Abstract
Spherocytic red cells with reduced membrane surface area are a feature of hereditary spherocytosis (HS) and some forms of autoimmune hemolytic anemia (AIHA). It is generally assumed that membrane loss in spherocytic red cells occurs during their sojourn in circulation. The structural basis for membrane loss in HS is improper assembly of membrane proteins, whereas in AIHA it is due to partial phagocytosis of circulating red cells by macrophages. A hypothesis was formed that these different mechanisms should lead to temporal differences in surface area loss during red cell genesis and during sojourn in circulation in these 2 spherocytic syndromes. It was proposed that cell surface loss could begin at the reticulocyte stage in HS, whereas surface area loss in AIHA involves only circulating mature red cells. The validity of this hypothesis was established by documenting differences in cellular features of reticulocytes in HS and AIHA. Using a novel technique to quantitate cell surface area, the decreased membrane surface area of both reticulocytes and mature red cells in HS compared with normal cells was documented. In contrast, in AIHA only mature red cells but not reticulocytes exhibited decreased membrane surface area. These data imply that surface area loss in HS, but not in AIHA, is already present at the circulating reticulocyte stage. These findings imply that loss of cell surface area is an early event during genesis of HS red cells and challenge the existing concepts that surface area loss in HS occurs predominantly during the sojourn of mature red cells in circulation.
Introduction
Spherocytic red cells result from a loss of membrane surface area and, consequently, exhibit increased cell sphericity and reduced cellular deformability.1,2Increased splenic sequestration of these indeformable spherocytic red cells results in anemia. Hemolytic anemia characterized by circulating spherocytic red cells can stem from various etiologies, the principal ones being hereditary spherocytosis (HS),3 an inherited disease, and autoimmune hemolytic anemia (AIHA) due to warm antibodies, an acquired disorder.4,5 Although spherocytic red cells in these 2 settings are morphologically indistinguishable, the mechanistic basis for their generation is very different. In HS, mutations in genes coding for various membrane proteins (including ankyrin, band 3, protein 4.2, α- or β-spectrin)6-8 result in the assembly of an intrinsically unstable membrane leading to vesiculation of the lipid bilayer.3 The membrane lipid loss in turn accounts for decreased surface area of spherocytic red cells. In AIHA, the loss of surface area occurs primarily during the interaction of red cells with macrophages in the spleen.5,9 The interaction between red cell membrane-bound immunoglobulin with the Fc receptor of phagocytic cells4,10 leads to partial phagocytosis of the red cell membrane, resulting in reduced cell surface area of the remnant cell that becomes spherocytic.4,5 11Although it has long been known that spherocytosis is a feature of mature red cells in both HS and AIHA, no information is currently available on the cellular characteristics of reticulocytes in these 2 disorders.
The aim of our study was to explore the temporal differences between HS and AIHA regarding the occurrence of surface area loss during red cell genesis and maturation. We propose that cell surface loss can exist in HS at the reticulocyte stage, whereas in AIHA it involves only mature red cells. The validity of this hypothesis rests on documenting differences in cellular features of reticulocytes in HS and AIHA. Using a novel technique12 to quantitate the surface area and volume of both reticulocytes and mature red cells, we documented decreased membrane surface area of both reticulocytes and mature red cells in HS compared with normal cells. Importantly, splenectomy had no effect on the extent of reticulocyte or mature red cell surface area loss in HS. In marked contrast, in AIHA only mature red cells but not reticulocytes exhibited decreased membrane surface area. These data imply that surface area loss in HS, but not in AIHA, is manifested at the circulating reticulocyte stage and challenge the existing concepts that membrane loss in HS occurs predominantly during the sojourn of mature red cells in circulation. Furthermore, we have shown that although the spleen plays a major role in sequestering spherical cells, its contribution to the generation of spherocytic red cells in HS is much less important than previously thought. We also noted that compared with either AIHA or normal reticulocytes, the volume of HS reticulocytes was reduced while cell hemoglobin concentration was increased. These findings further suggest that reticulocyte parameters could be potentially useful in the differential diagnosis of spherocytes of HS and AIHA.
Patients, materials, and methods
Subjects
Our hematology department at hôpital Bicêtre is one of the referral centers for red blood cell diseases in France. Informed consent was obtained from all individuals who participated in this study. None of the patients were transfused during the 3 months prior to their participation in the study. Twenty-five nonsplenectomized and 23 splenectomized patients with HS were studied (39 adults and 9 children; age range, 3-59 years; 21 males and 27 females). A diagnosis of HS was confirmed by documenting the decreased membrane surface area by osmotic gradient ektacytometry and by the analysis of red cell indices from an automated hematology analyzer (Bayer Diagnostics, Puteaux, France). Thirteen patients with untreated AIHA and a positive direct antiglobulin test (age range, 3-71 years; 9 females and 4 males) were also studied. At the time of the study, AIHA in these 13 individuals was not associated with other obvious immune manifestations. IgG autoantibodies were identified in 12 of these individuals, and in the remaining individual, an IgA autoantibody was documented. In 3 of these 13 patients with AIHA, sequential monitoring during steroid therapy was performed. Controls were 37 healthy adults with normal blood counts. We also studied 3 adults with normal blood cell counts who had been previously splenectomized for reasons unrelated to a red blood cell disorder: refractory autoimmune thrombocytopenic purpura (one case) and splenic trauma (2 cases).
Methods
Blood was drawn into ethylenediaminetetraacetic acid (EDTA) vacutainers and stored at 4°C. All the measurements were performed within 24 hours of blood sampling. Red cell morphology on blood smears was evaluated by optical microscopy. Red cell and reticulocyte counts and indices and hemoglobin values were determined using an automated blood cell analyzer (H*3 or Advia 120; Bayer Diagnostics). These 2 automated hematology analyzers provide the mean corpuscular volume and the mean cell hemoglobin concentration of reticulocytes (MCVr and CHCMr, respectively). The MCV and CHCM of mature red cells are either provided directly (Advia 120) or can be calculated (H*3) from the parameters of reticulocytes and total red cells (reticulocytes plus red cells).13 These hematology analyzers provide 2 distinct measures of red cell hemoglobin concentration: CHCM and MCHC. CHCM is derived from measurements of hemoglobin concentration of individual red cells, whereas MCHC is calculated from measured values of hemoglobin and hematocrit. Red cell deformability measurements were performed with an osmotic gradient ektacytometer (Bayer Diagnostics, Tarrytown, NY).14-17
Cell surface area.
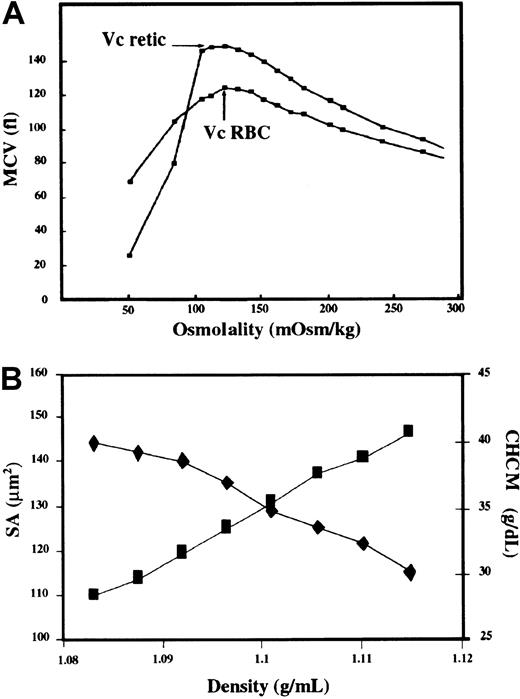
A new strategy that applies a simple geometric model to measure values of critical hemolytic volumes of reticulocytes and red cells was developed to derive the surface area of reticulocytes and red cells.12 Briefly, a series of 16 different solutions of varying osmolalities ranging from 290 and 110 mosm/kg were prepared by adding appropriate amounts of sodium chloride to 10 mM phosphate buffer solution (pH 7.4) containing the sphering agent (Bayer Diagnostics, France) and the reticulocyte-specific dye oxazine 750. Freshly drawn blood samples were diluted (1:1000) in the various osmotic solutions, equilibrated for 30 minutes, and analyzed in duplicate within 2 minutes using the flow cytometry–based hematology analyzer H*3 (Bayer Diagnostics, France). The percentage of reticulocytes in each of the 16 solutions remained the same. Red cell and reticulocyte volumes at different osmolarities were recorded. With decreasing suspending medium osmolality, there is a progressive increase in cell volume until at a defined osmolality the cells begin to hemolyze, resulting in an abrupt decrease in cell volume (Figure1A). The maximal spherical volume is attained just prior to hemolysis. The MCV measured at the osmolality preceding the osmolality where cells begin to lyse is defined as the critical hemolytic volume (Vc). Since Vc represents the maximum spherical volume of the cell for a defined surface area, the cell surface area is calculated as
Critical hemolytic volume, surface area, and red cell hemoglobin concentration of reticulocytes and red cells.
(A) Quantitation of surface area of reticulocytes and red cells in a blood sample. The whole blood sample was diluted 1 to 1000 in a series of 16 solutions with osmolality ranging from 290 to 110 mosm/kg, and the volume of red cells and reticulocytes was measured using an automated hematology analyzer (Bayer Diagnostics, Puteaux, France). As the suspending medium osmolality decreased, cell volume increased until the cells attained their critical hemolytic volume (indicated by the arrows) just prior to cell lysis. The surface area of reticulocytes and mature red cells was derived from their respective critical hemolytic volumes, Vc retic and Vc RBC as outlined in “Patients, materials, and methods.” (B) Surface area (diamonds) and mean cell hemoglobin concentration (CHCM) (squares) as a function of red cell density. As the cell density increased, the surface area decreased and CHCM increased.
Critical hemolytic volume, surface area, and red cell hemoglobin concentration of reticulocytes and red cells.
(A) Quantitation of surface area of reticulocytes and red cells in a blood sample. The whole blood sample was diluted 1 to 1000 in a series of 16 solutions with osmolality ranging from 290 to 110 mosm/kg, and the volume of red cells and reticulocytes was measured using an automated hematology analyzer (Bayer Diagnostics, Puteaux, France). As the suspending medium osmolality decreased, cell volume increased until the cells attained their critical hemolytic volume (indicated by the arrows) just prior to cell lysis. The surface area of reticulocytes and mature red cells was derived from their respective critical hemolytic volumes, Vc retic and Vc RBC as outlined in “Patients, materials, and methods.” (B) Surface area (diamonds) and mean cell hemoglobin concentration (CHCM) (squares) as a function of red cell density. As the cell density increased, the surface area decreased and CHCM increased.
Statistical analysis.
Statistical analysis was performed using the unpaired Studentt test and the nonparametric Mann-Whitney test.
Results
Red cell morphology, hemoglobin values, and reticulocyte counts
Morphologic examination of peripheral blood smears showed that spherocytic red cells are a distinguishing feature of red cell morphology in all patients with either HS or AIHA. In nonsplenectomized patients with HS, the mean hemoglobin value (Hb) was decreased compared with controls (P < .0001), but as previously reported,2 Hb values were either normal or higher than normal in splenectomized patients with HS (Table1). The reticulocyte count was significantly increased in nonsplenectomized patients with HS compared with controls (P < .0001), whereas it was only marginally elevated in splenectomized patients with HS (Table 1). In patients with AIHA, the mean Hb value was significantly decreased (P < .0001), and the reticulocyte count was increased as compared with controls (P < .0001). The magnitude of increase in the reticulocyte counts in patients with AIHA was similar to that seen in nonsplenectomized patients with HS (P = .74).
Hemoglobin value and reticulocyte count (mean value ± SD)
| . | Controls (n = 37) . | Nonsplenectomized HS (n = 25) . | Splenectomized HS (n = 23) . | AIHA (n = 13) . |
|---|---|---|---|---|
| Hb (g/dL) | 13.9 ± 1.0 | 12.2 ± 1.5 | 15.2 ± 1.3 | 11.3 ± 3.2 |
| (range, 11.8-15.8) | (range, 10.0-15.1) | (range, 12.7-18.6) | (range, 6.1-16.2) | |
| Reticulocytes (%) | 1.0 ± 0.3 | 6.7 ± 3.5 | 2.1 ± 1.0 | 7.3 ± 7.2 |
| (range, 0.6-1.9) | (range, 1.6-14.1) | (range, 0.7-4.3) | (range, 0.8-22.9) |
| . | Controls (n = 37) . | Nonsplenectomized HS (n = 25) . | Splenectomized HS (n = 23) . | AIHA (n = 13) . |
|---|---|---|---|---|
| Hb (g/dL) | 13.9 ± 1.0 | 12.2 ± 1.5 | 15.2 ± 1.3 | 11.3 ± 3.2 |
| (range, 11.8-15.8) | (range, 10.0-15.1) | (range, 12.7-18.6) | (range, 6.1-16.2) | |
| Reticulocytes (%) | 1.0 ± 0.3 | 6.7 ± 3.5 | 2.1 ± 1.0 | 7.3 ± 7.2 |
| (range, 0.6-1.9) | (range, 1.6-14.1) | (range, 0.7-4.3) | (range, 0.8-22.9) |
HS indicates hereditary spherocytosis; AIHA indicates autoimmune hemolytic anemia.
Red cell deformability studies
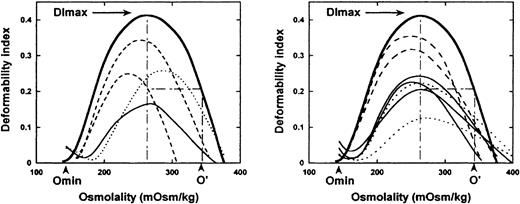
A representative set of osmotic gradient deformability profiles of red cells from patients with HS or AIHA are shown in Figure2. A decrease in DImax value, indicative of decreased red cell surface area, was a distinguishing feature of all HS and AIHA deformability profiles. Consistent with previous data,2 the mean DImax was 0.28 (range 0.18-0.35) for 48 patients with HS compared with the mean DImax of 0.40 for healthy controls (P < .0001). The extent of decrease in surface area was similar in splenectomized and nonsplenectomized patients with HS. DImax values were similarly decreased in patients with AIHA (mean 0.28; range, 0.14-0.36). A shift to the left of O' in the hypertonic region of the deformability profile, reflecting red cell dehydration, was noted in 31 of 48 patients with HS and in 8 of 13 patients with AIHA. A shift to the right of Omin in the hypotonic region of the deformability profile, reflecting a decreased surface-to-volume ratio and increased osmotic fragility, was noted in 33 of 48 patients with HS and in 8 of 13 patients with AIHA. Thus, red cells from a subset of patients with either HS or AIHA may exhibit normal osmotic fragility in the face of decreased surface area, due to a cell dehydration–induced decrease in cell volume.
Osmotic gradient ektacytometric profiles of HS and AIHA blood samples.
The deformability profiles of 4 HS blood samples (left panel) and 7 AIHA blood samples (right panel) are shown. The deformability profile of a representative normal blood sample (thick line) is shown in both panels. DImax, the maximum deformability index, is a measure of red cell surface area; Omin, the osmolality at which the deformability value reaches a minimum in the hypotonic region is a measure of red cell osmotic fragility; and O', the osmolality in the hypertonic region where the deformability index value is half the DImax value is a measure of red cell hydration status. The osmotic gradient ektacytometric profiles of HS and AIHA samples (thin lines) are very similar with variable extents of decreased DImax. In both HS and AIHA, Omin values may be either normal (dashed thin lines) or increased (solid and dotted thin lines) while O' values could be either normal (dotted thin lines) or decreased (solid and dashed thin lines).
Osmotic gradient ektacytometric profiles of HS and AIHA blood samples.
The deformability profiles of 4 HS blood samples (left panel) and 7 AIHA blood samples (right panel) are shown. The deformability profile of a representative normal blood sample (thick line) is shown in both panels. DImax, the maximum deformability index, is a measure of red cell surface area; Omin, the osmolality at which the deformability value reaches a minimum in the hypotonic region is a measure of red cell osmotic fragility; and O', the osmolality in the hypertonic region where the deformability index value is half the DImax value is a measure of red cell hydration status. The osmotic gradient ektacytometric profiles of HS and AIHA samples (thin lines) are very similar with variable extents of decreased DImax. In both HS and AIHA, Omin values may be either normal (dashed thin lines) or increased (solid and dotted thin lines) while O' values could be either normal (dotted thin lines) or decreased (solid and dashed thin lines).
Surface area of reticulocytes and mature red cells
We employed a new experimental strategy to quantitate the surface area of both reticulocytes and mature red cells. In order to validate the new method we measured the surface area of density-fractionated normal red cells. With progressive increase in red cell density, the cell surface area decreased and mean cell hemoglobin concentration increased (Figure 1B). The surface area of the least dense red cells was 145 μm2 and the surface area of the most dense cells was 117 μm.2 These measured values are in agreement with those derived previously using the micropipette method (135 μm2 ± 12 μm2 for the least dense cells and 112 μm2 ± 9 μm2 for most dense cells).18 Having validated the method, we measured surface area of reticulocytes and mature red cells in 12 healthy individuals (Figure 3). The mean surface area of normal reticulocytes is 142.4 μm2 ± 2.0 μm2 (range, 139.6 μm2 -145.9 μm2) and the mean surface area of normal mature red cells is 133.6 μm2 ± 3.0 (range, 128.6 μm2-138.1 μm2). Interestingly, in 3 individuals who had been splenectomized for reasons unrelated to a red cell membrane abnormality, the surface area of mature red cells was significantly higher than in nonsplenectomized normals (139.4 μm2 ± 1.4 μm2 vs 133.6 μm2 ± 3.0 μm2), whereas no difference was noted in the surface area of reticulocytes (143.7 μm2 ± 3.1 μm2 vs 142.4 μm2 ± 2.0 μm2). These findings are consistent with a major role of the spleen in membrane remodeling during the maturation of normal circulating reticulocytes into mature red cells.
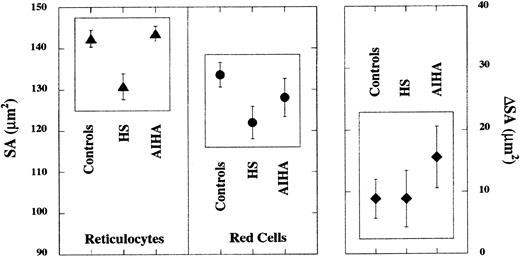
Reticulocyte and red cell surface area in HS and AIHA.
Surface area of reticulocytes (left panel) and of mature red cells (middle panel) in blood samples from control individuals (n = 12) and individuals with HS (n = 12) or AIHA (n = 7). In HS samples, the surface area of both reticulocytes and mature red cells was decreased compared with controls (P < .0001) whereas in AIHA samples, only the surface area of mature red cells (P = .0053), but not of reticulocytes, was decreased. The extent of difference in surface area between reticulocytes and mature red cells (ΔSA) was similar for HS and controls (right panel). In contrast, the difference in surface area between reticulocytes and mature red cells is larger in AIHA when compared with either normal cells (P = .0022) or with HS cells (P = .0084).
Reticulocyte and red cell surface area in HS and AIHA.
Surface area of reticulocytes (left panel) and of mature red cells (middle panel) in blood samples from control individuals (n = 12) and individuals with HS (n = 12) or AIHA (n = 7). In HS samples, the surface area of both reticulocytes and mature red cells was decreased compared with controls (P < .0001) whereas in AIHA samples, only the surface area of mature red cells (P = .0053), but not of reticulocytes, was decreased. The extent of difference in surface area between reticulocytes and mature red cells (ΔSA) was similar for HS and controls (right panel). In contrast, the difference in surface area between reticulocytes and mature red cells is larger in AIHA when compared with either normal cells (P = .0022) or with HS cells (P = .0084).
In 12 patients with HS (7 nonsplenectomized and 5 splenectomized), the surface area of both reticulocytes and mature red cells (Figure 3) was significantly reduced compared with normal cells (P < .0001). The surface area of HS reticulocytes was 130.8 μm2 ± 3.1 μm2 (range, 124.2 μm2 -134.8 μm2) and that of mature HS red cells was 121.9 μm2 ± 3.9 μm2 (range, 114.6 μm2 -130.6 μm2). No noticeable differences in surface area could be documented between cells from nonsplenectomized and splenectomized individuals with HS. It is noteworthy that the difference in surface area between reticulocytes and mature red cells is of very similar magnitude in HS cells and in normal cells (Figure 3). These data imply that surface area loss in HS is manifested at the circulating reticulocyte stage and that the extent of splenic remodeling is similar in patients with HS and in normal controls.
In marked contrast to HS, the surface area of reticulocytes in 7 patients with AIHA was similar to that of normal reticulocytes (Figure3). However, the surface area of mature red cells in AIHA was decreased when compared with normal red cells (Figure 3). The surface area of reticulocytes in AIHA is 143.6 μm2 ± 1.8 μm2 (range, 140.1 μm2 -145.3 μm2) and that of mature red cells is 128.1 μm2 ± 4.6 μm2 (range, 122.6 μm2 -136.0 μm2). The difference in surface area between reticulocytes and mature red cells is larger in AIHA when compared with either normal cells or to HS (Figure 3). The finding that in AIHA only mature red cells, but not reticulocytes, exhibited decreased membrane surface area implies that surface area loss in AIHA occurs only in mature red cells.
Volume and hemoglobin concentration of reticulocytes and red cells
As red cell dehydration has been previously documented in HS,2,13,19 20 we explored if cell dehydration is also a feature of AIHA. Indeed, increased percentage of hyperdense cells (cells with a hemoglobin concentration of > 41.0 g/dL) was a feature of red cells in all cases of HS and in all AIHA cases except one (Table 2). Similarly, mean values of corpuscular hemoglobin concentration of mature red cells (CHCMmRBC) was elevated in all patients with HS and in 12 of the 13 patients with AIHA (Table 2).
Mean cellular hemoglobin concentration of mature red cells and reticulocytes, hemoglobin concentration distribution width, and percentage of hyperdense cells (mean value ± SD)
| . | Controls (n = 37) . | Nonsplenectomized HS (n = 25) . | Splenectomized HS (n = 23) . | AIHA (n = 13) . |
|---|---|---|---|---|
| CHCMmRBC(g/dL) | 32.2 ± 0.7 | 36.1 ± 1.6 | 36.1 ± 0.8 | 35.7 ± 1.3 |
| (range, 31.0-34.1) | (range, 33.8-39.1) | (range, 34.8-37.6) | (range, 33.4-37.1) | |
| HDW (g/dL) | 2.4 ± 0.2 | 3.9 ± 0.6 | 3.0 ± 0.2 | 4.4 ± 1.0 |
| (range, 2.1-2.8) | (range, 2.9-5.0) | (range, 2.6-3.3) | (range, 3.1-6.1) | |
| Hyperdense cells (%) | 0.5 ± 0.3 | 16.6 ± 10.0 | 10.0 ± 4.2 | 12.1 ± 8.1 |
| (range, 0.1-1.5) | (range, 4.6-37.3) | (range, 4.2-20.1) | (range, 2.8-30.2) | |
| CHCMr(g/dL) | 26.6 ± 1.3 | 30.2 ± 2.5 | 31.2 ± 1.2 | 27.5 ± 1.6 |
| (range, 24.5-29.5) | (range, 25.9-35.9) | (range, 29.4-33.7) | (range, 24.9-29.7) |
| . | Controls (n = 37) . | Nonsplenectomized HS (n = 25) . | Splenectomized HS (n = 23) . | AIHA (n = 13) . |
|---|---|---|---|---|
| CHCMmRBC(g/dL) | 32.2 ± 0.7 | 36.1 ± 1.6 | 36.1 ± 0.8 | 35.7 ± 1.3 |
| (range, 31.0-34.1) | (range, 33.8-39.1) | (range, 34.8-37.6) | (range, 33.4-37.1) | |
| HDW (g/dL) | 2.4 ± 0.2 | 3.9 ± 0.6 | 3.0 ± 0.2 | 4.4 ± 1.0 |
| (range, 2.1-2.8) | (range, 2.9-5.0) | (range, 2.6-3.3) | (range, 3.1-6.1) | |
| Hyperdense cells (%) | 0.5 ± 0.3 | 16.6 ± 10.0 | 10.0 ± 4.2 | 12.1 ± 8.1 |
| (range, 0.1-1.5) | (range, 4.6-37.3) | (range, 4.2-20.1) | (range, 2.8-30.2) | |
| CHCMr(g/dL) | 26.6 ± 1.3 | 30.2 ± 2.5 | 31.2 ± 1.2 | 27.5 ± 1.6 |
| (range, 24.5-29.5) | (range, 25.9-35.9) | (range, 29.4-33.7) | (range, 24.9-29.7) |
HS indicates hereditary spherocytosis; AIHA, autoimmune hemolytic anemia; CHCMmRBC, mean cellular hemoglobin concentration of mature red cells; HDW, hemoglobin concentration distribution width; CHCMr, mean cellular hemoglobin concentration of reticulocytes.
To assess if the observed cell dehydration is related to the loss of membrane surface area, we analyzed the hemoglobin concentration and volume histograms of reticulocytes and red cells in HS and AIHA (Figure4). It can be seen that the hemoglobin concentration histogram of HS reticulocytes is shifted toward higher values compared with AIHA reticulocytes. Indeed, mean corpuscular hemoglobin concentration of HS reticulocytes (CHCMr), but not that of AIHA reticulocytes, is significantly increased compared with normal reticulocytes (P < .0001 vs P = .06) (Table2). Cell dehydration and decreased surface area are thus features of both reticulocytes and mature red cells in HS whereas these features are exhibited only by mature red cells in AIHA.
Red cell and reticulocyte indices.
Volume and cell hemoglobin concentration distribution histograms of reticulocytes (dark) and red cells (gray) of a representative normal control, a representative HS, and a representative AIHA blood sample.
Red cell and reticulocyte indices.
Volume and cell hemoglobin concentration distribution histograms of reticulocytes (dark) and red cells (gray) of a representative normal control, a representative HS, and a representative AIHA blood sample.
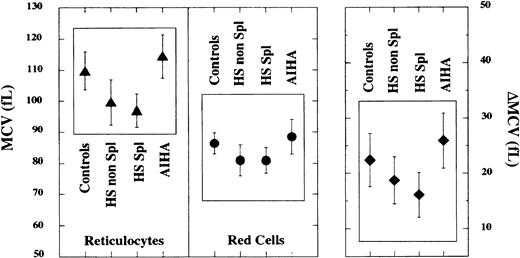
Similarly, it can be seen that the MCVr in patients with HS is shifted toward lower values when compared with AIHA (Figures 4 and 5) and normal control reticulocytes (P < .0001) (Figure5). The MCVr in nonsplenectomized patients with HS is 99.7 fL ± 7.3 fL (range, 86.3 fL-110.9 fL) and in splenectomized patients with HS it is 97.0 fL ± 5.4 fL (range, 87.7 fL-109.4 fL) compared with normal MCVr of 109.8 fL ± 6.1 fL (range, 98.0 fL-123.4 fL). In marked contrast, MCVr in AIHA was found to be modestly increased from normal cells (P = .03). As already observed,2 the MCV of mature HS red cells in both nonsplenectomized and splenectomized patients is also decreased compared with that of normal red cells (P < .0001) (Figure 5) whereas the MCV of AIHA mature red cells was not significantly different than that of normal red cells (P = .12) (Figure 5).
Reticulocyte and red cell volume in HS and AIHA.
Mean cell volume of reticulocytes (left panel) and of mature red cells (middle panel) in blood samples from 37 adult control individuals, 25 nonsplenectomized individuals with HS, 23 splenectomized individuals with HS, and 13 nonsplenectomized individuals with AIHA. MCV of both reticulocytes and of mature red blood cells in HS blood samples was decreased compared with controls (P < .0001). No significant differences were noted between splenectomized or nonsplenectomized HS samples. In contrast, in AIHA, blood samples MCV of reticulocytes was modestly increased compared with controls (P = .03) whereas the MCV of mature red blood cells was similar to that of controls. The extent of difference in cell volume between reticulocytes and mature red cells (ΔMCV) in AIHA was not different from the control (right panel), whereas it was significantly decreased in HS (P < .0001).
Reticulocyte and red cell volume in HS and AIHA.
Mean cell volume of reticulocytes (left panel) and of mature red cells (middle panel) in blood samples from 37 adult control individuals, 25 nonsplenectomized individuals with HS, 23 splenectomized individuals with HS, and 13 nonsplenectomized individuals with AIHA. MCV of both reticulocytes and of mature red blood cells in HS blood samples was decreased compared with controls (P < .0001). No significant differences were noted between splenectomized or nonsplenectomized HS samples. In contrast, in AIHA, blood samples MCV of reticulocytes was modestly increased compared with controls (P = .03) whereas the MCV of mature red blood cells was similar to that of controls. The extent of difference in cell volume between reticulocytes and mature red cells (ΔMCV) in AIHA was not different from the control (right panel), whereas it was significantly decreased in HS (P < .0001).
Reversal of red cell abnormalities in AIHA following treatment
To obtain further support for the potential relationship between surface area loss and cell dehydration, we monitored various red cell parameters following steroid therapy and normalization of the antiglobulin test (DAT) in 3 patients with AIHA. Representative data from one of these individuals is shown in Figure6. Following treatment, the osmotic deformability profile showed a normal DImax value, implying normal cell surface area. The hemoglobin concentration histogram showed marked reduction in the percentage of dense red cells, implying decreased cell dehydration.
Reversal of red cell abnormalities in AIHA following steroid therapy.
The osmotic deformability profiles (top panel) of blood samples from an individual with AIHA at the time of diagnosis (dashed lines) and following steroid therapy (solid line). The deformability profile of a representative normal blood sample is indicated by the thick line. Note the complete normalization of the deformability profile following treatment. Volume and cell hemoglobin concentration distribution histograms of red cells from the same individual with AIHA before and after steroid therapy. Note the complete disappearance of dehydrated red cells with cell hemoglobin concentration of more than 41 g/dL following steroid therapy.
Reversal of red cell abnormalities in AIHA following steroid therapy.
The osmotic deformability profiles (top panel) of blood samples from an individual with AIHA at the time of diagnosis (dashed lines) and following steroid therapy (solid line). The deformability profile of a representative normal blood sample is indicated by the thick line. Note the complete normalization of the deformability profile following treatment. Volume and cell hemoglobin concentration distribution histograms of red cells from the same individual with AIHA before and after steroid therapy. Note the complete disappearance of dehydrated red cells with cell hemoglobin concentration of more than 41 g/dL following steroid therapy.
Discussion
By maintaining a favorable surface area to volume ratio, the normal red cell is able to undergo the extensive passive deformations1,2,16,18,21-24 needed to traverse the microvasculature for optimal oxygen delivery. Loss of cell surface area resulting in increased sphericity18,23,24 is detrimental for red cell deformability and there is experimental evidence that these spherical cells are rapidly sequestered from circulation by the spleen.5,9,11,25-30 Hemolytic anemia characterized by spherocytic red cells with reduced membrane surface area is a feature of HS1,2,19 and of some forms of AIHA.4 In HS, the spherocyte formation has long been attributed to the increase propensity of abnormal red cells to shed membrane during their sojourn in circulation due to improper assembly of membrane proteins6-8 whereas in AIHA it is due to partial phagocytosis4 of the circulating red cell membrane bound antibodies complexes by macrophages.4,5,10,11,28 We surmised that these different mechanisms could result in temporal differences in surface area loss in these 2 spherocytic syndromes. Specifically, we proposed that cell surface loss could occur during erythroid maturation in the bone marrow in HS whereas surface area loss in AIHA might only involve circulating mature red cells. Using a novel technique12 to quantitate cell surface area, we indeed were able to document developmentally related temporal differences in membrane loss in HS and AIHA. Specifically decreased membrane surface area is a feature of HS reticulocytes but not of AIHA reticulocytes. On the other hand, mature red cells of both HS and AIHA exhibited decreased surface area. These data imply that surface area loss in HS, but not in AIHA, is already present at the circulating reticulocyte stage. In fact, much of the observed difference in cell surface area of HS and normal red cells can be attributed to decreased surface area at the reticulocyte stage. These findings have enabled us to unequivocally establish that loss of cell surface area is an early event during genesis of HS red cells. Moreover, the findings raise interesting issues regarding how disordered membrane assembly during erythropoiesis can lead to membrane loss.8,31,32 It is also intriguing to note that the average difference in the surface area of reticulocytes and mature red cells in HS is identical to that seen in normal cells. In marked contrast, cell surface loss in AIHA occurs during the life span of the mature red cells in circulation: the average difference in the surface areas of reticulocytes and mature red cells in AIHA is 15.6 μm2 compared with 8.9 μm2 in both normal cells and HS. These findings imply an extensive membrane loss involving mature circulating AIHA red cells, as a result of partial phagocytosis of the antibody-coated membrane,4,5 10 while normal and HS red cells experience similar extents of membrane loss during their life span.
Progressive decrease in red cell surface area and cell volume has been shown to occur during their life span in circulation.18,23,24,33 As a consequence of decreased cell volume, red cells with decreased membrane surface area have elevated cell hemoglobin concentration. It is unclear, however, if a direct relationship exists between membrane loss and decreased cell volume. In a recent study, Waugh and colleagues23 showed that following reinfusion of red cells with decreased membrane surface area and increased sphericity, the surviving fraction of spherocytic red cells progressively reduced their cell volume to attain a more favorable surface area to volume ratio and decreased cell sphericity index. These findings strongly suggest that following membrane loss, normal red cells can initiate volume regulatory pathways that enable them to reduce their volume and thereby reduce their sphericity, which in turn prolongs their life span. HS reticulocytes from the very beginning have decreased cell volume and increased cell hemoglobin concentration, which probably result from an early attempt to counterbalance membrane loss. It would be interesting in future studies to determine which of the various volume regulatory pathways contribute to the tight coupling between cell surface area and cell volume. One practical consequence of the tight coupling between volume and surface area loss in HS is that HS reticulocyte volume is consistently lower and hemoglobin concentration consistently higher than those of either normal or AIHA reticulocytes.
The filtration function of the spleen is well known. The spherocytes are trapped in “red” pulp of the cords of Billroth5,9,26,27 because they are less deformable1,2,21,22 than normal red cells and thus not able to traverse through the endothelium of splenic sinuses. The trapped cells are subsequently destroyed by the macrophages.5 Support for this thesis comes from the observation that the life span of red cells in HS is significantly increased following splenectomy. Life span of spherocytic red cells has been shown to negatively correlate with the mean intrasplenic red cell transit, in HS and AIHA.24,25,34,35 In addition to removing damaged or senescent red cells from the circulation, the spleen also plays a role in reticulocyte membrane remodeling.36-38 Remodeling of reticulocytes into mature red cells involves loss of lipid membrane,31,39,40 loss of surface area,12,19,41 and decrease in cell volume.41-43 Our finding that the surface area of mature red cells from individuals splenectomized for reasons unrelated to a blood cell disorder was significantly higher than in nonsplenectomized healthy controls in the absence of increased surface area of reticulocytes supports a key role for the spleen in inducing selective membrane loss during maturation of the normal reticulocyte into a mature red cell. However, our finding that the striking reduction in cell surface area can be observed as early as the reticulocyte stage in both nonsplenectomized and splenectomized patients with HS makes it unlikely that excessive remodeling of HS reticulocytes during the splenic passage is responsible for their decreased surface area. We have thus obtained an important insight into the function of the spleen in HS: although the spleen plays a major role in sequestering spherical cells from the circulation, accounting for their reduced survival, the contribution of this organ to the generation of spherocytic HS red cells with reduced surface area is much less important than previously implied. The reduced surface area of HS reticulocytes that we documented is likely to arise precociously during membrane assembly during erythropoiesis,8,31,32,44enucleation,45-47 or reticulocyte egress from the bone marrow.48 49 Further, in vivo and in vitro studies are necessary to define the contributions of these different mechanisms to the reduced surface area of HS reticulocytes. As such, documentation of the presence of small, dehydrated reticulocytes in the context of spherocytosis could be potentially useful in distinguishing spherocytes of HS from those of AIHA.
We thank Joel-Anne Chasis and Frédéric Bouquet for their insightful comments regarding the manuscript.
Supported in part by la Direction de la Recherche Clinique Assistance Publique-Hopitaux de Paris (CRC96082) and by a National Institutes of Health grant DK26263.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Narla Mohandas, Lawrence Berkeley National Laboratory, Mailstop 74-157, 1 Cyclotron Rd, Berkeley, CA 94720; e-mail: mnarla@lbl.gov.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal