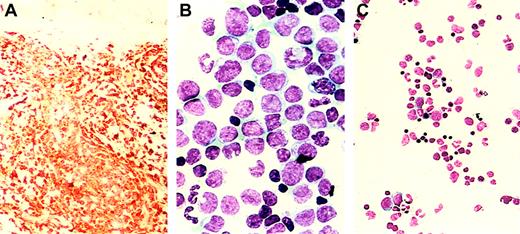
Six weeks after the initiation of EPO therapy, numerous violaceous nodules, each measuring 0.5 to 1 cm, appeared across the patient's back and abdomen. Biopsy specimens showed dermal infiltration by monoblasts staining immunohistochemically for lysozyme (Figure1A), myeloperoxidase, and CD15. Hemoglobin level was 9 g/dL, WBC count was 26.8 × 109/L with 41% neutrophils, 32% lymphocytes, 25% monocytes, 2% basophils, and 0% blasts, and platelet count was 203 × 109/L. The BM was hypercellular, with 45% monoblasts (Figure 1B) staining with α-naphthyl butyrate esterase and expressing CD45, HLADr, CD2, CD4, CD11b, CD11c, CD13, CD14, CD15, and CD33 by MFC with persistence of the B-cell clone. Karyotype was again normal, and MLL gene rearrangement was not detected in 500 interphase cells by fluorescence in situ hybridization with the LSI MLL dual-color rearrangement probe (catalog number 32-190083; Vysis, Downer's Grove, IL). A diagnosis of acute monoblastic leukemia (French-American-British type M5a AML) with leukemia cutis was made, but chemotherapy was not initiated because of comorbid conditions. EPO therapy was discontinued. Skin lesions regressed and disappeared completely by 7 weeks. A BM sample 3 weeks after the discontinuation of EPO showed reversion to MDS, without increased blasts (Figure 1C) and without abnormal myeloid cells by MFC; the B-cell clone persisted. Anemia worsened again, necessitating transfusions. The patient had a fatal myocardial infarction 4 months later; leukemia had not recurred.
Erythropoietin-dependent acute monoblastic leukemia.
Histopathology. Skin biopsy showing infiltration by monoblasts staining with lysozyme (panel A, × 50 magnification) and bone marrow aspirate smear showing acute monoblastic leukemia (panel B, × 200 magnification), both during EPO therapy. Bone marrow aspirate smear showing the absence of leukemia 3 weeks after the discontinuation of EPO therapy (panel C, × 50 magnification).
Erythropoietin-dependent acute monoblastic leukemia.
Histopathology. Skin biopsy showing infiltration by monoblasts staining with lysozyme (panel A, × 50 magnification) and bone marrow aspirate smear showing acute monoblastic leukemia (panel B, × 200 magnification), both during EPO therapy. Bone marrow aspirate smear showing the absence of leukemia 3 weeks after the discontinuation of EPO therapy (panel C, × 50 magnification).
Laboratory studies
Samples.
BM mononuclear cells obtained by Ficoll-Hypaque density centrifugation at presentation of AML, 3 months earlier, and 6 weeks later were cryopreserved in RPMI 1640 medium (Gibco, Grand Island, NY) with 20% fetal calf serum and 20% dimethyl sulfoxide using standard procedures.
EPO receptor expression.
EPO receptor expression was studied by MFC with the rabbit polyclonal antibody EpoR (C-20) (Santa Cruz Biotechnology, Santa Cruz, CA), detected with fluorescein isothiocyanate-conjugated goat anti–rabbit immunoglobulin G (Caltag, Burlingame, CA). The primary antibody was titered using the UT-7/EPO cell line15 provided by Dr Kamatsu (Tochigi, Japan). The EPO receptor was coexpressed with CD45 and CD13 on the surface of blasts, defined by forward versus side scatter characteristics, but not on lymphocytes, defined by forward versus side scatter and absence of CD13 expression. Cells coexpressing the EPO receptor, CD45, and CD13 were detected in samples from all 3 time points, but were most numerous at the presentation of AML (Figure2A).
EPO receptor expression on CD13+ blasts and in vitro proliferation of CD13+ cells in response to EPO.
Upper panels (A) demonstrate gating on blasts defined by forward scatter characteristics (FSC) versus side scatter characteristics (SSC) (left) and coexpression of the EPO receptor with CD45 (center) and CD13 (right) on cells in the gated region. Lower panels (B) demonstrate the incorporation of BrdU into CD13+ cells in the absence (left) and presence (right) of EPO. Increased DNA synthesis is seen in CD13+ cells in the presence of EPO.
EPO receptor expression on CD13+ blasts and in vitro proliferation of CD13+ cells in response to EPO.
Upper panels (A) demonstrate gating on blasts defined by forward scatter characteristics (FSC) versus side scatter characteristics (SSC) (left) and coexpression of the EPO receptor with CD45 (center) and CD13 (right) on cells in the gated region. Lower panels (B) demonstrate the incorporation of BrdU into CD13+ cells in the absence (left) and presence (right) of EPO. Increased DNA synthesis is seen in CD13+ cells in the presence of EPO.
In vitro EPO response.
BM cells cryopreserved before the initiation of EPO therapy were incubated for 4 hours in RPMI 1640 medium supplemented with 10% fetal calf serum, with and without 1 U/mL recombinant EPO (Amgen, Thousand Oaks, CA). DNA synthesis was measured by radiolabeled thymidine ([methyl-3H], 1 μCi [3.7 × 104Bq], 10 minutes) incorporation. In 2 experiments with 5 × 106 cells each, DNA synthesis increased 1.27- and 1.33-fold (mean, 1.3-fold) in the presence of EPO.
To identify the population proliferating in response to EPO, cells incubated for 4 hours with and without EPO were labeled with 10 μM 5-bromo-2-deoxyuridine (BrdU) for 30 minutes then were stained with CD13 antibody and analyzed by MFC.16 Incubation of marrow cells with versus without EPO resulted in a 1.6-fold increase in BrdU incorporation (from 3.3% to 5.2%) into myeloid blasts, defined by forward versus side scatter characteristics and CD13 expression.
Results and discussion
AML developed in our patient during EPO therapy and regressed after its discontinuation. Transformation to acute leukemia was unexpected, given the RARS subtype of MDS, the normal karyotype, and the presence of anemia as the sole cytopenia.5 Adriamycin administered to treat Hodgkin disease could have been leukemogenic, butMLL gene rearrangement, characteristic of topoisomerase II inhibitor-induced AML,17 was not found. The development of AML during EPO therapy and the disappearance of leukemia from BM and skin after the discontinuation of EPO were consistent with EPO-dependent transformation of MDS to AML. In vitro results also support this hypothesis; myeloid blasts expressed the EPO receptor and proliferated in response to EPO. Relatively modest EPO-induced proliferation in vitro is explained by the absence of leukocyte-conditioned medium or costimulatory cytokines in the cultures.18 19 Of note, the B-cell clone detected by MFC might possibly have produced costimulatory factors in vivo.
EPO has been reported to stimulate clonogenic leukemic erythroid progenitors in erythroleukemia20 and leukemic blast colony growth in the presence of phytohemagglutinin-stimulated, leukocyte-conditioned medium in other AML subtypes.18,19EPO receptor expression was found on leukemia cells in 81 of 136 (60%) patients with all French-American-British types of AML, and in vitro proliferation in response to EPO was seen in 16% of patients, all with expression of the receptor.21 Moreover, compared with those without EPO receptor expression, remission duration was shorter in patients whose cells expressed the EPO receptor and proliferated in response to EPO.21
To our knowledge, this is the first demonstration of EPO-dependent leukemic transformation of MDS. EPO is used increasingly in patients with MDS, and close observation for leukemic transformation is warranted. EPO therapy should be discontinued in patients with MDS that progresses to AML, and, if clinically feasible, those patients should be observed for the regression of AML.
Supported in part by shared resources of the Roswell Park Cancer Center Support Grant (P30 CA16056) and by the Leonard S. LoVullo Memorial Fund for Leukemia Research.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Maria R. Baer, Department of Medicine, Leukemia Section, Roswell Park Cancer Institute, Elm and Carlton Sts, Buffalo, NY 14263; e-mail: maria.baer@roswellpark.org.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal