Activated protein C (APC) resistance1 due to the factor V (FV) gene mutation G1691A (single-letter nucleotide codes)2 and the prothrombin gene mutation G20210A3 are the most common genetic disorders associated with venous thrombosis. APC resistance not due to the FV gene mutation G1691A,4,5 and the hyperprothrombinemia secondary to the prothrombin gene mutation G20210A,3 are also independent risk factors for venous thrombosis. Although it has been surmised that high levels of prothrombin in plasma may result in an increased rate of thrombin generation6 or increased thrombin potential,7 little is known on how hyperprothrombinemia leads to venous thrombosis. Recently, Smirnov and colleagues reported on an additional mechanism that might contribute to the pathogenetic role of hyperprothrombinemia.8 They showed that prothrombin may act as a modulator of the anticoagulant activity of APC both in a purified system and in plasma by inhibiting the ability of APC to inactivate FVa.
On the basis of this observation, one would predict that individuals with hyperprothrombinemia might also have acquired APC resistance as measured with the common aPTT-based test. To test this hypothesis, we selected from our files data on 285 individuals who served as controls in a previous study designed to assess the prevalence of the prothrombin gene mutation G20210A in our patient population.9 Individuals included in the analysis were those for whom APC resistance and prothrombin levels were available and those who were not carriers of the FV gene mutation G1691A. APC resistance was measured with the original aPTT-based test described by Dahlback et al1 as modified by Faioni et al10; results were expressed as normalized APC ratios (n-APC-ratios) against a frozen pooled normal plasma. Prothrombin was measured using S-2238 (Chromogenix, Mölndal, Sweden) as substrate and Echis Carinatus (Sigma, St Louis, MO) as activator11; results were expressed as U/dL against a pooled normal plasma arbitrarily set at 100 U/dL.
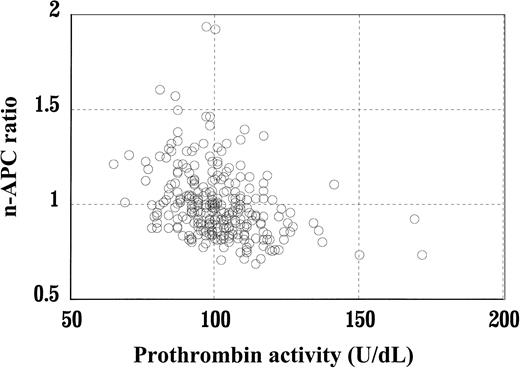
As shown in the figure, there was an inverse relationship between n-APC-ratios and prothrombin activity (r = −0.32, P < .001). In particular, 7 of the 60 subjects (12%) with prothrombin levels higher than the 80th percentile (ie, 110 U/dL) had n-APC-ratios lower than the lower limit for APC resistance (ie, 0.76) established for this method at our laboratory. In contrast, only 2 of the 225 subjects (1%) with prothrombin levels lower than the 80th percentile had n-APC ratios lower than the lower limit (P < .0001, Fisher exact test). These results support the view that plasma prothrombin is a determinant of APC resistance and may explain the mechanism through which hyperprothrombinemia is associated with an increased risk for venous thrombosis.
Normalized activated protein C ratios as a function of prothrombin levels in subjects without the FV gene mutation G1691A.
n-APC-ratios are inversely correlated to prothrombin levels (r = −0.32, P < .001).
Normalized activated protein C ratios as a function of prothrombin levels in subjects without the FV gene mutation G1691A.
n-APC-ratios are inversely correlated to prothrombin levels (r = −0.32, P < .001).
Furthermore, these results indicate that hyperprothrombinemia is another determinant of acquired APC resistance, like high factor VIII (FVIII) plasma levels.12 We surmise, however, that high levels of the 2 proteins act through different mechanisms. Perhaps high FVIII levels act by increasing the procoagulant strength of plasma as measured by the aPTT, a test that is very responsive to high FVIII levels.12 In contrast, as shown by Smirnov and colleagues, prothrombin is likely to act directly by inhibiting APC.8

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal