Abstract
Granulocyte colony-stimulating factor (G-CSF) has had a major impact on management of “severe chronic neutropenia,” a collective term referring to congenital, idiopathic, or cyclic neutropenia. Almost all patients respond to G-CSF with increased neutrophils, reduced infections, and improved survival. Some responders with congenital neutropenia have developed myelodysplastic syndrome and acute myeloblastic leukemia (MDS/AML), which raises the question of the role of G-CSF in pathogenesis. The Severe Chronic Neutropenia International Registry (SCNIR), Seattle, WA, has data on 696 neutropenic patients, including 352 patients with congenital neutropenia, treated with G-CSF from 1987 to present. Treatment and patient demographic data were analyzed. The 352 congenital patients were observed for a mean of 6 years (range, 0.1-11 years) while being treated. Of these patients, 31 developed MDS/AML, for a crude rate of malignant transformation of nearly 9%. None of the 344 patients with idiopathic or cyclic neutropenia developed MDS/AML. Transformation was associated with acquired marrow cytogenetic clonal changes: 18 patients developed a partial or complete loss of chromosome 7, and 9 patients manifested abnormalities of chromosome 21 (usually trisomy 21). For each yearly treatment interval, the annual rate of MDS/AML development was less than 2%. No significant relationships between age at onset of MDS/AML and patient gender, G-CSF dose, or treatment duration were found (P > .15). In addition to the 31 patients who developed MDS/AML, the SCNIR also has data on 9 additional neutropenic patients whose bone marrow studies show cytogenetic clonal changes but the patients are without transformation to MDS/AML. Although our data does not support a cause-and-effect relationship between development of MDS/AML and G-CSF therapy or other patient demographics, we cannot exclude a direct contribution of G-CSF in the pathogenesis of MDS/AML. This issue is unclear because MDS/AML was not seen in cyclic or idiopathic neutropenia. Improved survival of congenital neutropenia patients receiving G-CSF therapy may allow time for the expression of the leukemic predisposition that characterizes the natural history of these disorders. However, other factors related to G-CSF may also be operative in the setting of congenital neutropenia.
Severe chronic neutropenia (SCN) and recurrent serious infections are features of a heterogeneous group of disorders of myelopoiesis including congenital neutropenia, cyclic neutropenia, and idiopathic neutropenia. In keeping with the definition of SCN, these disorders are all characterized by absolute neutrophil counts of less than 0.5 × 109 counts per L on 3 separate occasions during 6 months of observation. Kostmann's syndrome, a subtype of congenital neutropenia inherited in an autosomal recessive manner, is characterized by early childhood onset of profound neutropenia, recurrent life-threatening infections, and a maturation arrest of bone marrow myeloid precursors at the promyelocyte-myelocyte stage of differentiation.1 2
Severe congenital neutropenia described herein has the same hematologic phenotype and clinical presentation as Kostmann's syndrome. Neutropenia is profound, with usually less than 0.2 × 109 neutrophil counts per L, and often absolute. The recessive inheritance of Kostmann's syndrome is deduced by inference when there is more than 1 affected child in a family. Congenital neutropenia is the more appropriate designation used for a single “sporadic” case in a family, and hence, may or may not be inherited in an autosomal recessive manner as is Kostmann's syndrome. Because at least one of the causes of SCN has only recently been discovered, and molecular diagnostic methods have not yet been readily available to distinguish between the disorders termed Kostmann's syndrome, the option to “lump” or “split” the 2 disorders remains a subject of argument. For this report, the terms Kostmann's syndrome and congenital neutropenia are used interchangeably. Shwachman-Diamond syndrome (SDS), an additional but discrete subtype of congenital neutropenia, is inherited in an autosomal recessive manner and consists basically of exocrine pancreatic insufficiency and varying degrees of neutropenia, usually with growth failure.3
Prior to the availability of recombinant human granulocyte colony-stimulating factor (G-CSF), it was recognized that leukemic transformation occurred in patients with these congenital forms of neutropenia.4-7 In the subgroup with SDS, the predisposition to spontaneous leukemic transformation is inordinately high, possibly up to 30%.8,9 However, in the precytokine era, many congenital neutropenia patients died in the first years of life from other causes. According to published cases of Kostmann's syndrome, for example, 42% of patients died, secondary to sepsis or pneumonia, at a mean age of 2 years.10 Thus, the true risk of congenital neutropenia patients developing myelodysplasia syndrome and/or acute myeloblastic leukemia (MDS/AML) has never been defined.
With G-CSF therapy, more than 90% of patients have responded with increased neutrophil numbers, have not developed life-threatening infections, and have survived well beyond 2 years of age. However, it is not known if increased survival will allow for the natural expression of leukemogenesis in this population. Moreover, because the long-term effects of G-CSF are not known beyond 11 years of observation, it is still unclear whether MDS or AML will occur with increased frequency in patients who receive G-CSF on a chronic life-long basis.
To address these issues, the largest currently available database of chronic neutropenia patients treated with G-CSF was used to determine the incidence of malignant myeloid transformation and its relationship to treatment and to other patient demographics that may be operative. The following hypothesis was also addressed: If the risk of transformation is directly dependent on G-CSF therapy, there should be a relationship to the duration of G-CSF treatment or to the dosage given.
Patients, materials, and methods
The Severe Chronic Neutropenia International Registry
In 1987, Amgen, Inc (Boulder, CO, and Thousand Oaks, CA) initiated clinical trials to test G-CSF therapy for SCN; 335 patients were enrolled and followed prospectively until 1994. The Severe Chronic Neutropenia International Registry (SCNIR), Seattle, WA, was established in 1994 to continue monitoring the clinical course, treatment, and disease outcomes of patients with SCN.11-21Clinical trial data from 1987-1994 were retrospectively transferred to the Registry and were added to the data of newly diagnosed SCN patients from 1994 onward. SCNIR is a unique resource that continues to collect clinical data on large numbers of patients worldwide. Patient data are submitted internationally to the data coordinating centers at the University of Washington, Seattle, and the Medizinische Hochschule, Hannover, Germany.
The Registry's administrative and operational structure consists of 5 components: (1) an international Scientific Advisory Board of 10 physicians/hematologists; (2) a panel of European local liaison physicians who treat neutropenic patients; (3) the Registry data coordinating offices, which are responsible for data collection; (4) Amgen's International Clinical Safety Department; and (5) a Safety Monitoring Committee, which comprises 3 physicians and 2 scientists who address the risks and benefits of G-CSF therapy with regard to the hazard of MDS/AML arising during treatment.
For this report, all data received as of December 31, 1998, were available for analysis. Patients who met the eligibility criteria with documented persistent severe neutropenia (less than 0.5 × 109 absolute neutrophil counts per L), a confirmed diagnosis of SCN, and signed release of medical information were eligible for enrollment in the SCNIR.
Criteria for diagnosis and classification
Entry criteria for enrollment in the SCNIR required documentation of severe neutropenia, defined as an absolute neutrophil count of less than 0.5 × 109 counts per L on 3 separate occasions during at least a 6-month period. Severe congenital neutropenia patients in the SCNIR have the identical hematologic phenotype and clinical presentation as Kostmann's syndrome and, hence, the terms are used interchangeably. The diagnostic criteria for congenital neutropenia and for SDS are detailed in the “Introduction.” Patients with cyclic neutropenia were required to demonstrate 5 consecutive days per cycle of absolute neutrophil counts of less than 0.5 × 109 counts per L for each of 3 regularly spaced cycles during a 6-month period. The term idiopathic neutropenia refers to the onset of absolute neutrophil counts of less than 0.5 × 109 counts per L from months to years after birth without apparent cause. Excluded from the idiopathic group are patients with marrow clonal cytogenetic abnormalities at diagnosis or with MDS, aplastic anemia, collagen vascular and autoimmune disease including Felty's syndrome, and drug-induced neutropenia. The SCNIR does not have data on the incidence of antineutrophil antibodies in idiopathic neutropenia patients.
Clinical monitoring
Bone marrow aspirations for morphology and cytogenetic studies were performed at local institutions prior to G-CSF therapy and were required at 12-month intervals thereafter for all enrolled patients who were receiving treatment through 1996. After October 1996, when the data indicated that only patients with congenital neutropenia were at risk of MDS/AML, the annual requirement for marrow testing was dropped for patients with cyclic and idiopathic neutropenia. Patients were seen at varying intervals for assessment of hematological and clinical parameters. For the patients enrolled in the SCNIR, data assessment forms were requested from the treating physicians every 6 months. For patients enrolled in clinical trials from 1987 to 1994, hematological studies were collected at least monthly. The discovery of a cytogenetic clonal abnormality of marrow cells or marrow morphologic changes of MDS or AML were reported immediately.
Statistical analysis and study design
The protocol design used to analyze the Registry data can be described as nonrandomized, noncontrolled, multicentered, and observational. All patients in the SCNIR were followed through December 31, 1998. Univariate descriptive statistics were generated on all demographic, hematologic, and dosing parameters. The Kaplan-Meier21 method was used to estimate hazard rates and probability of conversion to MDS/AML for years of treatment with G-CSF and for age. The Cox proportional hazards model22 was used to assess both the univariate and multivariate effects G-CSF dosage, years of treatment with G-CSF, and demographic factors on the age of MDS/AML conversion. All statistical analyses were performed using SAS.23
Results
Patient demographics
By the end of 1998, we had received information dating back to 1987 on a total of 648 patients submitted by 358 treating physicians from 13 countries (Table 1). Of this total, 304 patients were classified as having congenital neutropenia (including Kostmann's syndrome and SDS). Of the other patients, 132 had cyclic neutropenia, and 212 patients had idiopathic neutropenia.
Demographics by diagnosis of 648 patients enrolled at end of 1998 in the SCNIR
| . | Patients with congenital neutropenia (n = 304) . | Patients with cyclic neutropenia (n = 132) . | Patients with idiopathic neutropenia (n = 212) . | Total patients (n = 648) . |
|---|---|---|---|---|
| Age, mean (range), y | 12.8 (0.4-49.7) | 22.8 (1.4-76.0) | 29.3 (1.9-88.7) | 20.2 (0.4-88.7) |
| Age category | ||||
| Pediatric, <18 y; n (%) | 240 (78.9) | 66 (50) | 82 (38.7) | 388 (59.9) |
| Adult, ≥18 y; n (%) | 64 (21.1) | 66 (50) | 130 (61.3) | 260 (40.1) |
| Sex | ||||
| Male, n (%) | 156 (51.3) | 59 (44.7) | 65 (30.7) | 280 (43.2) |
| Female, n (%) | 148 (48.7) | 73 (55.3) | 147 (69.3) | 368 (56.8) |
| Race | ||||
| Caucasian | 252 | 118 | 204 | 574 |
| Black | 18 | 4 | — | 22 |
| Asian | 11 | — | 1 | 12 |
| Hispanic | 15 | 2 | 2 | 19 |
| Unknown | 8 | 8 | 5 | 21 |
| . | Patients with congenital neutropenia (n = 304) . | Patients with cyclic neutropenia (n = 132) . | Patients with idiopathic neutropenia (n = 212) . | Total patients (n = 648) . |
|---|---|---|---|---|
| Age, mean (range), y | 12.8 (0.4-49.7) | 22.8 (1.4-76.0) | 29.3 (1.9-88.7) | 20.2 (0.4-88.7) |
| Age category | ||||
| Pediatric, <18 y; n (%) | 240 (78.9) | 66 (50) | 82 (38.7) | 388 (59.9) |
| Adult, ≥18 y; n (%) | 64 (21.1) | 66 (50) | 130 (61.3) | 260 (40.1) |
| Sex | ||||
| Male, n (%) | 156 (51.3) | 59 (44.7) | 65 (30.7) | 280 (43.2) |
| Female, n (%) | 148 (48.7) | 73 (55.3) | 147 (69.3) | 368 (56.8) |
| Race | ||||
| Caucasian | 252 | 118 | 204 | 574 |
| Black | 18 | 4 | — | 22 |
| Asian | 11 | — | 1 | 12 |
| Hispanic | 15 | 2 | 2 | 19 |
| Unknown | 8 | 8 | 5 | 21 |
In addition to the 304 patients with congenital neutropenia (Table 1), the SCNIR compiled data on 48 congenital patients who were enrolled in industry-sponsored G-CSF clinical trials from 1987 to 1994. These patients were not prospectively enrolled in the SCNIR for a variety of reasons; most commonly, death occurred prior to enrollment. Thus, a total of 352 patients (304 plus 48 patients) with congenital neutropenia who were treated with G-CSF were available for analysis.
Efficacy of G-CSF therapy
Previous clinical trials of G-CSF therapy in patients with congenital neutropenia were conducted for up to 6 years. In more than 90% of these patients, the cytokine selectively increased and sustained blood neutrophil numbers with little effect on other blood counts.24 From a subset of 238 patients in the SCNIR database, only 8 patients (3%) failed to experience a sustained increase in neutrophil counts, even when they were given large daily doses (greater than 100 μg/kg) of G-CSF.16 Responders have sustained a mean absolute neutrophil count of more than 2.0 × 109 counts per L for up to 10 years of observation. As of December 1998, SCNIR patients with congenital neutropenia were receiving a mean daily G-CSF subcutaneous dose of 13.8 μg/kg (range, 0.1-240 μg/kg), with a mean therapy duration of 6 years (range, 0.1-11 years). For patients with cyclic neutropenia and idiopathic neutropenia, G-CSF induced identical neutrophil responses in more than 90% of the patients in each diagnostic category. The mean daily G-CSF dose for both groups was lower than the mean dose for the congenital neutropenia patients (for cyclic neutropenia, 2.64 μg/kg; for idiopathic neutropenia, 2.4 μg/kg).
Malignant myeloid transformation
Of the 352 patients with congenital neutropenia who were treated with G-CSF, 31 patients developed MDS/AML from 1987 to December 1998. Thus, the overall incidence or crude rate of malignant transformation is 8.8%, with an average follow-up rate of 6 years. Of these 31 patients, 29 were diagnosed with a type of Kostmann's syndrome congenital neutropenia, and 2 patients were classified as having SDS. It is noteworthy that to date, there have been no cases of MDS/AML reported in patients with glycogen storage disease type 1b (the other subgroup of congenital neutropenia). There also have been no reported cases of MDS/AML in any SCNIR patients with cyclic or idiopathic neutropenia who have been treated with G-CSF for up to 11 years.
In Table 2, summary demographic and dosing information of the patients who converted to MDS/AML are compared with those who did not convert, and Table 3provides individual details of all 31 patients with MDS/AML. The ages of the patients varied widely. There was a preponderance of male patients (n = 18, 58%), but this was not statistically significant compared with patients who did not convert to MDS/AML (51% of total). The patients who converted to MDS/AML received a broad range of G-CSF daily doses (from 1-58 μg/kg/d), and there was no consistent pattern of prescribed dosage. To answer the question of whether there was a difference between the G-CSF doses given to MDS/AML patients versus those without MDS/AML, an analysis of variance was performed and failed to show a significant trend (P = .83). The Cox proportional hazards model was used to determine if there was a relationship between the G-CSF dose and patient age when MDS/AML developed, and none was demonstrated (P = .15).
Comparison of demographics and G-CSF dosing among patients who converted to MDS/AML and those who did not convert
| . | Nonconverters (n = 321) . | Converters (n = 31) . |
|---|---|---|
| Sex | ||
| Male, n (%) | 164 (51) | 18 (58) |
| Female, n (%) | 157 (49) | 13 (42) |
| Age | ||
| Mean (SD), y | 11.1 (9.4) | 13.6 (10.1) |
| Median (range), y | 9.7 (0.3-45.2) | 12.4 (2.3-49.3) |
| Dose of G-CSF | ||
| Mean (SD), μg/kg/day | 13.2 (23.7) | 14.4 (12.2) |
| Median (range), μg/kg/day | 6 (0.1-240) | 12 (1-58) |
| Duration of G-CSF | ||
| Mean (SD), y | 4.5 (3.1) | 4.9 (2.4) |
| Median (range), y | 3.9 (0.1-10.5) | 4.9 (0.1-9.1) |
| . | Nonconverters (n = 321) . | Converters (n = 31) . |
|---|---|---|
| Sex | ||
| Male, n (%) | 164 (51) | 18 (58) |
| Female, n (%) | 157 (49) | 13 (42) |
| Age | ||
| Mean (SD), y | 11.1 (9.4) | 13.6 (10.1) |
| Median (range), y | 9.7 (0.3-45.2) | 12.4 (2.3-49.3) |
| Dose of G-CSF | ||
| Mean (SD), μg/kg/day | 13.2 (23.7) | 14.4 (12.2) |
| Median (range), μg/kg/day | 6 (0.1-240) | 12 (1-58) |
| Duration of G-CSF | ||
| Mean (SD), y | 4.5 (3.1) | 4.9 (2.4) |
| Median (range), y | 3.9 (0.1-10.5) | 4.9 (0.1-9.1) |
Data on 31 patients with congenital neutropenia who developed malignant myeloid transformation while receiving G-CSF therapy
| Patient no. . | Age, y . | Sex . | Diagnosis . | Duration of G-CSF to MDS/AML, mo . | G-CSF dose,3-150 μg/kg/d . | Prior marrow cytogenetic evaluation . | Cytogenetic abnormality . |
|---|---|---|---|---|---|---|---|
| 1 | 8 | M | MDS | 52 | 20 | unknown | trisomy 21 |
| monosomy 7 | |||||||
| 2 | 48 | M | MDS/AML | 57.4 | 2.4 | normal | monosomy 7 |
| del(6)(q21) | |||||||
| 3 | 12 | M | MDS/AML | 58 | 20 | normal | trisomy 21 |
| monosomy 7 | |||||||
| 4 | 8 | F | AML | 73 | 18 | normal/on-study | 48, xx +marker × 2 |
| 5 | 4 | F | AML | 53 | 6.3 | normal | monosomy 7 |
| 6 | 12 | M | AML | 9 | — | normal | trisomy (3)(22) |
| der (5) | |||||||
| t(1;5)(q21;q21) | |||||||
| 7 | 20 | F | AML, SDS | 1 | 6 | not done | del(3)(7)(21) |
| 8 | 10 | F | MDS/CMML | 39 | 40 | not done | monosomy 7 |
| del(q20) | |||||||
| 9 | 13 | M | AML | 85.8 | 6 | normal | 46,xy,der(9) |
| t(6;9)(q15;q34) | |||||||
| 37,xy,add(3)(q26) | |||||||
| 10 | 12 | M | AML | 101 | 20 | normal | normal |
| 11 | 7 | F | MDS/AML | 68 | 24.6 | normal | del(2)(q31;q36) |
| del(2)(q32;2) | |||||||
| del(7)(q32) | |||||||
| del(5)(q31;q34) | |||||||
| del(7)(q22;q32) | |||||||
| 12 | 15 | M | MDS | 75 | 6 | normal | monosomy 7 |
| del(6)(q21;q26) | |||||||
| 13 | 4 | F | AML | 44.2 | 13.5 | normal/on-study | inv 16(p13;q22) |
| t(5;6)(q31;q27) | |||||||
| 14 | 17 | M | AML | 84 | 6 | normal | normal |
| 15 | 8 | F | AML | 79 | 38 | normal | normal |
| 16 | 20 | F | AML | 98.8 | 12 | normal | i(17)(q10) 3/20 |
| (8.23 y) | idem, +8 10/20 | ||||||
| 17 | 40 | M | MDS/AML | 73 | 8.6 | normal/on-study | monosomy 7 |
| 18 | 13 | M | AML | 101.1 | 12 | normal | add (11)(q24) |
| (8.4 y) | i(21)(q10) 13/20 | ||||||
| add (11)(q24) | |||||||
| +21, +mar 6/20 | |||||||
| 19 | 19 | F | MDS | 99.1 | 6 | normal | (t3,21) |
| (8.3 y) | |||||||
| 20 | 4 | M | AML | 32.8 | 35 | not done | monosomy 7 |
| trisomy 11 | |||||||
| 21 | 12 | M | MDS | 22.7 | 8.7 | not done; baseline FISH negative for monosomy 7 | monosomy 7 trisomy 21 |
| 22 | 15 | M | MDS | 76 | 12 | normal | trisomy 21, +x |
| 23 | 5 | M | MDS/AML | 29 | 30 | normal/on-study | monosomy 7 |
| 24 | 8 | F | AML | 78.9 | 20 | normal/on-study | t(p1;q3) |
| elongation of 5q | |||||||
| 25 | 23 | M | MDS/AML | 35 | 1 | not done | monosomy 7 |
| trisomy 21 | |||||||
| 26 | 18 | M | AML | 2 | 3.5 | not done | t(9;11) |
| 27 | 13 | M | MDS/AML | 59.8 | 16 | not done | monosomy 7 |
| trisomy 21 | |||||||
| 28 | 10 | F | MDS | 72 | — | not done | monosomy 7 |
| 29 | 2 | F | AML | 20 | 13 | normal | del (7)(q22q36)[22] |
| del (6)(p22p25) | |||||||
| del (7)(22q36)[3] | |||||||
| 30 | 5 | M | MDS, SDS | 22 | 7 | normal | monosomy 7 |
| 31 | 16 | F | AML | 102 | 2.6 | normal/on-study | monosomy 7 |
| tetraploidy |
| Patient no. . | Age, y . | Sex . | Diagnosis . | Duration of G-CSF to MDS/AML, mo . | G-CSF dose,3-150 μg/kg/d . | Prior marrow cytogenetic evaluation . | Cytogenetic abnormality . |
|---|---|---|---|---|---|---|---|
| 1 | 8 | M | MDS | 52 | 20 | unknown | trisomy 21 |
| monosomy 7 | |||||||
| 2 | 48 | M | MDS/AML | 57.4 | 2.4 | normal | monosomy 7 |
| del(6)(q21) | |||||||
| 3 | 12 | M | MDS/AML | 58 | 20 | normal | trisomy 21 |
| monosomy 7 | |||||||
| 4 | 8 | F | AML | 73 | 18 | normal/on-study | 48, xx +marker × 2 |
| 5 | 4 | F | AML | 53 | 6.3 | normal | monosomy 7 |
| 6 | 12 | M | AML | 9 | — | normal | trisomy (3)(22) |
| der (5) | |||||||
| t(1;5)(q21;q21) | |||||||
| 7 | 20 | F | AML, SDS | 1 | 6 | not done | del(3)(7)(21) |
| 8 | 10 | F | MDS/CMML | 39 | 40 | not done | monosomy 7 |
| del(q20) | |||||||
| 9 | 13 | M | AML | 85.8 | 6 | normal | 46,xy,der(9) |
| t(6;9)(q15;q34) | |||||||
| 37,xy,add(3)(q26) | |||||||
| 10 | 12 | M | AML | 101 | 20 | normal | normal |
| 11 | 7 | F | MDS/AML | 68 | 24.6 | normal | del(2)(q31;q36) |
| del(2)(q32;2) | |||||||
| del(7)(q32) | |||||||
| del(5)(q31;q34) | |||||||
| del(7)(q22;q32) | |||||||
| 12 | 15 | M | MDS | 75 | 6 | normal | monosomy 7 |
| del(6)(q21;q26) | |||||||
| 13 | 4 | F | AML | 44.2 | 13.5 | normal/on-study | inv 16(p13;q22) |
| t(5;6)(q31;q27) | |||||||
| 14 | 17 | M | AML | 84 | 6 | normal | normal |
| 15 | 8 | F | AML | 79 | 38 | normal | normal |
| 16 | 20 | F | AML | 98.8 | 12 | normal | i(17)(q10) 3/20 |
| (8.23 y) | idem, +8 10/20 | ||||||
| 17 | 40 | M | MDS/AML | 73 | 8.6 | normal/on-study | monosomy 7 |
| 18 | 13 | M | AML | 101.1 | 12 | normal | add (11)(q24) |
| (8.4 y) | i(21)(q10) 13/20 | ||||||
| add (11)(q24) | |||||||
| +21, +mar 6/20 | |||||||
| 19 | 19 | F | MDS | 99.1 | 6 | normal | (t3,21) |
| (8.3 y) | |||||||
| 20 | 4 | M | AML | 32.8 | 35 | not done | monosomy 7 |
| trisomy 11 | |||||||
| 21 | 12 | M | MDS | 22.7 | 8.7 | not done; baseline FISH negative for monosomy 7 | monosomy 7 trisomy 21 |
| 22 | 15 | M | MDS | 76 | 12 | normal | trisomy 21, +x |
| 23 | 5 | M | MDS/AML | 29 | 30 | normal/on-study | monosomy 7 |
| 24 | 8 | F | AML | 78.9 | 20 | normal/on-study | t(p1;q3) |
| elongation of 5q | |||||||
| 25 | 23 | M | MDS/AML | 35 | 1 | not done | monosomy 7 |
| trisomy 21 | |||||||
| 26 | 18 | M | AML | 2 | 3.5 | not done | t(9;11) |
| 27 | 13 | M | MDS/AML | 59.8 | 16 | not done | monosomy 7 |
| trisomy 21 | |||||||
| 28 | 10 | F | MDS | 72 | — | not done | monosomy 7 |
| 29 | 2 | F | AML | 20 | 13 | normal | del (7)(q22q36)[22] |
| del (6)(p22p25) | |||||||
| del (7)(22q36)[3] | |||||||
| 30 | 5 | M | MDS, SDS | 22 | 7 | normal | monosomy 7 |
| 31 | 16 | F | AML | 102 | 2.6 | normal/on-study | monosomy 7 |
| tetraploidy |
Includes all patients who developed MDS/AML regardless of when the event occurred in relation to G-CSF treatment. The predominant dose of G-CSF is shown.
Of the 21 patients who could be classified by the French-American-British morphology guidelines for MDS and AML, 1 patient was classified as MDS refractory anemia with excess blasts (RAEB); 1 patient, MDS RAEB in transformation (T); 4 patients, AML M1; 3 patients, AML M2; 9 patients, AML M4; 2 patients, AML M7; and 1 patient, “basophilic leukemia.”
Conversion to MDS/AML was associated with diverse marrow cell cytogenetic abnormalities reflecting the malignant clonal disease (Table 3). Of the 30 patients who were studied, 28 had abnormal chromosomal changes: A partial or complete loss of chromosome 7 (7q− or monosomy 7) was noted in 18 patients. Abnormalities of chromosome 21 (usually trisomy 21 [n = 6]) were noted in 9 patients. This was often detected in conjunction with the aberrant chromosome 7 alterations. None of the patients who were tested prior to G-CSF therapy showed abnormal marrow cytogenetic changes.
Cytogenetic abnormalities without MDS/AML
In addition to the 31 patients with MDS/AML, the SCNIR also has data on 9 patients with severe chronic neutropenia whose bone marrow shows cytogenetic clonal changes, but the patients appear to be without transformation to MDS/AML (Table4). Of these 9 patients, 5 have congenital neutropenia including 2 with SDS, 2 patients have idiopathic neutropenia, and 2 patients have cyclic neutropenia or a variant. Although 3 of these 9 patients have abnormalities in chromosome 7, the other cytogenetic changes are variable and show no consistent pattern. None of the patients had abnormal cytogenetic studies prior to G-CSF therapy. These patients were observed for 2.5-86 months after the initial abnormal cytogenetic finding without further evidence of MDS/AML. There is no apparent relationship between onset of clonal changes, patient age, gender, or dose and duration of G-CSF therapy. The 2 patients with SDS and monosomy 7 received a bone marrow transplantation.
Nine patients with severe chronic neutropenia receiving G-CSF therapy with clonal cytogenetic abnormalities but not malignant myeloid transformation
| Type of neutropenia . | Age, y sex . | G-CSF dose,4-150 μg/kg/d . | Duration of G-CSF at detection of abnormality, mo . | Prior cytogenetic evaluation . | Cytogenetic abnormality . | Treatment . | Length of follow-up after abnormality detected, mo . |
|---|---|---|---|---|---|---|---|
| Idiopathic | 67 F | 3.0 | 19.2 | normal | trisomy 8 | G-CSF discontinued | 74 |
| Congenital | 10 F | 3.5 | 48.5 | normal | inv(5)(q13q31) | G-CSF prn for infections | 65 |
| Cyclic | 11 F | 6.0 | 41.9 | normal | monosomy 21 inv(8) | G-CSF continued | 53 |
| Congenital | 11 F | 22.5 | 75.6 | normal | t(x;5)(q13;q35) | G-CSF continued | 37 |
| SDS | 12 M | 5.0 | 58.6 | normal | del(7)(q22q34) | G-CSF discontinued; BMT | 44 |
| SDS | 7 F | 16.0 | 70.3 | normal | monosomy 7 t(6;13)(q21;q32) | G-CSF continued; BMT | Expired 6 mo after diagnosis (sepsis post-BMT) |
| Idiopathic | 76 M | 2.4 | 75.5 | normal | del(11)(q23) | G-CSF continued; subsequent evaluation, normal karyotype | 26 |
| Congenital | 37 M | 2.4 | 90.8 | normal | monosomy 7 add(18)(p11) | G-CSF discontinued 2.5 mo after finding | 24 |
| Congenital | 8 F | 6.0 | 64.0 | normal | 5 q(−) | G-CSF continued | 2.5 |
| Type of neutropenia . | Age, y sex . | G-CSF dose,4-150 μg/kg/d . | Duration of G-CSF at detection of abnormality, mo . | Prior cytogenetic evaluation . | Cytogenetic abnormality . | Treatment . | Length of follow-up after abnormality detected, mo . |
|---|---|---|---|---|---|---|---|
| Idiopathic | 67 F | 3.0 | 19.2 | normal | trisomy 8 | G-CSF discontinued | 74 |
| Congenital | 10 F | 3.5 | 48.5 | normal | inv(5)(q13q31) | G-CSF prn for infections | 65 |
| Cyclic | 11 F | 6.0 | 41.9 | normal | monosomy 21 inv(8) | G-CSF continued | 53 |
| Congenital | 11 F | 22.5 | 75.6 | normal | t(x;5)(q13;q35) | G-CSF continued | 37 |
| SDS | 12 M | 5.0 | 58.6 | normal | del(7)(q22q34) | G-CSF discontinued; BMT | 44 |
| SDS | 7 F | 16.0 | 70.3 | normal | monosomy 7 t(6;13)(q21;q32) | G-CSF continued; BMT | Expired 6 mo after diagnosis (sepsis post-BMT) |
| Idiopathic | 76 M | 2.4 | 75.5 | normal | del(11)(q23) | G-CSF continued; subsequent evaluation, normal karyotype | 26 |
| Congenital | 37 M | 2.4 | 90.8 | normal | monosomy 7 add(18)(p11) | G-CSF discontinued 2.5 mo after finding | 24 |
| Congenital | 8 F | 6.0 | 64.0 | normal | 5 q(−) | G-CSF continued | 2.5 |
Indicates predominant dose given.
Transformation risk versus duration of therapy
A crucial issue is whether long-term administration of G-CSF therapy for congenital neutropenia increases the risk of transformation to MDS/AML. To address this issue, we performed a life table analysis of the malignant conversions and analyzed, year to year, 31 patients who received G-CSF therapy (Table 5). Table 5 shows the total number of patients who received G-CSF therapy at the start of each time interval (for example n = 352 for the first yearly interval), the “effective” number of patients at risk of MDS/AML for each interval (after adjusting for those patients who did not complete the interval for reasons other than leukemia), and the number of patients developing MDS/AML in that interval. This information allows generation of the statistical parameters shown in Table 5 including the hazard rate or percent of MDS/AML patients as determined by numerator (n, the number of patients with MDS/AML) over the denominator (“effective” n at risk) times 100.
Life table analysis of malignant transformation in a cohort of 352 patients with congenital neutropenia
| Interval, y . | Patients at onset (without MDS/AML) . | Patients censored . | Patients at risk of MDS/AML . | Patients with MDS/AML . | Proportion of MDS/AML . | Cumulative proportion without MDS/AML (standard error) . | Hazard rate, % . |
|---|---|---|---|---|---|---|---|
| 0-1 | 352 | 45 | 329.5 | 3 | 0.0091 | 1.000 | 0.9 |
| (0.0000) | |||||||
| 1-2 | 303 | 42 | 282 | 2 | 0.0071 | 0.9909 | 0.7 |
| (0.0052) | |||||||
| 2-3 | 259 | 29 | 244.5 | 3 | 0.0123 | 0.9838 | 1.2 |
| (0.0072) | |||||||
| 3-4 | 227 | 28 | 214 | 3 | 0.0141 | 0.9718 | 1.4 |
| (0.0099) | |||||||
| 4-5 | 196 | 27 | 182.5 | 5 | 0.0274 | 0.9581 | 2.7 |
| (0.0125) | |||||||
| 5-6 | 164 | 17 | 155.5 | 1 | 0.0064 | 0.9318 | 0.6 |
| (0.0168) | |||||||
| 6-7 | 146 | 24 | 134 | 6 | 0.0448 | 0.9258 | 4.4 |
| (0.0177) | |||||||
| 7-8 | 116 | 41 | 95.5 | 3 | 0.0314 | 0.8844 | 3.1 |
| (0.0237) | |||||||
| 8-9 | 72 | 22 | 59 | 5 | 0.0847 | 0.8566 | 8.4 |
| (0.0278) | |||||||
| 9-10 | 41 | 35 | 23.5 | 0 | 0.000 | 0.7840 | 0.0 |
| (0.0402) | |||||||
| 10-11 | 6 | 6 | 3 | 0 | 0.000 | 0.7840 | 0.0 |
| (0.0402) |
| Interval, y . | Patients at onset (without MDS/AML) . | Patients censored . | Patients at risk of MDS/AML . | Patients with MDS/AML . | Proportion of MDS/AML . | Cumulative proportion without MDS/AML (standard error) . | Hazard rate, % . |
|---|---|---|---|---|---|---|---|
| 0-1 | 352 | 45 | 329.5 | 3 | 0.0091 | 1.000 | 0.9 |
| (0.0000) | |||||||
| 1-2 | 303 | 42 | 282 | 2 | 0.0071 | 0.9909 | 0.7 |
| (0.0052) | |||||||
| 2-3 | 259 | 29 | 244.5 | 3 | 0.0123 | 0.9838 | 1.2 |
| (0.0072) | |||||||
| 3-4 | 227 | 28 | 214 | 3 | 0.0141 | 0.9718 | 1.4 |
| (0.0099) | |||||||
| 4-5 | 196 | 27 | 182.5 | 5 | 0.0274 | 0.9581 | 2.7 |
| (0.0125) | |||||||
| 5-6 | 164 | 17 | 155.5 | 1 | 0.0064 | 0.9318 | 0.6 |
| (0.0168) | |||||||
| 6-7 | 146 | 24 | 134 | 6 | 0.0448 | 0.9258 | 4.4 |
| (0.0177) | |||||||
| 7-8 | 116 | 41 | 95.5 | 3 | 0.0314 | 0.8844 | 3.1 |
| (0.0237) | |||||||
| 8-9 | 72 | 22 | 59 | 5 | 0.0847 | 0.8566 | 8.4 |
| (0.0278) | |||||||
| 9-10 | 41 | 35 | 23.5 | 0 | 0.000 | 0.7840 | 0.0 |
| (0.0402) | |||||||
| 10-11 | 6 | 6 | 3 | 0 | 0.000 | 0.7840 | 0.0 |
| (0.0402) |
The number of patients censored indicates the number of patients starting the year interval but not yet completing it. The number of effective patients at risk indicates that n is the number of patients who start, minus one-half n censored. The assumption is that half of n censored do not reach the half-year point. The proportion of MDS/AML indicates the number of patients with MDS/AML divided by the effective n at risk. Hazard rate indicates the number of patients with MDS/AML divided by the effective n at risk times 100.
As shown in Table 5, the number of patients with MDS/AML and the resultant hazard rates are fairly uniform for each time span, less than 2% per year, except for an apparent increase in year 4 to 5 (hazard rate, 2.7%), in year 6 to 7 (hazard rate, 4.4%), and in year 8 to 9 (hazard rate, 8.4%). The meaning of these 3 increases is not clear because the pattern was not reproduced in the yearly interval immediately following the designated year. The hazard rates may give the appearance of increasing with time, and as a result, we conducted a review of the 95% confidence intervals for each yearly time span. The results show that each estimate either includes zero or was sufficiently close to zero. These results support the conclusion that the increases observed were seemingly apparent, but they were not real and were most likely due to the changes in sample size.
Transformation risk versus patient age
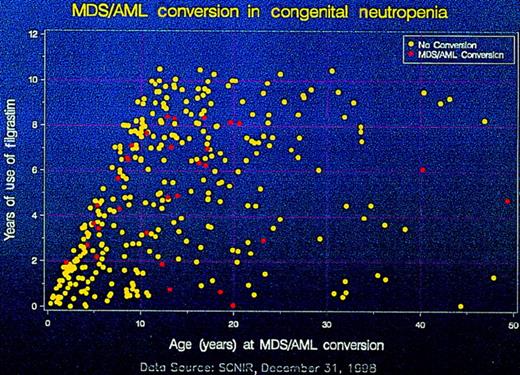
To determine if improved patient survival allows more time for expression of an underlying propensity for MDS/AML, a graphic plot was prepared showing the duration of G-CSF therapy versus the age of patients who did and did not develop malignant transformation (Figure1). The proportion of patients with MDS/AML within each 10-year age increment and 2-year period of G-CSF exposure is shown. The distribution of malignant events was random and without clustering during the years of therapy with G-CSF. Life table analyses of the time to MDS/AML conversion compared with patient ages showed that the 10- to 20-year-old patients had a greater proportion of malignant transformation (16 patients) than either the 0- to 9-year-old group (11 patients) or the 20- to 29-year-old group (2 patients). In the 40- to 49-year-old group, we observed 2 patients, but there were no patients found in the 30- to 39-year-old group. Among the 10- to 20-year-old group, 3 of 4 patients developing MDS/AML did so during clinical trials and were retrospectively found to have documented evidence of leukemic conversion prior to G-CSF initiation. These cases have been considered part of the natural background rate of leukemic conversion among patients with congenital neutropenia.
The duration of treatment with G-CSF pictured in a graphic plot and sectioned into yearly intervals versus patients' ages in 10-year intervals.
The 31 patients with MDS/AML are represented by red circles, and those who did not transform to MDS/AML are represented by yellow circles.
The duration of treatment with G-CSF pictured in a graphic plot and sectioned into yearly intervals versus patients' ages in 10-year intervals.
The 31 patients with MDS/AML are represented by red circles, and those who did not transform to MDS/AML are represented by yellow circles.
Finally, a Cox proportional hazards model analysis was used to assess the univariate impact of years of G-CSF treatment on patient ages at the time of MDS/AML conversion. The effect of years of G-CSF treatment was not significant when the model was assessed with all 352 congenital neutropenia patients (P = .57).
Discussion
G-CSF has had a major impact on the management of severe chronic neutropenia and has established itself as the first choice of treatment for this heterogeneous group of disorders. After 10 years of clinical use, it is clear that more than 90% of patients have benefited substantially in terms of a well-documented improved quality of life with less infection, inflammation, and oropharyngeal ulcers; less antibiotic use and hospitalization; and improved survival.25-27
The beneficial effect of G-CSF therapy has been most evident in the management of severe congenital forms of neutropenia, especially the subgroup of Kostmann's syndrome. In these congenital neutropenias, defective marrow granulopoiesis can be profound and can predispose a patient to life-threatening bacterial sepsis. A review of published cases, for example, showed that 42% of the patients died in the precytokine era, at an average age of 2 years, due to overwhelming pneumonia or septicemia.10 The SCNIR data on 352 patients with congenital neutropenia shows that severe bacterial complications have been almost completely eliminated in more than 90% of patients with G-CSF therapy, and death from sepsis is now a very unusual, if not rare, event. Thus, the natural history of congenital neutropenia has been sharply altered by G-CSF therapy. These patients have a vastly improved survival and are living longer.
The phenomenon of malignant myeloid transformation in some patients with congenital neutropenia has understandably dampened the euphoria of the therapeutic success. Through the efforts of the SCNIR Scientific Advisory Board, the evolution from neutropenia to MDS/AML in patients with congenital disease has been catalogued carefully and brought to the attention of treating physicians, patients, and families by way of newsletters, booth exhibits at pertinent meetings, and oral presentations.17 Predictably, there is dismay and concern about the malignant conversion and its relationship, if any, to G-CSF therapy. This issue has prompted us at the SCNIR to meticulously examine possible factors that may be operative in the development of MDS/AML.
First, conversion to MDS/AML must be considered in light of the underlying primary problem. It is well known that many of the inherited bone marrow failure syndromes have a propensity to evolve into MDS and/or AML,28 and this background of malignant predisposition in patients with congenital neutropenia has been well documented in a few cases.4-7 However, prior to the availability of G-CSF therapy, the true risk of patients with congenital neutropenia developing MDS/AML was never defined. A clearer understanding of the natural history and incidence of MDS/AML in SDS is known because many patients have milder forms of neutropenia and survive the disease long-term without the need for G-CSF treatment. Recent information suggests that the incidence of malignant transformation in these patients with SDS may be as high as 30%.8 9 Thus, any analysis of factors that may play a role in malignant conversion must be weighed against this historical background for leukemic predisposition.
In the analysis described herein, the evolution to MDS/AML was associated with a fairly distinctive clinical and laboratory profile. After starting G-CSF therapy and remaining on treatment for varying durations, a subgroup of patients developed malignant myeloid transformation in association with one or more cellular genetic changes. Many of these changes were repetitive and somewhat predictable. Of the 31 patients who developed transformations, 18 patients acquired a partial or complete loss of chromosome 7 in marrow cells, and 9 patients showed abnormalities of chromosome 21; often, both of these situations occurred together in the same patient. We showed previously that none of the patients tested prior to starting G-CSF therapy had chromosome 7 alterations.29 After development of MDS/AML, activating ras oncogene mutations were also identified retrospectively, but not at baseline, in 5 of 10 patients from our series.29 Of the 5 patients, 4 had monosomy 7. The ras mutations were all similar, with GGT (glycine) to GAT (aspartic acid) substitutions at codon 12. Marrow cells from the 5 patients with MDS/AML also showed point mutations in the gene for the G-CSF receptor, therefore resulting in a truncated C-terminal cytoplasmic region of the receptor, which is crucial for maturation signaling.30-32 There were 20 patients without receptor mutations who showed no evidence of progression to MDS/AML, and 4 additional patients were identified with mutations but without MDS/AML.33 The receptor mutations are acquired and are not the cause of congenital neutropenia.31 These patients and the ones with clonal cytogenetic changes but without MDS/AML (Table 4) are currently being monitored closely for early signs of transformation. The chromosome and molecular abnormalities must be operative in the pathogenesis of MDS/AML because they are so repetitive, but this requires further study.
The acquired marrow cytogenetic clonal abnormalities shown in Table 4are of great interest, but they are puzzling. None of the patients had these alterations prior to starting G-CSF therapy, and, therefore, the change was acquired and detected between 19 months and 7.5 years after being on therapy. Clonal changes usually signify malignant transformation, yet none of these patients have developed MDS/AML. One of the patients with trisomy 8 has been monitored for more than 6 years and has remained in good health. Note also that not all of these patients have congenital neutropenia, the only diagnostic category thus far in which MDS/AML has been observed.
What is the role of G-CSF in the conversion of congenital neutropenia to MDS/AML? Can G-CSF be considered leukemogenic? Does it accelerate the overt development of an underlying preleukemic or leukemic predisposition? From the data presented herein, there was no definitive evidence that either the dose of G-CSF or the duration of G-CSF therapy were directly related to the malignant transformation. Similarly, there was no apparent relationship to age, gender, or any other demographic factors that could be linked to the development of MDS/AML. However, these data do not completely “exonerate” G-CSF as a direct contributor in the pathogenesis. The data thus far are unclear about this, and further monitoring is needed to clarify the issue.
Regarding G-CSF as a carcinogen, it would be unexpected for G-CSF to break molecular bonds and cause DNA damage. In well-defined, treatment-related cases of secondary MDS/AML due to chemotherapy for a primary disorder, there is also always a lag phase between the drug exposure and the malignant event. For example, the risk of alkylating agent-related leukemia begins to increase 2 years after the start of chemotherapy and peaks in the 5-10 year follow-up. Similarly, etoposide-related AML has a median 2- to 3-year lag phase following its therapeutic use. In the 0- to 1-year interval of G-CSF therapy, there were 3 conversions to MDS/AML at varying times within the first 12 months of treatment (Table 5). Thus, the customary lag phase expected for treatment-induced MDS/AML is not apparent; however, it is unknown if longer follow-up will disclose a pattern similar to chemo-induced MDS/AML. Thus far, the hazard rate appears flat, but this could change, and it requires careful long-term surveillance. It seems highly unlikely at this point, though, that G-CSF is directly leukemogenic. It may be operative in facilitating transformation in other ways yet to be defined.
It is notable that MDS/AML has not been diagnosed in any of the other patients with cyclic neutropenia or idiopathic neutropenia who are enrolled in the SCNIR and have been treated with G-CSF for the same duration of time. If the cytokines were contributing to the development of MDS/AML, one might expect to see cases in these other diagnostic categories, as well. However, it must be acknowledged that these disorders are heterogeneous and have varying leukemogenic potential. Thus, it is not clear from our data that the potential, if any, for G-CSF therapy to exacerbate a leukemic predisposition would be the same for each of these types of neutropenias.
Patients with congenital neutropenia who respond well to G-CSF therapy have been observed to develop MDS/AML associated with recurrent acquired patterns of cellular genetic changes, singly or in combination. Although the exact sequence of events is unclear, the change seemingly begins with a genetic lesion that causes the congenital neutropenia, which then evolves into G-CSF–receptor mutations, monosomy 7, ras oncogene mutations, and finally overt malignant disease. We could not identify any specific factors that could be implicated in promoting MDS/AML. We conclude that G-CSF improves survival of patients with congenital neutropenia, and with improved survival, the underlying leukemic propensity that characterizes this disorder becomes unmasked. On the other hand, our data have not excluded a direct contribution of G-CSF in the pathogenesis. In this regard, it is possible that G-CSF allows abnormal malignant cellular clones to proliferate excessively and survive. In addition, G-CSF may confer a growth advantage on these cells, especially after the myeloid cells acquire mutations of the G-CSF receptor.34 35 Currently, G-CSF is still deemed specific therapy for all forms of severe chronic neutropenia and still offers a high margin of safety. It should be the initial treatment for this family of disorders. However, careful surveillance and serial monitoring of clinical, hematological, and cytogenetic parameters are urged.
Note added in proof. The data presented in this manuscript were analyzed up to a cut-off date of December 31, 1998. Between January 1, 1999, and December 31, 1999, 36 additional patients with congenital neutropenia were enrolled in the Registry, thereby increasing the total number to 388. During the same time interval, there were 4 new cases of MDS/AML. Thus. the new, overall incidence or crude rate of MDS/AML conversion is 9.0% (35 cases among 388 patients taking G-CSF). This new crude rate is not statistically different than that of 8.8% quoted in the manuscript. Furthermore, when the new data were added to Tables 1, 2, and 5 and reanalyzed statistically, there were no significant differences compared to the analysis in the manuscript. Therefore, the data interpretation and conclusions based on the new information are virtually identical to those presented in the paper.
Acknowledgments
We thank all of our colleagues and friends associated with the Data Collection Centers of the Severe Chronic Neutropenia International Registry at the University of Washington, Seattle, WA, and the Medizinische Hochschule, Hannover, Germany. We are also grateful to the many physicians worldwide who have faithfully and generously submitted data on their patients.
The Severe Chronic Neutropenia International Registry, Seattle, WA, is funded by Amgen Inc, Boulder, CO, and Thousand Oaks, CA.
Reprints:Melvin H. Freedman, Division of Hematology/Oncology, The Hospital for Sick Children, 555 University Ave, Toronto, Ontario, Canada M5G 1X8; e-mail:melvin.freedman@sickkids.on.ca.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal