Abstract
Secreted phospholipase A2 (sPLA2) regulates a variety of cellular functions. The present investigation was undertaken to elucidate the potential role of sPLA2 in endothelial cell (EC) migration. Bovine aortic endothelial cells (BAECs) exposed to sPLA2 placed in the lower compartment of a modified Boyden chamber displayed increased migration compared to cells exposed to vehicle. The effect of sPLA2 on EC migration was time and dose dependent. Migration of BAECs was observed at 30 minutes, increased over 1 to 2 hours, and declined thereafter. At 2 hours of stimulation, sPLA2 (0.01-2 μmol/L) induced 1.2- to 3-fold increased cell migration compared with media alone. Among the different sPLA2s tested, bee venom, Naja naja, and porcine and human pancreatic PLA2s all evoked a migratory response in ECs. Moreover, human synovial fluid, obtained from patients with arthritis and containing sPLA2 activity, induced EC migration. Migration of ECs was significantly reduced after exposure to a catalytic site mutant of pancreatic sPLA2with decreased lipolytic activity as compared to wild-type sPLA2. Similarly, pretreatment of human synovial fluid withp-bromophenacyl bromide, an irreversible inhibitor of sPLA2, markedly decreased the ability of human synovial fluid to stimulate EC migration. Moreover, migration of ECs was stimulated on exposure to hydrolytic products of sPLA2activity including arachidonic acid, lysophosphatidic acid, and lysophosphatidylcholine. These findings suggest that sPLA2plays a physiologic role in induction of EC migration. Moreover, the effects of sPLA2 on EC migration are mediated, at least in part, by its catalytic activity.
Introduction
Phospholipases A2 (PLA2;phosphatidylcholine-2-acylhydrolase, EC 3.1.1.4) represent a large family of lipolytic enzymes that catalyze the hydrolysis of the sn-2 fatty acyl ester bond of membrane glycero-3-phospholipids to release free fatty acids and lysophospholipids such as arachidonic acid (AA) and lysophosphatidic acid (LPA).1 PLA2 can be classified into several groups based on cellular localization, amino acid sequence, molecular mass, and calcium requirement for enzymatic activity.1 The extracellular or secreted PLA2s (sPLA2) are characterized by high disulfide bridge content, low molecular mass (14-16 kd), the requirement of millimolar concentration of calcium for catalysis, and wide fatty acid selectivity in vitro.2 Several mammalian and venom sPLA2s have been identified.2-5 Group IB sPLA2 is highly expressed in porcine, bovine, and human pancreas and in other tissues.1,3 Group IIA sPLA2, also known as inflammatory-type sPLA2, is highly expressed in human synovial fluid and platelets.1,3 Group III sPLA2, mainly found in bee venom, has particular structural features.1-3 Although several studies have elucidated many of the biochemical characteristics of sPLA2s, their physiologic role remains elusive.6 Secreted PLA2s have been implicated in the regulation of a wide array of cellular functions.7-9 Moreover, elevated levels of sPLA2 have been detected in several diseases including arthritis, pancreatitis, and acute chest syndrome of sickle cell disease.10-12 Some of the effects of sPLA2 on cell function appear to be dependent on the release of bioactive mediators including fatty acids such as AA and lysophospholipids.13,14 Others may be dependent on the binding of the enzyme to specific membrane receptors.15Two types of sPLA2 receptors have been isolated with different tissue distribution and binding characteristics.16 The M-type receptor is highly expressed in skeletal muscle cells and has high affinity for the pancreatic sPLA2 and for OS1 (Oxyuranus scutellatus toxin 1), an sPLA2 isolated from the venom of the Australian taipan snake.17 The N-type receptor is expressed mostly in neuronal cells and binds with high-affinity venom sPLA2s, including bee venom and OS2 (O scutellatus toxin 2).18
Recent studies have suggested a role for sPLA2 on cell motility. Secreted PLA2 from Naja najainduced migration of a rat gastric epithelial cell (EC) line, whereas pancreatic-type sPLA2 induced migration of rat embryonic thoracic aorta smooth muscle cells.19,20 Moreover,Naja naja and pancreatic PLA2 induced migration of NIH-3T3 fibroblasts.15 Although evidence exists on the role of sPLA2 on cell motility, little is known about the effect of this enzyme on EC migration. Studies by Sa and Fox21 showed that the effect of basic fibroblast growth factor (bFGF) on wound-induced movement of ECs was markedly reduced by pharmacologic inhibition of PLA2, suggesting that bFGF-induced cell migration was mediated by PLA2activation. However, a direct effect of sPLA2 on EC migration has not yet been demonstrated.21 In this study, we present evidence that sPLA2 stimulates the migration of human and bovine ECs. Furthermore, we demonstrate that sPLA2 generated under pathophysiologic conditions in synovial fluid of patients with arthritis was also able to stimulate EC migration. These findings indicate a novel process by which sPLA2 may influence cell responses involving migration of ECs.
Materials and methods
Reagents
The EC growth medium, EC growth supplements, attachment factor,p-bromophenacyl bromide (p-BPB), and p-aminophenyl-α-d-mannopyranoside-bovine serum albumin (mannose-BSA) were purchased from Sigma (St Louis, MO). Fetal bovine serum (FBS) was purchased from Hyclone (Logan, UT). McCoy 5A modified medium was purchased from Gibco (Gaithersburg, MD). Transwell tissue culture plates were purchased from Corning Corporation (Cambridge, MA). Diff-Quick stain was obtained from Dada Behring (Newark, DE). Antisynovial PLA2 monoclonal antibody, sPLA2enzyme assay kit, and bromoenol lactone (BEL) were purchased from Cayman (Ann Arbor, MI). The enhanced chemiluminescence detection kit was purchased from Amersham (Arlington Heights, IL)
Phospholipase A2
The PLA2 (E.C. 3.1.1.4.) from bee venom (bvPLA2) was obtained from Sigma and was further purified using C18 reverse phase chromatography as previously described.16 PLA2 from Naja najawas obtained from Sigma. The purity of sPLA2 was confirmed by 16% sodium dodecyl sulfate (SDS) gel electrophoresis followed by Coomassie blue staining. A single band in the area of the 14-kd molecular weight marker was detected. Porcine pancreatic group IB sPLA2 (pGIB sPLA2) was purchased from Boehringer Mannheim (Indianapolis, IN) and was further purified using high-performance cation exchange liquid chromatography.22 A catalytic site mutant of pGIB sPLA2 (H48Q) was obtained in Escherichia coli as previously described.23 The catalytic activity of the H48Q variant was reduced by a factor of 105 when compared to the activity of wild-type pGIB sPLA2.23OS1 PLA2 was purified to homogeneity as previously described.24 Human recombinant pancreatic group IB sPLA2 (hGIB sPLA2) was purified to homogeneity and migrated as a single band on SDS polyacrylamide gel.22 Human recombinant group II sPLA2 (hGIIA sPLA2) was obtained from insect cells using the baculovirus expression system as previously described.22
Cell cultures
The majority of experiments were performed using bovine aortic endothelial cells (BAECs) purchased from Cell Systems (Kirkland, WA). Cells were serially cultured in tissue culture flasks coated with attachment factor as previously described.25 Cells were maintained in EC medium containing 10% FBS and 1% EC growth supplement at 37°C in humidified 5% CO2. In selected experiments, ECs from different tissue origins were used. Human microvascular endothelial cells (HMVECs) and bovine pulmonary artery endothelial cells (BPAECs) were purchased from Clonetics Corp (San Diego, CA) and Cell Systems, respectively. Cells were plated in attachment factor-coated flasks in RPMI medium supplemented with 10% FBS and 1% EC growth factor supplement. The ECs exhibited the typical cobblestone appearance and were used between passages 4 to 12. Human vascular smooth muscle cells (HVSMCs) were obtained from Cell Systems. Cells were maintained in medium containing 10% FBS and 1% growth factor supplement. NIH-3T3 cells were obtained from ATCC (Rockville, MD). Cells were maintained in McCoy modified medium supplemented with 10% FBS. The characteristics on the murine stromal cell line +/+.1 LDA 11 have been previously described.26
Cell migration assay
Migration of ECs was assayed by a modification of the Boyden apparatus assay described by Auerbach and coworkers,27using 24-well Transwell cell culture inserts with 8-μmol/L polycarbonate filters. Filters were coated when indicated with attachment factor, fibronectin, collagen, or 0.1% gelatin. Subconfluent BAEC cultures were washed, trypsinized to obtain single-cell suspension, and suspended in Hanks balanced salt solution (HBSS). In the standard assay, 80 μL of cell suspension containing 2.5 × 105 cells was placed in the upper compartment of the Transwell chamber. Secreted PLA2 or vehicle was placed in the lower compartment of the chamber in 0.3 mL of HBSS containing 1 mmol/L CaCl2. The chambers were incubated for different times at 37°C in a humidified incubator with 5% CO2 to allow cell migration. After the incubation period, the filter was removed, and the upper side of the filters was wiped gently with a cotton applicator to remove nonmigrated cells. The filters were fixed with methanol and stained with a Giemsa solution (Diff-Quick). Migration was quantitated by counting cells that had migrated to the lower surface of the filter. Four random fields in each filter were examined. Each experiment was performed in triplicate and migration was expressed as the average number ± SE of total cells counted per field.
Detection and measurement of secreted phopholipase A2catalytic activity in human synovial fluid
Synovial fluid was obtained from patients with arthritis by the staff of the Arthritis Care Center, Clarian Health, Indianapolis, IN. Fluids were centrifuged at 400g for 10 minutes to sediment cellular material. The resultant supernatants were assayed for levels and activity of sPLA2. To detect sPLA2,aliquots of human synovial fluid were diluted with SDS sample buffer, boiled for 5 minutes, and resolved on 16% SDS-gel electrophoresis. Proteins were transferred to nitrocellulose membranes and subjected to immunoblotting as previously described28 with a monoclonal anti-sPLA2 antibody (1:1000) that specifically recognizes synovial sPLA2. Blots were subsequently incubated for 1 hour with horseradish peroxidase–linked sheep antimouse antibody (1:4000). Human synovial sPLA2 was visualized by the enhanced chemiluminescence detection system.28 Measurement of sPLA2 activity was performed using a colorimetric assay kit from Cayman following the manufacturer's instructions. This assay uses the 1,2-dithio analog of diheptanoyl phosphatidylcholine as a substrate.29 On hydrolysis of the thio ester bond at the sn-2 position by sPLA2, free thiols are released and subsequently detected using 5,5-dithiobis(2-nitrobenzoic acid) (DTNB). Briefly, aliquots of human synovial fluid (1-15 μL) were incubated with 10 μL DTNB in a buffer containing 25 mmol/L Tris-HCl (pH 7.5), 10 mmol/L CaCl2, 100 mmol/L KCl, 0.3 mmol/L Triton-X-100, and 1 mg/ml BSA. Following addition of the substrate, sPLA2activity was monitored over a period of 15 minutes and detected by measuring the absorbance at 414 nm using a VERSAmax microplate reader (Molecular Device, Sunnyvale, CA). The reaction rate at 414 nm was determined using the DTNB extinction rate of 13.6 mmol/L per cm. Results are expressed as μmol/min.
In vitro inactivation of synovial secreted phospholipase A2
Protein determination
The protein concentration was determined by the method of Bradford using BSA as a standard.30
Statistical analysis
Results are presented as mean ± SE of at least 3 independent experiments, each performed in triplicate unless otherwise indicated. Results were statistically evaluated using the Student ttest. Differences between means yielding P values of less than .05 were considered statistically significant.
Results
Effect of secreted phospholipase A2 on endothelial cell migration
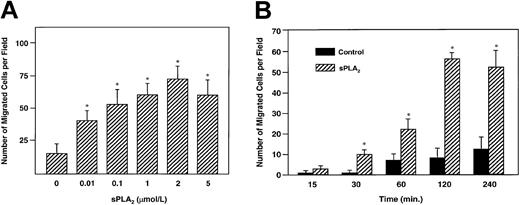
Using 24-well Transwell chambers, we first assessed the migratory response of BAECs to increasing concentrations of bvPLA2 (0.01-2 μmol/L). FBS was used, when indicated, as a positive control. The bvPLA2, added to the lower compartment of the modified chemotaxis chamber, induced a significant increase of EC migration in a dose-dependent fashion compared to migration of cells exposed to vehicle alone (Figure1A). A 1.2-fold increase of migration was detected in cells stimulated with 0.01 μmol/L bvPLA2compared to vehicle-treated cells. Challenge of ECs with bvPLA2 further increased migration over unstimulated cells from 1.8- to 3.0-fold at concentrations of 0.1, 1, and 2 μmol/L, respectively (Figure 1A). Higher concentrations of bvPLA2(5 μmol/L) were ineffective in inducing any further increase of EC migration (Figure 1A).
Stimulation of EC migration by sPLA2: dose response
. (A) BAECs (2.5 × 105) were placed in the upper compartment of a Transwell chamber. Varying concentrations of bvPLA2 were placed in the lower compartment. Cells were allowed to migrate for 2 hours through 8-μm pores of polycarbonate filters coated with attachment factor and placed between the upper and the lower compartment. After migration, the upper part of the filter was washed to remove nonmigrated cells and the membrane was stained using Diff-Quick. Migrated cells were quantified by counting nuclei in 4 random fields (× 10)/filter. Results are the mean ± SE of 4 independent experiments. Asterisk indicates statistically significant (P < .004 versus basal migration). (B) Stimulation of EC migration by sPLA2: time course. BAECs were placed in the upper compartment of the Transwell chamber, and bvPLA2 (1 μmol/L) was placed in the lower compartment. Migration was evaluated at the indicated times. Quantification of migrated cells was performed as described above. Results are the mean ± SE of 3 independent determinations. Asterisk indicates statistical significance (P < .001 basal migration).
Stimulation of EC migration by sPLA2: dose response
. (A) BAECs (2.5 × 105) were placed in the upper compartment of a Transwell chamber. Varying concentrations of bvPLA2 were placed in the lower compartment. Cells were allowed to migrate for 2 hours through 8-μm pores of polycarbonate filters coated with attachment factor and placed between the upper and the lower compartment. After migration, the upper part of the filter was washed to remove nonmigrated cells and the membrane was stained using Diff-Quick. Migrated cells were quantified by counting nuclei in 4 random fields (× 10)/filter. Results are the mean ± SE of 4 independent experiments. Asterisk indicates statistically significant (P < .004 versus basal migration). (B) Stimulation of EC migration by sPLA2: time course. BAECs were placed in the upper compartment of the Transwell chamber, and bvPLA2 (1 μmol/L) was placed in the lower compartment. Migration was evaluated at the indicated times. Quantification of migrated cells was performed as described above. Results are the mean ± SE of 3 independent determinations. Asterisk indicates statistical significance (P < .001 basal migration).
The effect of bvPLA2 on EC migration was time dependent. A significant increase of EC migration (P < .001) was detected after 30 minutes of exposure of BAECs to bvPLA2. The maximum effect on cell migration was observed after 1 to 2 hours of stimulation with bvPLA2 and declined thereafter (Figure1B). The standard migration assays were performed using attachment factor–coated filters. No differences on bvPLA2-induced cell migration were found when filters were coated with 0.1% gelatin, collagen, or fibronectin (data not shown).
To distinguish between chemotaxis (directional cell movement) and chemokinesis (random cell movement), checkerboard analyses were performed. In these experiments, BAECs were placed in the upper compartment of the chamber, and bvPLA2 at concentrations of 1 and 2 μmol/L was placed either in the lower compartment of the chamber, or in the upper compartment, or in both. As shown in Table1, significant migration was observed when bvPLA2 was present in the lower compartment, creating a concentration gradient between upper and lower compartments. When the concentration gradient was abolished by adding equal concentrations of bvPLA2 to both lower and upper compartments, no migration of ECs was detected. Similarly, the presence of bvPLA2 in the upper compartment, where ECs were placed, also abolished the migratory response of ECs to bvPLA2. Thus, a concentration gradient was required for the migratory effect of bvPLA2, suggesting that the enzyme had a chemotactic rather than a chemokinetic effect on BAECs.
Checkerboard analysis of BAECs in response to sPLA2
| sPLA2 in lower compartment (μmol/L) . | sPLA2 in upper compartment (μmol/L) . | ||
|---|---|---|---|
| 0 . | 1 . | 2 . | |
| 0 | 25 ± 2 | 28 ± 1 | 30 ± 4 |
| 1 | 57 ± 5 | 25 ± 2 | 26 ± 7 |
| 2 | 79 ± 3 | 58 ± 8 | 31 ± 6 |
| sPLA2 in lower compartment (μmol/L) . | sPLA2 in upper compartment (μmol/L) . | ||
|---|---|---|---|
| 0 . | 1 . | 2 . | |
| 0 | 25 ± 2 | 28 ± 1 | 30 ± 4 |
| 1 | 57 ± 5 | 25 ± 2 | 26 ± 7 |
| 2 | 79 ± 3 | 58 ± 8 | 31 ± 6 |
Various concentrations of bvPLA2 were placed in the upper and/or lower compartment as indicated. Cells were placed in the upper compartment of the Transwell chamber and allowed to migrate for 2 hours at 37°C and 5% CO2. Migration was quantified by counting the number of cells that migrated to the lower side of the polycarbonate membrane containing 8-μm pores. Numbers represent mean ± SE of 4 low-power fields (10 ×) from 3 wells.
Tissue, cell type, and group specificity of secreted phospholipase A2–induced endothelial cell migration
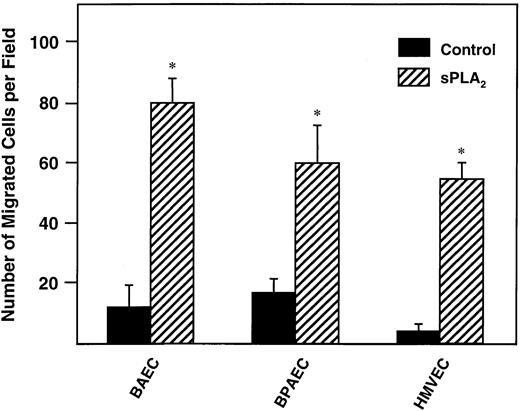
To investigate the tissue specificity of the bvPLA2-dependent migratory response, ECs from different tissues were tested for their ability to migrate toward the enzyme. BAECs, BPAECs, and HMVECs (2.5 × 105) were placed on the upper compartment of the Transwell chamber and exposed to 1 μmol/L bvPLA2 for 2 hours. As shown in Figure2, all of the ECs tested migrated when exposed to bvPLA2. The maximum effect of bvPLA2on EC motility was observed in BAECs followed by HMVECs and BPAECs. The effect of bvPLA2 was examined on NIH-3T3 fibroblasts and HVSMCs to establish cell-type specificity. NIH-3T3 cells also migrated following exposure to bvsPLA2 (data not shown). No effect of the enzyme was detected on migration of HVSMCs (data not shown). Thus, although ECs from different tissue origins all migrated following stimulation with sPLA2, the effect of the enzyme was cell-type specific.
Tissue specificity of sPLA2-induced EC migration.
BAECs, HMVECs, and BPAECs were placed in the upper compartment of a Transwell chamber, and bvPLA2 (1 μmol/L) was placed in the lower compartment. Migration was allowed to occur for 2 hours at 37°C and 5% CO2. Filters were removed and nonmigrated cells were scraped off. Filters were stained using Diff-Quick. Nuclei from 4 random power fields (× 10)/filter were counted. Bars indicate the mean ± SE of 3 independent experiments. Asterisk indicates statistical significance (P < .01 versus basal migration).
Tissue specificity of sPLA2-induced EC migration.
BAECs, HMVECs, and BPAECs were placed in the upper compartment of a Transwell chamber, and bvPLA2 (1 μmol/L) was placed in the lower compartment. Migration was allowed to occur for 2 hours at 37°C and 5% CO2. Filters were removed and nonmigrated cells were scraped off. Filters were stained using Diff-Quick. Nuclei from 4 random power fields (× 10)/filter were counted. Bars indicate the mean ± SE of 3 independent experiments. Asterisk indicates statistical significance (P < .01 versus basal migration).
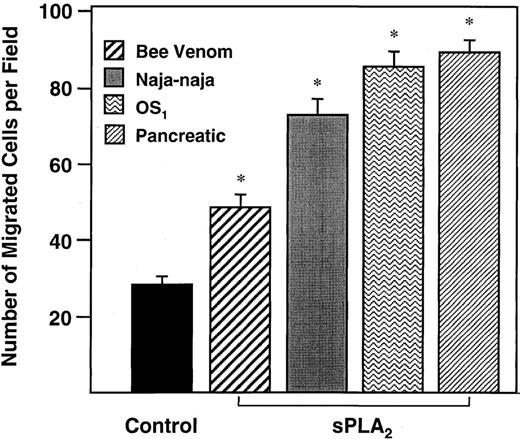
We next examined the effect of distinct sPLA2s on EC migration. In these experiments the effect of bvPLA2 on cell migration was compared to that of sPLA2 fromNaja naja, pGIB sPLA2, and OS1. Cells were exposed to sPLA2 (0.5 μmol/L) for 2 hours prior to assessment of migration. As shown in Figure3, bee venom, Naja naja, OS1, and pGIB sPLA2s evoked 0.9-, 1.8-, 2.3-, and 2.4-fold increases in BAEC migration, respectively.
Effect of different sPLA2s on EC migration.
BAECs were seeded in the upper compartment of a Transwell chamber. Bee venom sPLA2, Naja naja sPLA2, porcine pancreatic sPLA2, and OS1 (0.5 μmol/L each) were placed in the lower compartment. Cells that migrated after 2 hours of incubation at 37°C and 5% CO2 were stained. Nuclei from 4 random fields (× 10)/filter were counted. Results are the mean ± SE of the number of migrated cells per field from 3 independent determinations. Asterisk indicates statistical significance (P < .001 versus basal migration).
Effect of different sPLA2s on EC migration.
BAECs were seeded in the upper compartment of a Transwell chamber. Bee venom sPLA2, Naja naja sPLA2, porcine pancreatic sPLA2, and OS1 (0.5 μmol/L each) were placed in the lower compartment. Cells that migrated after 2 hours of incubation at 37°C and 5% CO2 were stained. Nuclei from 4 random fields (× 10)/filter were counted. Results are the mean ± SE of the number of migrated cells per field from 3 independent determinations. Asterisk indicates statistical significance (P < .001 versus basal migration).
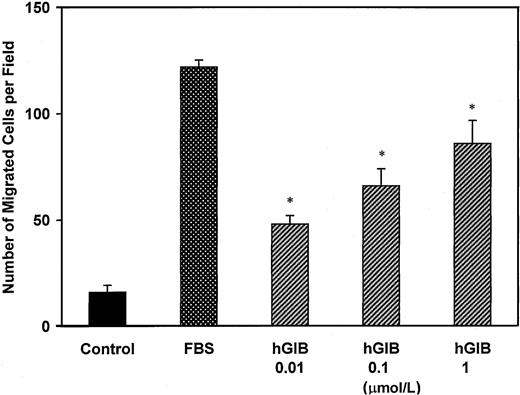
Effect of human secreted phospholipase A2 on bovine aortic endothelial cell migration
We examined the migratory response of BAECs following exposure to human sPLA2. For this purpose, hGIB sPLA2, purified as previously described,22 was used. BAECs, placed in the upper compartment of the Boyden chamber, were stimulated with various concentrations of hGIB sPLA2 (0.01-1 μmol/L) for 2 hours at 37°C and 5% CO2. As shown in Figure4, hGIB sPLA2 induced a dose-dependent increase of BAEC migration (from 3- to 5.3-fold increase over control). Similarly, hGIIA sPLA2 (0.1 μmol/L) induced a 4-fold increase of BAEC migration (data not shown).
Effect of human sPLA2 on EC migration.
BAECs were placed in the upper compartment of the Transwell chamber and increasing concentrations of human pancreatic group IB sPLA2 (hGIB sPLA2, 0.01-1 μmol/L) were added in the lower compartment. Migration was evaluated at 2 hours of incubation at 37°C. Migrated cells were stained and quantified by counting nuclei in 4 random fields (× 10)/filter. FBS (10%) was used as a positive control. Bars represent the mean ± SE of triplicate determinations. Similar results were obtained in 3 independent experiments. Asterisk indicates statistical significance (P < .001 versus hGIB sPLA2-induced migration); FBS, fetal bovine serum; hGIB, human pancreatic group IB sPLA2.
Effect of human sPLA2 on EC migration.
BAECs were placed in the upper compartment of the Transwell chamber and increasing concentrations of human pancreatic group IB sPLA2 (hGIB sPLA2, 0.01-1 μmol/L) were added in the lower compartment. Migration was evaluated at 2 hours of incubation at 37°C. Migrated cells were stained and quantified by counting nuclei in 4 random fields (× 10)/filter. FBS (10%) was used as a positive control. Bars represent the mean ± SE of triplicate determinations. Similar results were obtained in 3 independent experiments. Asterisk indicates statistical significance (P < .001 versus hGIB sPLA2-induced migration); FBS, fetal bovine serum; hGIB, human pancreatic group IB sPLA2.
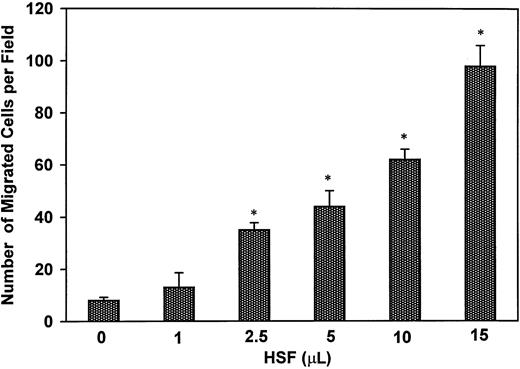
To evaluate the physiologic relevance of the migratory response detected on exposure of ECs to human sPLA2s, we tested the ability of human synovial fluid, obtained from patients with arthritis, to induce BAEC migration in the Boyden assay. Increased levels and activity of hGIIA sPLA2 have been detected in the synovial fluid of patients with rheumatoid arthritis.31 BAECs were exposed to increasing concentrations of human synovial fluid (1, 2.5, 5, 10, and 15 μL corresponding to 5.5, 13.7, 27.5, 55, and 82.5 μg of total protein content) placed in the lower compartment of the Boyden chamber for 2 hours at 37°C. Exposure of ECs to human synovial fluid induced a vigorous, dose-dependent migratory response (Figure5).
Effect of human synovial fluid on EC migration.
BAECs were placed on the upper compartment of a Transwell chamber. Various amounts of human synovial fluid (1-15 μL) were placed in the lower compartment containing 0.3 mL of HBSS medium. Migration assay was performed for 2 hours at 37°C. Migrated cells were quantitated by counting nuclei from 4 random fields (× 10)/filter as described above. Bars represent the mean ± SE of 3 independent experiments. Asterisk indicates statistical significance (P < .001 versus control, with no added human synovial fluid); HSF, human synovial fluid.
Effect of human synovial fluid on EC migration.
BAECs were placed on the upper compartment of a Transwell chamber. Various amounts of human synovial fluid (1-15 μL) were placed in the lower compartment containing 0.3 mL of HBSS medium. Migration assay was performed for 2 hours at 37°C. Migrated cells were quantitated by counting nuclei from 4 random fields (× 10)/filter as described above. Bars represent the mean ± SE of 3 independent experiments. Asterisk indicates statistical significance (P < .001 versus control, with no added human synovial fluid); HSF, human synovial fluid.
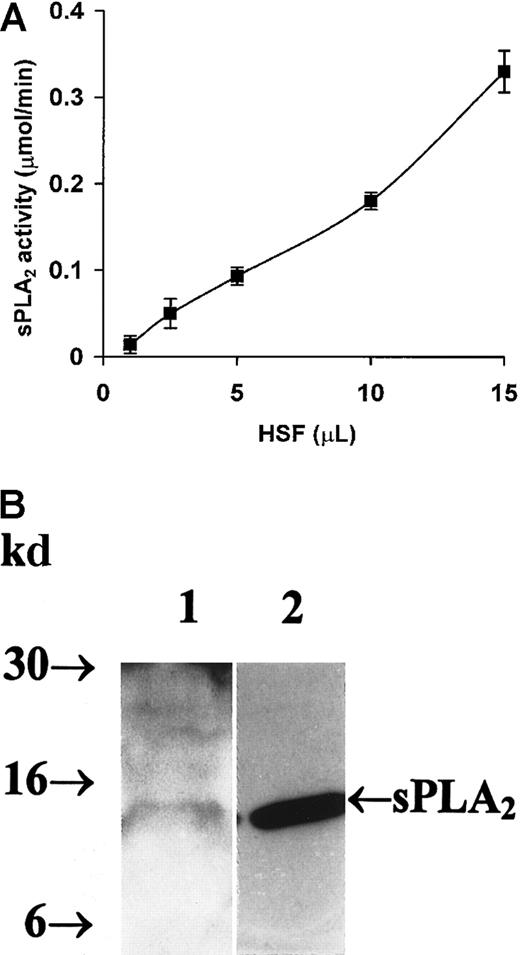
We next investigated whether the human synovial fluid used in the migration assay possessed sPLA2 activity. Aliquots of human synovial fluid (1-15 μL) were tested for sPLA2 activity with 1,2-dithio analog of diheptanoyl phosphatidylcholine as a substrate. As shown in Figure 6A, an increase of sPLA2 catalytic activity was detected with increasing concentrations of human synovial fluid. The presence of sPLA2 in the synovial fluid tested for induction of cell migration was detected by Western blot analysis (Figure 6B).
Detection of sPLA2 in human synovial fluid.
(A) Measurement of human synovial fluid sPLA2 enzyme activity. Assays to measure human synovial fluid sPLA2enzyme activity were performed as described in “Material and methods” using a 96-well microtiter plate. Enzyme activity was monitored for 15 minutes at 25°C by measuring absorbance at 414 nm. The background absorbance in the absence of added human synovial fluid was subtracted from each sample. Bee venom PLA2 (0.01 μg) was included as a positive control. Data points represent the mean ± SE from triplicate determinations of a representative experiment. HSF indicates human synovial fluid. (B) Western blotting of human synovial fluid sPLA2. Aliquots of human synovial fluid (15 μL/lane corresponding to 82.5 μg of total protein content) or purified human synovial sPLA2 (1 μg/lane) were fractionated on a 16% polyacrylamide gel and transferred to a nitrocellulose membrane. The membrane was probed with a monoclonal antisynovial sPLA2 antibody (diluted 1:1000). Antibody reactions were detected using horseradish peroxidase–conjugated sheep antimouse Ig (diluted 1:2500) and the enhanced chemiluminescence detection system. Shown on the left are molecular weight markers expressed in kilodaltons. The arrow on the right indicates the 14-kd sPLA2. Lane 1 is human synovial fluid. Lane 2 is human synovial sPLA2 that was used as a positive control.
Detection of sPLA2 in human synovial fluid.
(A) Measurement of human synovial fluid sPLA2 enzyme activity. Assays to measure human synovial fluid sPLA2enzyme activity were performed as described in “Material and methods” using a 96-well microtiter plate. Enzyme activity was monitored for 15 minutes at 25°C by measuring absorbance at 414 nm. The background absorbance in the absence of added human synovial fluid was subtracted from each sample. Bee venom PLA2 (0.01 μg) was included as a positive control. Data points represent the mean ± SE from triplicate determinations of a representative experiment. HSF indicates human synovial fluid. (B) Western blotting of human synovial fluid sPLA2. Aliquots of human synovial fluid (15 μL/lane corresponding to 82.5 μg of total protein content) or purified human synovial sPLA2 (1 μg/lane) were fractionated on a 16% polyacrylamide gel and transferred to a nitrocellulose membrane. The membrane was probed with a monoclonal antisynovial sPLA2 antibody (diluted 1:1000). Antibody reactions were detected using horseradish peroxidase–conjugated sheep antimouse Ig (diluted 1:2500) and the enhanced chemiluminescence detection system. Shown on the left are molecular weight markers expressed in kilodaltons. The arrow on the right indicates the 14-kd sPLA2. Lane 1 is human synovial fluid. Lane 2 is human synovial sPLA2 that was used as a positive control.
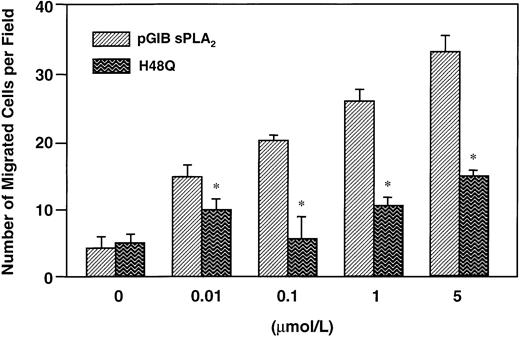
Effect of secreted phospholipase A2 catalytic activity on endothelial cell migration
We next determined whether the catalytic activity of sPLA2 was required for stimulation of EC migration. To assess the influence of sPLA2 catalytic activity on stimulation of EC migration, BAECs were exposed to equimolar concentrations of pGIB sPLA2 (wild type) or H48Q pGIB sPLA2. This latter is a variant of pGIB sPLA2in which replacement in the catalytic site of histidine by a glutamine gives rise to a protein that displays a dramatic loss of its lipolytic activity.23 As shown in Figure7, exposure of BAECs to pGIB sPLA2 induced a dose-dependent increase of cell migration. Exposure of ECs to equimolar concentrations of H48Q pGIB sPLA2 also stimulated cell migration but to a much lower degree compared to that observed with wild-type pGIB sPLA2(Figure 7). In contrast, exposure of NIH-3T3 and bone marrow stromal cells to pGIB or H48Q pGIB sPLA2 induced the same degree of EC migration (data not shown). Mannose-BSA was previously shown to bind to sPLA2 receptors22,32 and in some cases to prevent sPLA2-dependent cellular effects.33 We therefore examined whether mannose-BSA could prevent sPLA2-induced EC migration. Our results indicate that mannose-BSA, at 25 μg/mL, has no effect on pGIB sPLA2-induced BAEC migration (data not shown).
Effect of wild-type or H48Q mutant pancreatic sPLA2 on EC migration.
BAECs were placed on the upper compartment of a Transwell chamber. Wild-type porcine pancreatic sPLA2 (pGIB sPLA2) or a mutated pGIB sPLA2 (H48Q) were placed in the lower compartment of the Transwell chamber at concentrations of 1 μmol/L. Migration assay was carried out for 2 hours at 37°C. Quantitation of the migrated cells was performed by counting nuclei from 4 random fields (× 40) for each filter. Bars represent the mean ± SE from triplicate determination of a representative experiment. Asterisk indicates statistical significance (P < .001 versus wild-type pGIB sPLA2-induced migration).
Effect of wild-type or H48Q mutant pancreatic sPLA2 on EC migration.
BAECs were placed on the upper compartment of a Transwell chamber. Wild-type porcine pancreatic sPLA2 (pGIB sPLA2) or a mutated pGIB sPLA2 (H48Q) were placed in the lower compartment of the Transwell chamber at concentrations of 1 μmol/L. Migration assay was carried out for 2 hours at 37°C. Quantitation of the migrated cells was performed by counting nuclei from 4 random fields (× 40) for each filter. Bars represent the mean ± SE from triplicate determination of a representative experiment. Asterisk indicates statistical significance (P < .001 versus wild-type pGIB sPLA2-induced migration).
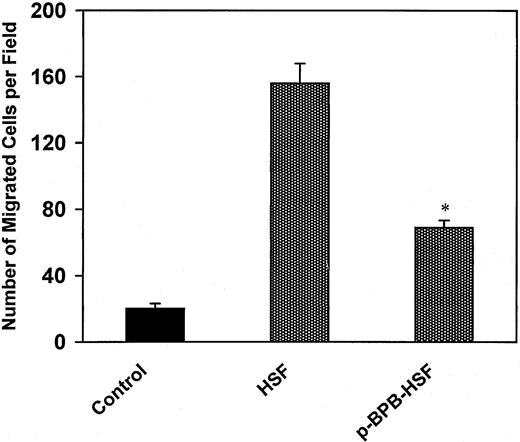
To determine whether sPLA2 activity in human synovial fluid influenced EC migration, we treated human synovial fluid with p-BPB, an irreversible inhibitor of sPLA2.34,35 This treatment induced inhibition of sPLA2 activity measured by hydrolysis of the 1,2-dithio analog of diheptanoyl phosphatidylcholine (data not shown). Human synovial fluid before or after treatment with p-BPB was assayed for induction of EC migration. As shown in Figure8 pretreatment of human synovial fluid with p-BPB induced a 56% decrease of BAEC migration compared to untreated synovial fluid. These results suggest that the catalytic effect of sPLA2 is responsible for stimulation of EC migration by human synovial fluid (Figure 8). In contrast, pretreatment of human synovial fluid with BEL, a specific inhibitor of the calcium-independent PLA2(iPLA2),36 had no effect on the migratory response of ECs (data not shown).
Effect of inhibition of human synovial fluid sPLA2 activity on EC migration.
Aliquots of human synovial fluid (15 μL) treated withp-BPB or with vehicle were placed in the lower compartment of a Transwell chamber. BAECs, placed in the upper compartment of the Transwell chamber, were allowed to migrate for 2 hours at 37°C. Determination of the number of migrated cells was carried out as described in “Material and methods.” Bars represent the mean ± SE from triplicate determinations of 3 independent experiments. Asterisk indicates statistical significance (P < .01 versus untreated human synovial fluid); HSF, human synovial fluid.
Effect of inhibition of human synovial fluid sPLA2 activity on EC migration.
Aliquots of human synovial fluid (15 μL) treated withp-BPB or with vehicle were placed in the lower compartment of a Transwell chamber. BAECs, placed in the upper compartment of the Transwell chamber, were allowed to migrate for 2 hours at 37°C. Determination of the number of migrated cells was carried out as described in “Material and methods.” Bars represent the mean ± SE from triplicate determinations of 3 independent experiments. Asterisk indicates statistical significance (P < .01 versus untreated human synovial fluid); HSF, human synovial fluid.
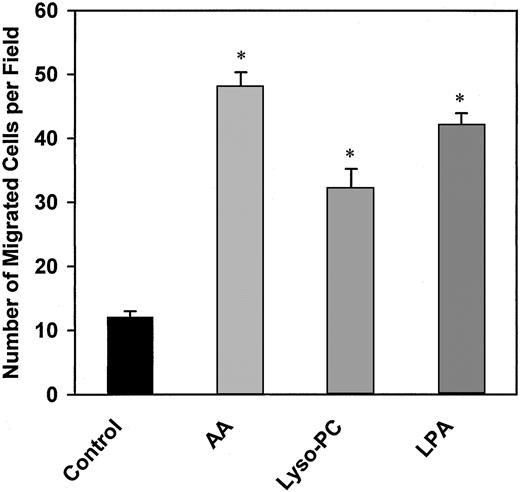
Activation of sPLA2 leads to generation of lipid mediators including AA, LPA, and lysophosphatidylcholine (lyso-PC).1-5 Therefore, we tested the effect of AA, LPA, and lyso-PC on migration of ECs. Stimulation of BAECs with AA (10 μmol/L), LPA (0.5 μmol/L), or lyso-PC (10 μmol/L) for 1 hour at 37°C induced a 4-, 2.7-, and 3.8-fold increase of EC migration over vehicle alone (Figure 9).
Effect of AA, LPA, and lyso-PC on EC migration.
BAECs were placed on the upper compartment of a Boyden chamber. AA (10 μmol/L), LPA (0.5 μmol/L), and lyso-PC (1 μmol/L) were placed in the lower compartment. Migration was carried out for 1 hour at 37°C. The number of migrated cells was determined as described in “Material and methods.” Bars represent the mean ± SE of 3 independent experiments. Asterisk indicates statistical significance (P < .005 versus control).
Effect of AA, LPA, and lyso-PC on EC migration.
BAECs were placed on the upper compartment of a Boyden chamber. AA (10 μmol/L), LPA (0.5 μmol/L), and lyso-PC (1 μmol/L) were placed in the lower compartment. Migration was carried out for 1 hour at 37°C. The number of migrated cells was determined as described in “Material and methods.” Bars represent the mean ± SE of 3 independent experiments. Asterisk indicates statistical significance (P < .005 versus control).
Discussion
Secreted PLA2s comprise several groups of lipolytic enzymes implicated in the regulation of a variety of pathophysiologic conditions.1-4 These enzymes are found in abundance in mammalian tissues and in snake and insect venoms and form a family of structurally related enzymes.1-4 Although previous studies have demonstrated a role for pancreatic and Naja najaPLA2 as positive regulators of cell motility, no direct evidence exists on the effect of these enzymes on EC migration.19-21 To our knowledge, the present study is the first to describe the migration of vascular ECs in response to sPLA2. Previous studies by Sa and Fox21 showed that inhibitors of PLA2 including aristolochic acid and ONO-RS-082 decreased bFGF-stimulated EC migration. However, in this work, no evidence of a direct effect of PLA2 on EC migration was presented nor was the class of which PLA2mediated the effect of bFGF investigated. In this paper, we have demonstrated that ECs of different tissue origins migrated toward sPLA2s, including bee venom, Naja naja, OS1, and porcine and human pancreatic sPLA2. NIH-3T3, but not HVSMCs, migrated to bvPLA2 suggesting that the effect of the enzyme is cell-type specific. The migratory response of ECs to bvPLA2was only observed when a concentration gradient of the enzyme was present, implying a chemotactic rather than a chemokinetic effect. In contrast, a chemokinetic effect of pancreatic sPLA2 has been demonstrated on rat vascular smooth muscle cells.37
The effect of sPLA2 on EC motility, which we observed, was dose and time dependent. Exposure of BAECs to bvPLA2induced a rapid chemotactic response as demonstrated by the initial cell movement across the filter, detected between 15 and 30 minutes of stimulation. The effect of sPLA2 on cell motility increased over a period of 2 hours and declined thereafter. After 4 hours of stimulation, no difference between stimulated and unstimulated cells was detected. The decline of cell migration after 4 hours of exposure to sPLA2 is in contrast with the findings of Sa and Fox,21 who observed a slower EC response (presumably PLA2 dependent) after bFGF stimulation. Thus, these authors demonstrated that bFGF-dependent wound-induced EC movement was mediated by induction of PLA2 activity after 20 hours of incubation.21 However, differences in the techniques used to analyze cell migration may be implicated in the observed differences, because we measured cell migration using a modified Boyden chamber. In the Boyden chamber, the stimulus placed in the lower compartment will gradually diffuse into the upper compartment. Thus, although we did not measure the diffusion coefficient of bvPLA2, it may be possible that at 4 hours of stimulation, bvPLA2 diffusion into the upper compartment is complete, thereby abolishing the concentration gradient. In addition, it is possible that the longer interval of time necessary for bFGF to induce cell migration, in the experiments of Sa and Fox, was due to the time needed to induce synthesis of PLA2, whereas this lag of time was abolished, in our study, by direct exposure of cells to sPLA2.
Secreted PLA2s have distinct biologic functions. Group I sPLA2 has been implicated in regulation of proliferation and smooth muscle cell contraction.8,38 Group II sPLA2 plays a crucial role as a proinflammatory mediator as demonstrated by in vitro experimental data and clinical studies.10-12 Venom sPLA2 possesses potent neurotoxicity, myocardial toxicity, and anticoagulant and proinflammatory properties.39 We observed that all of the sPLA2 tested (groups I, II, and III) elicited EC migration although with different degrees of potency. The maximum effect was detected following stimulation of ECs with hGIB and hGIIA sPLA2s followed by pGIB sPLA2 and OS1. The concentrations of sPLA2 capable of inducing EC migration were similar to those detected in several pathologic conditions. Thus, concentration of sPLA2 in synovial fluid of patients with arthritis or in plasma of patients with acute chest syndrome has been estimated to be 50 to 500 ng/mL.13-15 In addition, circulating levels of sPLA2 are dramatically increased in patients with pancreatitis.40 The physiologic relevance of our findings is confirmed by the observation that human synovial fluid (containing sPLA2 activity) induced a robust migratory response of ECs. This response is partially sPLA2 dependent as shown by a 56% decrease of EC migration on exposure to p-BPB–treated human synovial fluid. Other inflammatory mediators, such as cytokines, have been detected in the synovial fluid of patients with arthritis41,42 and are likely to contribute to the migration of ECs, which we observed. Nevertheless, our findings support the hypothesis that sPLA2 plays an important role in physiologic and pathologic conditions associated with EC migration such as increase of vascular permeability and angiogenesis.43 44 Thus, we detected an increase of vascular permeability, assayed by the passage of albumin bound to Evans blue dye, through endothelial monolayers stimulated with sPLA2 (unpublished observations). Further studies will be required to determine whether sPLA2-induced EC migration is associated with angiogenesis.
Secreted PLA2 acts on membrane phospholipids to release free fatty acids including AA and lysosphospholipids.6-10Previous studies from our laboratory and others have shown that these biologically active lipids play a critical role in regulation of a variety of cellular functions.45-50 However, sPLA2 can also bind to specific receptors and some of the biologic effects of sPLA2, including cell migration, have been proposed to be associated with the binding of the enzyme to its receptors.8,15,16,37,38 In the present study, several lines of evidence suggested that the enzymatic activity of sPLA2 was involved in the EC chemotactic response. First, the catalytic site mutant of pGIB sPLA2, H48Q sPLA2, in which substitution of histidine with glutamine induces a drastic reduction of its lipolytic activity,23also induced a less pronounced stimulation of EC migration, when compared to the wild-type pGIB sPLA2. Second, inhibition of sPLA2 but not iPLA2 catalytic activity in human synovial fluid induced a marked decrease of EC migration compared to untreated synovial fluid. Third, lipid mediators, which are generated on sPLA2 activation (including AA, LPA, and lyso-PC), stimulated EC migration. These results are consistent with previous studies of Tan and colleagues51 in which the edema-inducing activity of sPLA2 was described to be dependent on the enzyme catalytic activity. Moreover, studies by Minami and coworkers19,20 demonstrated that Naja najasPLA2 stimulated intestinal and gastric epithelial cell migration via its enzymatic activity. On the other hand, studies from Kundu and Mukherjee15 demonstrated that pGIB sPLA2 and Naja naja sPLA2 induced migration of NIH-3T3 cells by a mechanism independent of sPLA2-associated catalytic activity and involving activation of the M-type receptor.15 These authors demonstrated that inactivation of pGIB by p-BPB did not affect the ability of the enzyme to stimulate migration in cells expressing the M-receptor. Furthermore, cells lacking the M-type receptor failed to migrate on stimulation with pGIB, suggesting that binding of pGIB to the M-type receptor is a prerequisite for stimulation of cell migration. We observed that exposure of NIH-3T3 and bone marrow stromal cells to H48Q pGIB induced the same degree of migration as wild-type pGIB (data not shown). Thus, whereas the catalytic activity of sPLA2 on membrane phospholipids is required to induce migration of ECs, in other cell types including fibroblasts, the effect of sPLA2 appears independent of its catalytic activity and may require binding to specific receptors. Further investigation is required to determine whether M-type or N-type receptors or distinct unknown binding sites are involved in mediating these effects of sPLA2. Taken together, these findings suggest that the signaling mechanisms by which sPLA2influences cell locomotion are cell-type specific.
In summary, our findings implicate a physiologic role of sPLA2 as a mediator of EC migration. The mechanisms by which sPLA2 influences EC movement appear to depend on its catalytic activity. Additional studies are required to elucidate the signaling steps involved in the motile response of ECs to sPLA2.
Acknowledgments
We thank Dr Jingsong Chu for technical assistance with the experiment in Figure 6B. We are grateful to Dr M. Janssen for the generous gift of the H48Q pGIB sPLA2. We are indebted to Drs Anne Leaver and William Geary for their comments and critical revision of the manuscript.
Supported by grants from the Showalter Foundation, the American Heart Association (INN-97-701 GIA), and Clarian Values Fund (VFR26) to M.T.R. and from the Centre National de la Recherche Scientifique (CNRS) and the Association pour la Recherche sur le Cancer (ARC) to G.L.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Maria Teresa Rizzo, Signal Transduction Laboratory, Methodist Research Institute, Clarian Health, 1701 North Senate Blvd, Rm WG 30, Indianapolis, IN 46201; e-mail:mrizzo@clarian.com.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal