Congenital relapsing fever (Borrelia hermsii).
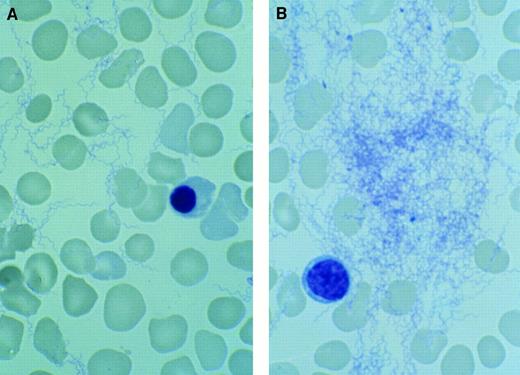
William A. Dittman Sr, Sacred Heart Medical Center, Spokane, WA. A 35-week infant was delivered by cesarean section because of fetal distress. Her mother presented to Sacred Heart Medical Center early because of decreased fetal movement. At delivery, the child demonstrated respiratory depression requiring intubation and manual resuscitation. Apgar scores were 1 at one minute and 5 at five minutes. The “admitting” diagnosis was sepsis with shock. Cord blood counts revealed a white blood cell count at 8.2/μL, hemoglobin level at 16.4g/dL, hematocrit level at 48.8%, and platelet count at 8/μL. Nucleated red blood cells were 88 per 100 white blood cells. During verification of the platelet count with the blood film, multiple spirochetes were seen (A), many in clumps (B). These spirochetes were further classified and confirmed by immunofluorescent antibody staining as Borrelia hermsii. No organisms were seen on multiple blood films of the mother. Although the placenta was grossly and microscopically normal, silver stains demonstrated spirochetes. A review of the prenatal history identified an episode of fever, chills, aching, headache, and fatigue which occurred at week 16 of the pregnancy. The mother recalled a similar one-day illness at week 19. There were no other untoward events until presentation. The child was treated with fluids for the septic shock. Ampicillin and cefotaxime were given initially, and erythromycin was added when the spirochetes were found. Dexamethasone was administered for the septic shock and thrombocytopenia. Improvement was progressive until day 9 when hypotension, pallor, and abdominal distension occurred. Autopsy revealed bleeding into a liver abscess with subsequent rupture of a subcapsular hematoma. No organisms were found in the abscesses at autopsy. Relapsing fever (tick-borne borrelia hermsii) is endemic to the western United States. It is transmitted by theOrnithodoros hermsii tick.
Congenital relapsing fever (Borrelia hermsii).
William A. Dittman Sr, Sacred Heart Medical Center, Spokane, WA. A 35-week infant was delivered by cesarean section because of fetal distress. Her mother presented to Sacred Heart Medical Center early because of decreased fetal movement. At delivery, the child demonstrated respiratory depression requiring intubation and manual resuscitation. Apgar scores were 1 at one minute and 5 at five minutes. The “admitting” diagnosis was sepsis with shock. Cord blood counts revealed a white blood cell count at 8.2/μL, hemoglobin level at 16.4g/dL, hematocrit level at 48.8%, and platelet count at 8/μL. Nucleated red blood cells were 88 per 100 white blood cells. During verification of the platelet count with the blood film, multiple spirochetes were seen (A), many in clumps (B). These spirochetes were further classified and confirmed by immunofluorescent antibody staining as Borrelia hermsii. No organisms were seen on multiple blood films of the mother. Although the placenta was grossly and microscopically normal, silver stains demonstrated spirochetes. A review of the prenatal history identified an episode of fever, chills, aching, headache, and fatigue which occurred at week 16 of the pregnancy. The mother recalled a similar one-day illness at week 19. There were no other untoward events until presentation. The child was treated with fluids for the septic shock. Ampicillin and cefotaxime were given initially, and erythromycin was added when the spirochetes were found. Dexamethasone was administered for the septic shock and thrombocytopenia. Improvement was progressive until day 9 when hypotension, pallor, and abdominal distension occurred. Autopsy revealed bleeding into a liver abscess with subsequent rupture of a subcapsular hematoma. No organisms were found in the abscesses at autopsy. Relapsing fever (tick-borne borrelia hermsii) is endemic to the western United States. It is transmitted by theOrnithodoros hermsii tick.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal