Cell adhesion molecules are critically involved in the multistep process of leukocyte recruitment in inflammation. The specific receptors used by polymorphonuclear leukocytes (PMN) for locomotion in extravascular tissue have as yet not been identified. By means of immunofluorescence flow cytometry and laser scanning confocal microscopy, this study demonstrated that surface expression of the 2β1 (VLA-2) integrin, though absent on blood PMN, is induced in extravasated PMN collected from human skin blister chambers, and rat PMN accumulated in the peritoneal cavity after chemotactic stimulation. Intravital time-lapse videomicroscopy was used to investigate chemoattractant-induced PMN locomotion in the rat mesentery in vivo. Local administration of function-blocking monoclonal antibody or peptide recognizing the 2β1 integrin reduced PMN migration velocity in the extravascular tissue by 73% ± 3% and 70% ± 10%, respectively ( means ± SD). The distance f-met-leu-phe peptide (fMLP)-stimulated human PMN migrated in a collagen gel in vitro was markedly reduced by treatment with anti-2 mAbs or peptide, whereas no effect was observed with antibodies or peptides recognizing the 4β1 or 5β1integrins. Further evidence for a critical role of expression of 2β1 integrin in PMN locomotion in extravascular tissue was obtained in the mouse air pouch model of acute inflammation where chemoattractant-induced PMN recruitment was substantially inhibited by local anti-2 mAb treatment. Thus, expression of 2β1 integrin on extravasated PMN has been identified and a novel role of this receptor in regulating the extravascular phase of leukocyte trafficking in inflammation has been formulated.
Recruitment of polymorphonuclear leukocytes (PMN) constitutes the first line of defense in the cellular inflammation response.1 Following their emigration from the vasculature, the PMN respond to chemotactic gradients by moving in the extravascular tissue toward sites of injury or infection. The locomotion of extravasated PMN is thought to depend on coordinated and transient interactions of leukocytic cell adhesion molecules with extracellular matrix (ECM) components.2 Although it is established that adhesion molecules of the selectin and β2 integrin families are critical for PMN adhesion to the endothelium,3there is no direct evidence that PMN migration in the extravascular tissue is dependent on these molecules. The β1 (VLA) integrins comprise a family of receptors that mediate cell adhesion to ECM proteins (eg, collagen, fibronectin, and laminin). They share a common β chain (β1; CD29) that is non-covalently linked to 1 of at least 6 different α chains (α1-α6; CD49a-f) determining the binding properties of the receptor.4 The function of β1 integrin in PMN has been considered to be limited because circulating blood PMN, in contrast to other hematopoietic cells, express only low levels of β1integrins.4 However, recent observations indicate that extravasation of PMN may be associated with up-regulation of β1 integrins on the cell surface,5-7 and significant expression of α4β1, α5β1, and α6β1on these cells has been reported.5-8 We have previously documented a critical role for β1 integrins in PMN locomotion in vivo.7 Moreover, this process was shown to involve members of the β1 integrin family other than the fibronectin-binding receptors α4β1 and α5β1. Results of this study indicate that surface expression of the α2β1 (VLA-2) integrin is induced in human and rat PMN on extravasation in vivo and that PMN locomotion and recruitment to extravascular tissue are critically dependent on α2β1 integrin function.
Materials and methods
Antibodies and peptides
The following antibodies reacting with rat integrin molecules were used: monoclonal antibody (mAb) HMβ1-1 against the β1 subunit (CD29) and mAb Ha1/29 (cross-reactive with mouse) against the α2 subunit (CD49b) (both from Pharmingen, San Diego, CA), mAb TA-2 (Serotec, Oxford, England) against the α4 subunit (CD49d), and mAb HMα5-1 (Pharmingen) against the α5 subunit (CD49e). The following mAbs reacting with human integrin molecules were used: mAb13 against the β1 subunit (CD29) (Becton Dickinson, Mountain View, CA), mAb P1E6 (Becton Dickinson) and mAb AK7 (Pharmingen) against the α2 subunit (CD49b), mAb L25.3 (Becton Dickinson) against the α4 subunit (CD49d), and mAb16 against the α5 subunit (CD49e) (Becton Dickinson). Function-blocking activity has been documented for all antibodies listed above.
The following integrin-binding peptides were used: DGEA (Peninsula Laboratories, Belmont, CA) specifically blocking α2β1 integrin binding to type I collagen,9 SLIDIP blocking the function of α4β1 integrin and ACRGDGWMCG (RGDGW) blocking the function of α5β1integrin.10
Antibodies Ha1/29, TA-2, HMα5-1, P1E6, AK7, mAb13, L25.3, and mAb16 contained sodium azide (0.001-0.01% in final dilution). Other reagents were free of preservatives. Control experiments showed that sodium azide at corresponding concentrations was without effect on the parameters analyzed as previously reported.7
Isolation of human PMN
The suction-blister chamber technique was used as previously described.11 The experimental procedure was approved by the local ethical committee. In brief, chambers with a volume of 1 mL were mounted on the freshly formed skin blisters on the volar aspect of the arm and filled with autologous serum (70% in Hank's balanced salt solution [HBSS]) to stimulate PMN extravasation. The skin blister fluid was collected after 8 hours and PMN that had accumulated in the fluid (6-10 × 106 cells/chamber) were washed and resuspended in HBSS. Peripheral blood PMN were isolated from whole blood by single-step density centrifugation over Polymorphprep (Nycomed Pharma AS, Oslo, Norway). Following hypotonic lysis of contaminating red blood cells, the PMN were washed and resuspended in HBSS.
Isolation of rat PMN
Extravasation of PMN in the peritoneal cavity of Wistar rats (200-250 g) was induced by intraperitoneal stimulation with platelet-activating factor (PAF; 10−7 mol/L) (Sigma, St. Louis, MO) in 10 mL HBSS. After 2 hours, the animals were killed with methyl-ether and peritoneal leukocytes were harvested by washing the peritoneal cavity with 10 mL ice-cold HBSS. The leukocytes were fixed directly in 4% paraformaldehyde for 5 minutes at room temperature, washed twice in HBSS, and stained for fluorescence-activated cell sorter (FACS) analysis as described. EDTA-anticoagulated blood was collected from the same animal, and leukocyte-rich plasma was obtained through dextran sedimentation. The leukocytes were washed and fixed as above.
Immunofluorescence flow cytometry
The PMN were incubated with primary mAb against integrin molecules (10 μg/mL) for 20 minutes at 4°C. After 3 washes the PMN were incubated with fluorescein isothiocyanate (FITC)-conjugated goat antimouse (detecting P1E6, L25.3, and mAb16), goat antirat (detecting mAb13), or goat antihamster (detecting Ha1/29) F(ab′)2 (Jackson Immunoresearch Lab., West Grove, PA), diluted 1:100, for 20 minutes at 4°C in the dark. The cells were again washed 3 times and analyzed on a FACSort flow cytometer (Becton Dickinson). Gating was based on forward and side scatter parameters and purity of analyzed human PMN was ensured with neutrophil specific marker for CD16 (mAb DJ130c; Dako, Glostrup, Denmark). Lymphocyte and platelet contamination was excluded by negative staining with markers for CD2 (mAb MT910; Dako) and CD41 (mAb 5B12; Dako), respectively. Purity of rat PMN collected from the peritoneal cavity was determined through differential leukocyte count (Wright/Giemsa stain).7 Fluorescence intensity of 1 × 104 PMN was analyzed and compared to nonspecific background fluorescence of irrelevant mouse, rat, or hamster IgG.
Identification of 2β1 integrin expression on human PMN adhering to collagen
Purified native collagen (type I) from rat tail tendons, extracted according to standard procedures, was a generous gift from Dr Björn Öbrink (CMB, Karolinska Institutet). Isolated blood PMN at a concentration of 0.5 × 106 cells/mL were plated on coverslips coated with collagen, 20 μg/mL. PMN adhesion and spreading was induced by stimulation with the chemotactic peptide f-met-leu-phe (fMLP, 10−7 mol/L; Sigma) for 15 minutes at 37°C. Nonadherent cells were rinsed off from the coverslips with ice-cold HBSS and adherent cells were fixed for 5 minutes in 4% paraformaldehyde (Sigma) at room temperature. Immunofluorescent staining of α2β1 on adherent cells was performed on ice by incubation with primary mAb P1E6 (10 μg/mL) for 30 minutes. The samples were rinsed 3 times with ice-cold HBSS and incubated with FITC-conjugated antimouse F(ab′)2 (Jackson Immunoresearch Lab), diluted 1:100, for additional 30 minutes at 4°C in the dark. The samples were rinsed and viewed in a laser scanning confocal microscope (Insight Plus, Meridian Instruments Inc, Okemos, MI) under normal transmitted and laser-emitted fluorescent light. Correction for unspecific antibody binding and background fluorescence was made by comparing specific mAb fluorescence with that of samples treated with irrelevant antibodies at the same concentration and incubation time.
Intravital time lapse videomicroscopy of PMN locomotion in vivo
Locomotion of PMN in rat mesenteric tissue was studied through use of intravital time lapse videomicroscopy according to the protocol previously described in detail.7 In brief, Wistar rats (200-250 g) were anesthetized with equal parts of fluanison/fentanyl (10/0.2 mg/mL; Hypnorm; Janssen-Cilag Ltd., Saunderton, UK) and midazolam (5 mg/mL; Dormicum; Hoffman-La Roche, Basel, Switzerland) diluted 1:1 with sterile water (2 mL/kg intramuscularly). Body temperature was maintained at 37°C by a heating pad connected to a rectal thermistor. After laparotomy, a segment of the ileum was exposed on a heated transparent pedestal to allow microscopic observation of the mesenteric microvasculature (Orthoplan microscope equipped with water immersion lens SW × 25, NA 0.60; Leitz, Wetzlar, Germany). The exposed tissue was continuously superfused with a warmed (37°C) bicarbonate-buffered suffusion solution equilibrated with 5% CO2 in nitrogen. The microscopic image was televised and recorded on time-lapse video (at one seventh of normal speed). Analysis of leukocyte migration in the mesenteric tissue was made off line and the migration path of individual leukocytes was tracked with a digital image analyzer.
Leukocyte extravasation and migration were induced by soaking the exposed mesentery with 5 mL CO2-bubbled bicarbonate buffer (37°C) containing PAF at a concentration of 10−7mol/L. The tissue was then covered with a transparent plastic film to provide continuous chemoattractant stimulation. After 40 minutes of chemotactic stimulation, when numerous leukocytes had extravasated, time lapse recording of leukocyte migration was undertaken, first for 20 minutes to assess basal migration rates in response to PAF stimulation, and then for additional 40 minutes in the presence of PAF together with antibodies or peptides. The antibody concentration in the mixture administered to the tissue was for all antibodies 100 μg/mL. The peptide DGEA was administered at a concentration of 25 mM and SLIDIP/RGDGW at a concentration of 500 μM. Due to dilution of the reagent in fluid covering the tissue these seemingly high doses, ∼10 times the documented effective blocking dose, were chosen to reach a sufficient concentration in proximity of the migrating leukocytes in the tissue. Cells that did not move during the observation time were not included in the analysis. As previously documented, more than 85% of the migrating cells were neutrophils.7
PMN migration in gels of collagen (type I) and gelatin
Gels were formed in 24-well culture dishes (250 μL/well) by mixing 8.5 volumes of rat collagen solution or bovine gelatin solution (Sigma) at a concentration of 1.5 mg/mL with 1 volume of × 10 minimum essential medium (MEM; Life Technologies, Gaithersburg, MD) and 0.5 volume of 4.4% NaHCO3 and fMLP (final concentration 10−7 mol/L). Purified human PMN (0.5 × 106), suspended in 200 μL of MEM containing 10−9 mol/L fMLP, were placed on top of the gels and incubated with or without mAbs or peptides for 30 minutes at 37°C. The final concentration was for all mAbs 20 μg/mL, for DGEA 5 mM, and for SLIDIP/RGDGW 100 μM. The tetrapeptide RGDV was used as control for DGEA at a concentration of 5 mM. Four to 6 experiments were run in duplicate gels for each reagent tested and 10 randomly chosen microscopic fields (with a defined area of 0.0625 mm2) were analyzed in each gel. The migration of PMN into the gel was analyzed with an Leitz Orthoplan microscope equipped with a water immersion lens (Leitz UO × 55W, NA 0.80) by focusing down through the gel. The calibrated micrometer scale in the fine focus adjustment was used to determine the migration distance of individual PMN from the upper gel surface. The average migration distance of the 3 leading cells in each field was calculated and defined as the migration distance of the leading front.
PMN accumulation in the mouse air pouch
Male C57BL/6 mice weighing 25 to 30 g were anesthetized through inhalation of Isofluran (Abbott Laboratories, North Chicago, IL), and 5 mL of sterile air was injected subcutaneously into the back. After 3 days, the air pouch was reinflated with 2.5 mL sterile air. Six days after the initial air injection, 0.5 mL HBSS containing PAF (10−7 mol/L) together with mAb Ha1/29 or isotype-matched control mAb (irrelevant hamster IgG) at a final concentration of 50 μg/mL was injected into the air pouch. HBSS without PAF was used to assess PMN accumulation in the pouch in absence of a chemotactic stimulus. Four hours later, the animals were killed through inhalation of Isofluran and the air pouches lavaged with 1 mL HBSS. Leukocytes in exudates were stained and counted in a Bürker chamber.
All animal experiments presented in this study were approved by the regional ethical committee for animal experimentation.
Statistical evaluation
Data are presented as means ± SD. Statistical significance was calculated using the Wilcoxon signed rank test for paired observations and the Mann-Whitney test for independent samples.
Results
Surface expression of 2, 4, and 5 integrin subunits is induced in extravasated PMN
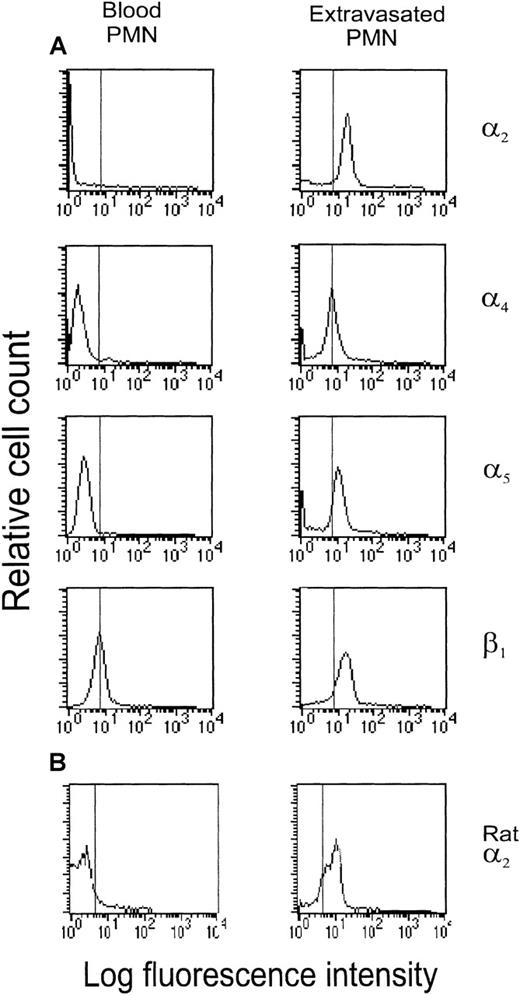
Surface expression of β1 integrin receptors was analyzed on blood PMN and on extravasated human PMN obtained with the skin blister chamber technique. Immunofluorescence flow cytometry showed that expression of the β1 integrin subunit on blood PMN is limited and apparently associated with the α6 subunit (data not shown). A significant increase in β1 integrin expression was detected on extravasated PMN. Expression of the α2, α4, and α5 subunits was concomitantly induced in the extravasated PMN (Figure 1A), whereas the expression of α1 and α3 remained negative (data not shown). Incubation of isolated human blood PMN in suspension at 37°C with the chemoattractant fMLP (10−9-10−5 mol/L) or PAF (10−7-10−5 mol/L) for up to 2.5 hours failed to increase β1 integrin expression (data not shown). In agreement with the induction of α2β1 integrin expression on extravasated human PMN, α2β1 was also detected on rat PMN that accumulated in the peritoneal cavity in response to chemotactic stimulation with PAF (Figure 1B).
FACS analysis of integrin molecule expression on human (A) and rat (B) PMN.
Left panel shows staining of PMN isolated from peripheral whole blood. Right panel shows staining of extravasated human PMN accumulated in skin blister chambers in response to stimulation with autologous serum and rat PMN accumulated in the peritoneal cavity in response to PAF stimulation (10−7 mol/L). Vertical line indicates the 99th percentile of fluorescence events for cells stained with irrelevant, species-matched IgG. Histograms are representative tracings of 4 to 6 analyses for each antibody.
FACS analysis of integrin molecule expression on human (A) and rat (B) PMN.
Left panel shows staining of PMN isolated from peripheral whole blood. Right panel shows staining of extravasated human PMN accumulated in skin blister chambers in response to stimulation with autologous serum and rat PMN accumulated in the peritoneal cavity in response to PAF stimulation (10−7 mol/L). Vertical line indicates the 99th percentile of fluorescence events for cells stained with irrelevant, species-matched IgG. Histograms are representative tracings of 4 to 6 analyses for each antibody.
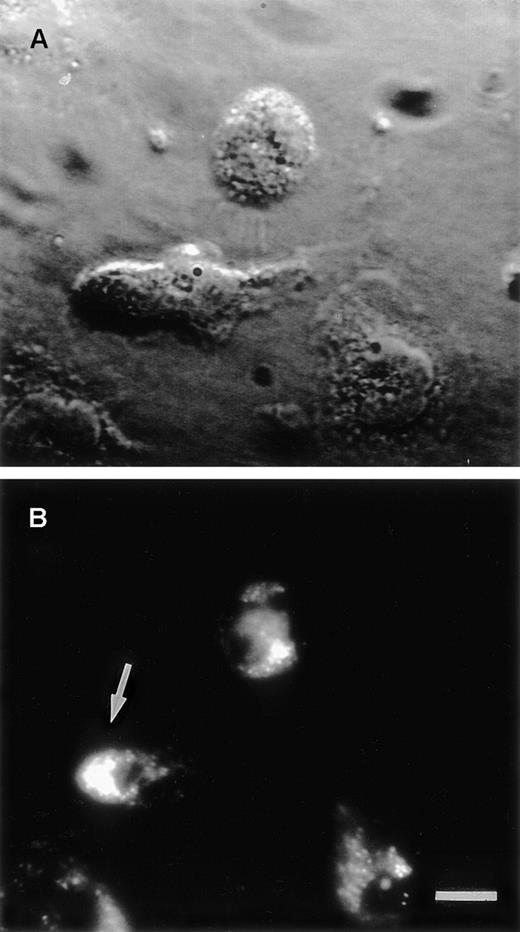
Laser-scanning confocal microscopy was used to confirm α2β1 integrin expression on human blood PMN migrating on collagen in response to stimulation with fMLP (Figure2). In most cells with a polarized morphology, intense staining for α2β1 was localized to the anterior lamellipodium of the cell (Figure 2B). For adherent PMN with a less polarized morphology, staining for α2β1 was fainter and distributed diffusely over the cell membrane.
Stimulated human PMN.
(A) Enhanced transmitted light image of fMLP (10−7mol/L)-stimulated human PMN adhering to collagen. (B) Corresponding image in laser-emitted fluorescent light showing immunofluorescent staining for α2β1. Combined examination of cell morphology and α2β1 integrin expression revealed that the receptor was localized to the lamellipodium in the front of PMN having a distinct head-tail morphology (arrow). Bar indicates 5 μm.
Stimulated human PMN.
(A) Enhanced transmitted light image of fMLP (10−7mol/L)-stimulated human PMN adhering to collagen. (B) Corresponding image in laser-emitted fluorescent light showing immunofluorescent staining for α2β1. Combined examination of cell morphology and α2β1 integrin expression revealed that the receptor was localized to the lamellipodium in the front of PMN having a distinct head-tail morphology (arrow). Bar indicates 5 μm.
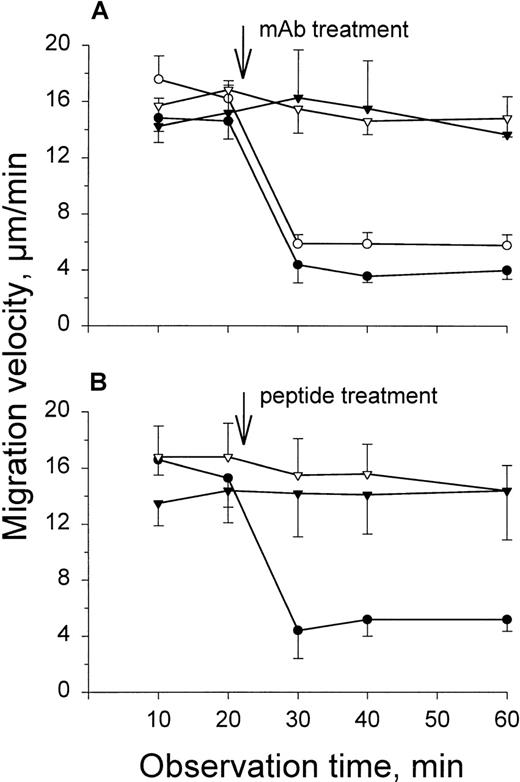
Blockade of 2β1 function inhibits PMN locomotion in rat mesenteric tissue in vivo and in collagen gels in vitro
Direct intravital time-lapse videomicroscopy was used to investigate PMN locomotion in the rat mesentery in vivo. The migration velocity of randomly chosen PMN that had extravasated to the interstitial tissue in response to PAF stimulation was determined before and after topical administration of function blocking antibodies or peptides against β1 integrins (Figure 3). Treatment with mAb Ha1/29 against the rat α2 integrin subunit rapidly and persistently reduced PMN migration velocity from 14.7 ± 1.4 μm/min in response to PAF alone to 3.9 ± 0.9 μm/min after administration of the antibody (73% ± 3% inhibition, P < 0.001) (Figure 3A). Similar inhibition of PMN locomotion has previously been reported by us after antibody blockade of the common β1 integrin chain.7 As shown in Figure 3A, combined administration of antibodies against the α2 and the β1 integrin chain did not further inhibit PMN locomotion above what was found for either of the treatments alone (16.9 ± 1.4 μm/min to 5.9 ± 0.7 μm/min, 65 ± 6% inhibition, P < 0.001). Treatment with antibodies against the α4 or α5 subunits was without effect on migration velocity. Also, administration of isotype-matched control antibodies at the same concentration, and with the same incubation time, did not modulate PMN migration (data not shown).
Time course effects of local treatment with antibodies (A) or peptides (B) on PAF-stimulated (10−7 mol/L) PMN locomotion in the rat mesentery.
(A) Anti-α2 (mAb Ha1/29) (•), combined anti-α2 and anti-β1 (mAb HMβ1-1) (○), anti-α4 (mAb TA-2) (▾), and anti-α5 (mAb HMα5-1) (▿) integrin antibodies (100 μg/mL). (B) The α2β1-binding peptide DGEA (25 mM) (•), α4β1-binding peptide SLIDIP (500 μM) (▾), and α5β1-binding peptide RGDGW (500 μM) (▿). Data are based on calculation of mean migration velocity during 10- to 20-minute periods and presented as means ± SD of 4 to 5 experiments for each reagent tested.
Time course effects of local treatment with antibodies (A) or peptides (B) on PAF-stimulated (10−7 mol/L) PMN locomotion in the rat mesentery.
(A) Anti-α2 (mAb Ha1/29) (•), combined anti-α2 and anti-β1 (mAb HMβ1-1) (○), anti-α4 (mAb TA-2) (▾), and anti-α5 (mAb HMα5-1) (▿) integrin antibodies (100 μg/mL). (B) The α2β1-binding peptide DGEA (25 mM) (•), α4β1-binding peptide SLIDIP (500 μM) (▾), and α5β1-binding peptide RGDGW (500 μM) (▿). Data are based on calculation of mean migration velocity during 10- to 20-minute periods and presented as means ± SD of 4 to 5 experiments for each reagent tested.
The β1 integrin-binding peptides had similar activity profile on PMN migration velocity as antibodies (Figure 3B). The tetrapeptide DGEA, specifically blocking α2β1 integrin-mediated adhesion to collagen,9 inhibited PMN migration velocity by 70 ± 10% (P < 0.001), whereas peptides against α4β1 integrin (SLIDIP) and α5β1 integrin (RGDGW) were without effect on PMN migration. The use of 10-fold higher concentrations of SLIDIP/RGDGW in some experiments did not yield different effects.
We further analyzed the involvement of β1integrins in human PMN chemotaxis in collagen (type I) gels (Figure4A). PMN, suspended in fMLP 10−9 mol/L, were placed on top of collagen gels containing fMLP at a concentration of 10−7 mol/L. The PMN migrated down into the gel along the chemotactic gradient that was established. Migration distance of the leading front of fMLP-stimulated PMN was 76.5 ± 5.3 μm over a 30-minute incubation period at 37°C. Blockade of α2β1 integrin function with either mAb P1E6 or AK7 reduced the migration distance of fMLP-stimulated PMN to the level of nonstimulated cells. The α2β1 integrin-binding peptide DGEA, but not the tetrapeptide RGDV used as control for DGEA, reduced migration distance to the same extent. Antibody blockade of the common β1 chain either alone or in combination with anti-α2 antibody (mAb13 + P1E6) was less effective in inhibiting PMN locomotion than blockade of α2 alone. Blockade with either antibodies or peptides of α4β1 and α5β1, alone or in combination, resulted in a slightly increased migration distance in the collagen gels. Qualitatively similar results as those reported here for fMLP-stimulated PMN were obtained with PAF as chemoattractant (data not shown); however, migration was not as efficient.
fMLP-stimulated PMN chemotaxis in gels of collagen (A) and gelatin (B).
PMN, suspended in fMLP 10−9 mol/L, were placed on top of the gels containing fMLP at a concentration of 10−7mol/L. PMN migration into the gel was microscopically quantified after 30 minutes of incubation at 37° C. (A) Effect of antibodies against α2 (mAb P1E6 and mAb AK7), α4 (mAb L25.3), α5 (mAb16), and β1 (mAb13) integrin molecules (20 μg/mL), and of integrin-binding peptides recognizing α2β1 (DGEA, 5 mM), α4β1 (SLIDIP, 100 μM), and α5β1 (RGDGW, 100 μM). The tetrapeptide RGDV (5mM) served as control for DGEA. (B) Effect of antibodies against α2 (mAb AK7) and β1 (mAb13) integrin molecules (20 μg/mL) on fMLP-stimulated PMN migration in gelatin gels. “Unstim” shows PMN migration in respective gel in absence of chemotactic stimulation. Data are based on calculation of migration distance of the leading front and presented as means ± SD of 4 to 6 experiments for each combination analyzed. * indicates significant difference versus fMLP-stimulation alone (P < 0.05).
fMLP-stimulated PMN chemotaxis in gels of collagen (A) and gelatin (B).
PMN, suspended in fMLP 10−9 mol/L, were placed on top of the gels containing fMLP at a concentration of 10−7mol/L. PMN migration into the gel was microscopically quantified after 30 minutes of incubation at 37° C. (A) Effect of antibodies against α2 (mAb P1E6 and mAb AK7), α4 (mAb L25.3), α5 (mAb16), and β1 (mAb13) integrin molecules (20 μg/mL), and of integrin-binding peptides recognizing α2β1 (DGEA, 5 mM), α4β1 (SLIDIP, 100 μM), and α5β1 (RGDGW, 100 μM). The tetrapeptide RGDV (5mM) served as control for DGEA. (B) Effect of antibodies against α2 (mAb AK7) and β1 (mAb13) integrin molecules (20 μg/mL) on fMLP-stimulated PMN migration in gelatin gels. “Unstim” shows PMN migration in respective gel in absence of chemotactic stimulation. Data are based on calculation of migration distance of the leading front and presented as means ± SD of 4 to 6 experiments for each combination analyzed. * indicates significant difference versus fMLP-stimulation alone (P < 0.05).
In a separate set of experiments, PMN migration in gelatin gels was assessed (Figure 4B). This was important to verify that the modulatory effect of β1 integrin blockade was substrate dependent. In comparison with collagen gels, fMLP-stimulated migration in gelatin was less efficient (37.6 ± 3.9 μm). Notably, neither blockage of the α2 subunit or the common β1 chain significantly modulated the migration distance of the leading front.
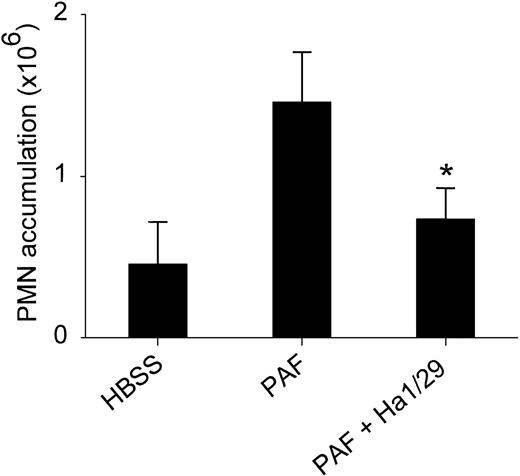
Blocking 2β1 integrin function reduces PAF-stimulated PMN accumulation in mouse air pouch
The involvement of α2β1 in regulating chemoattractant-induced PMN accumulation in extravascular tissue was further investigated using the mouse air pouch model of acute inflammation. As shown in Figure 5, significant leukocyte accumulation (> 90% PMN as identified by nuclear staining) was induced by incubating the air pouch with PAF (together with control antibody) for 4 hours. When PAF was added together with the anti-α2 mAb Ha1/29, the PMN accumulation was substantially reduced (P < 0.01). Compensating for the spontaneous PMN accumulation in the pouch (HBSS only), an inhibition of chemoattractant-induced PMN accumulation by approximately 70% is indicated after anti-α2 mAb treatment.
Effect of anti-2 mAb (Ha1/29) on PMN recruitment in mouse subcutaneous air pouch.
PMN accumulation was assessed by counting leukocytes in the lavage fluid after 4 hours of stimulation with HBSS, PAF (10−7 mol/L together with isotype-matched control antibody), or PAF together with mAb Ha1/29 (50 μg/mL). Values are means ± SD of 7 separate experiments in each group. * indicates significant difference versus PAF (P < 0.01).
Effect of anti-2 mAb (Ha1/29) on PMN recruitment in mouse subcutaneous air pouch.
PMN accumulation was assessed by counting leukocytes in the lavage fluid after 4 hours of stimulation with HBSS, PAF (10−7 mol/L together with isotype-matched control antibody), or PAF together with mAb Ha1/29 (50 μg/mL). Values are means ± SD of 7 separate experiments in each group. * indicates significant difference versus PAF (P < 0.01).
Discussion
One hallmark of acute inflammation is the early and rapid recruitment of PMN to sites of infection and tissue injury. The initial events in the process of PMN extravasation have been carefully investigated, revealing a complex receptor cross-talk between leukocytes and endothelium.1 Less is known, however, about adhesive interactions involved in the subsequent PMN locomotion in extravascular tissue. We recently showed that adhesion molecules belonging to the β1 integrin family participate in this process.7 The present study provides evidence for a critical role of the collagen-binding α2β1integrin in the recruitment of PMN to inflamed tissue sites. First, in vivo extravasation of human and rodent PMN was associated with induction of α2β1 integrin on the PMN surface. Second, blockade of α2β1 integrin function with either mAb or peptide markedly impaired PMN locomotion both in vivo and in vitro. Third, PMN recruitment to tissues in response to chemotactic stimulation was greatly reduced after local anti-α2 treatment. Surface expression of α2β1 was detected on both human PMN that had extravasated in the skin of the forearm and rat PMN after extravasation in the peritoneal cavity. Because expression of α2β1 on blood PMN is negative, these findings indicate that α2β1 is induced in PMN in conjunction with their emigration from blood to tissue. A similar induction of α4β1 expression on PMN extravasation has previously been reported.6,7 However, this study is the first to demonstrate that α2β1 can be found on PMN and serves a specific function in these cells. Similar to the αvβ3 integrin, which is thought to support PMN locomotion on vitronectin,12α2β1 was localized predominantly to the anterior lamellipodium of PMN migrating on collagen. The precise mechanisms underlying the induction of different β1integrins on the PMN surface in association with their extravasation are still unknown and need further investigation. Previous data have suggested that transmigration of the PMN and cytoskeletal reorganization are required for up-regulation of β1integrins.5 Our observation that chemotactic stimulation of isolated blood PMN in suspension failed to induce α2β1 integrin expression, whereas expression was induced in stimulated PMN adhering to collagen further suggests that adhesion-dependent signaling events are significant for induction of β1 integrin expression. The apparent complexity of regulation of α2β1 expression in PMN may explain why this cell population formerly has been considered to lack the α2β1receptor.4
Chemoattractants are known to induce a kinetic response of leukocytes (chemokinesis) that in the presence of a concentration gradient is manifested as a directional movement (chemotaxis). In this study, blockage of α2β1 integrin function inhibited both directional (collagen gel and mouse air pouch) and nondirectional (rat mesentery) PMN locomotion, which conforms to the notion that the biochemical mechanisms by which chemoattractants stimulate chemotaxis and chemokinesis probably are the same.13 Further, our findings that inhibition of α2β1 integrin function suppressed PMN locomotion in both the rat mesentery in vivo and collagen gels in vitro indicate that the antibody/peptide effect on PMN migration in vivo was not due to potential involvement in this process of other β1 integrin-expressing cells present in the tissue (eg, fibroblasts and mast cells). The finding that blockade of the α2β1 integrin with antibody or peptide caused substantial inhibition of PMN locomotion, and that combined inhibition of α2 and the common β1 chain did not result in further inhibition, indicate that β1integrin-mediated PMN locomotion in extravascular connective tissue is primarily dependent on the α2β1 integrin and clearly suggest a principal role of this receptor in leukocyte motility. Substrate specificity in the motile response is indicated by the differences observed for migration in collagen versus gelatin gels. Accordingly, as previously shown by us, neither antibodies nor integrin-binding peptides, blocking the function of the fibronectin-binding receptors α4β1 and α5β1, are effective in modulating PMN locomotion in the rat mesentery in vivo.7 Interestingly, here we report a tendency for slightly increased PMN migration distance in collagen gels after blockade of α4 and α5 integrins. Fibronectin can be secreted by activated PMN,14 which may explain a function of the fibronectin-binding receptors in gels of pure collagen. In accordance, PMN locomotion in collagen gels has been shown to be reduced on supplementation of the gel with fibronectin.15 These data may suggest an anchoring function of the α4 and α5 integrins in the leukocyte extravascular migration and indicate a complex interplay between different integrin receptors in regulating the motility of these cells. The distribution of integrin receptors on the cell surface (eg, receptor clustering and polarization) and their recycling properties, critical for receptor function and ECM interactions, have been shown to be differentially regulated for different integrins,16 which may explain distinct roles of various β1 integrins in the locomotive process. Moreover, the receptor ligand avidity may be regulated distinct from the receptor expression,17 and rate of changes in avidity may accordingly determine the role of different integrins in the consecutive steps of the leukocyte extravasation process.18
Others have observed increased β1 integrin expression in T cells after transendothelial migration19 and that lymphocyte locomotion in collagen gels is attenuated by α2β1 blockade.20 These results are consistent with our findings and indicate that induction and engagement of α2β1 may be a general mechanism by which the different leukocyte subclasses reach their targets in extravascular tissue. On the other hand, integrin-independent PMN locomotion has been demonstrated in experimental systems devoid of extracellular matrix proteins.21 These observations indicate that integrin receptors, apparently required for PMN locomotion in the dense restraining meshwork of biopolymers in native tissue, may be of little importance for locomotion in an environment lacking such elements. Noteworthy, collagen, by far, is the most abundant protein in the extracellular matrix and makes up one third of total body protein, which speaks in favor of collagen as a primary substrate in leukocyte interactions with extracellular matrix.
Using the mouse air pouch model of acute inflammation, PMN recruitment to tissues in response to chemotactic stimulation is markedly suppressed after local treatment with monoclonal antibodies against the α2β1 integrin. Because mAb treatment was extravascular, and uptake of intact mAb into the circulation is limited due to the size of the Ig molecule, the inhibitory effect on PMN accumulation in the pouch most likely can be ascribed to an extravascular activity of the mAb in agreement with our microscopic observations rather than being related to an effect on intravascular events. Together with the microscopic findings of impaired PMN locomotion after α2β1 blockade, these observations indicate a direct relationship between the locomotive capacity of PMN in the extravascular space and their ability to accumulate in inflamed tissue. Thus, the α2β1 integrin complements the intravascular functions of the selectins and β2 integrins in the recruitment of PMN to sites of injury or infection by serving a distinct and critical function in the extravascular phase of this process. These findings provide new insight into the roles of various cell adhesion molecules in leukocyte trafficking, and they also suggest that the α2β1 integrin is a potential target molecule in the development of new therapeutic strategies in treatment of inflammatory disease.
Supported by the Swedish Medical Research Council (14X-4342, 04P-10738), the Swedish Foundation for Health Care Sciences and Allergy Research (A98110), and IngaBritt and Arne Lundbergs Foundation.
Reprints:Lennart Lindbom, Department of Physiology and Pharmacology, Karolinska Institutet, S-171 77 Stockholm, Sweden; e-mail: lennart.lindbom@fyfa.ki.se.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal