Abstract
Transfusion or transplantation of T lymphocytes into an allogeneic recipient can evoke potent immune responses including, in immunocompromised patients, graft-versus-host disease (GVHD). As our previous studies demonstrated attenuated immunorecognition of red blood cells covalently modified with methoxy(polyethylene glycol) (mPEG), we hypothesized that T-cell activation by foreign antigens might similarly be prevented by mPEG modification. Mixed lymphocyte reactions (MLR) using peripheral blood mononuclear cells (PBMC) from HLA class II disparate donors demonstrate that mPEG modification of PBMC effectively inhibits T-cell proliferation (measured by 3H-thymidine incorporation) in a dose-dependent manner. Even slight derivatization (0.4 mmol/L mPEG per 4 × 106 cells) resulted in a ≥75% decrease, while higher concentrations caused ≥96% decrease in proliferation. Loss of PBMC proliferation was not due to either mPEG-induced cytotoxicity, as viability was normal, or cellular anergy, as phytohemagglutinin (PHA)-stimulated mPEG-PBMC demonstrated normal proliferative responses. Addition of exogenous interleukin (IL)-2 also had no proliferative effect, suggesting that the mPEG-modified T cells were not antigen primed. Flow cytometric analysis demonstrates that mPEG-modification dramatically decreases antibody recognition of multiple molecules involved in essential cell:cell interactions, including both T-cell molecules (CD2, CD3, CD4, CD8, CD28, CD11a, CD62L) and antigen-presenting cell (APC) molecules (CD80, CD58, CD62L) likely preventing the initial adhesion and costimulatory events necessary for immune recognition and response.
THE T LYMPHOCYTE plays a central role in the immune response and under normal circumstances, T-cell activation is closely regulated.1,2 However, with the advent and expansion of transfusion and transplantation medicine, the unwanted activation of donor T cells in blood products has become an issue of grave clinical concern, especially with regards to graft-versus-host disease (GVHD).3-5 Consequently, extensive attention has been given to the removal or inactivation of contaminating (passenger) T cells, as well as other leukocytes (B lymphocytes, mononuclear cells, and granulocytes) from blood products.
Currently blood banks inactivate/remove passenger leukocytes via gamma irradiation (inactivation) and/or filtration (removal). While both are clinically proven leuko-reduction methods, neither is without problems.6-8 Irradiation has been shown to result in a decreased storage life of red blood cells (RBC) and may not completely eliminate the risk of allosensitization as leukocyte membrane fragments remain after irradiation. Filtration methods meanwhile are not 100% effective and significantly increase the costs of blood processing due to the high costs of the filter. Hence even following these methods, a risk of allosensitization to disparate antigens and/or GVHD remains for the transfused patient.
Previously, we demonstrated that the modification of RBC membranes with nonimmunogenic materials (eg, methoxy[polyethylene glycol]; mPEG) could yield antigenically silent (stealth) cells.9-12 These stealth cells exhibit decreased/absent antisera-mediated agglutination, antibody binding, and decreased immunogenicity. Importantly, this modification procedure has no negative effects on normal cell structure, function, or viability. Based on these data, we hypothesized that it would be possible to alter both immune recognition of foreign tissues (eg, major histocompatability complex [MHC] class I and II) and prevent the necessary cell:cell interaction of the T cell and antigen-presenting cell (APC) by the covalent modification of cell surfaces with mPEG. To investigate this hypothesis, we have used mixed lymphocyte reaction (MLR) assays using HLA class II disparate donors.13 14
MATERIALS AND METHODS
Cell derivatization.
Peripheral blood mononuclear cells (PBMC) were prepared from healthy donors by layering whole blood over a Histopaque gradient (Sigma Chemical Co, St Louis, MO) and centrifuging (900g) for 30 minutes. The PBMC were washed 3 times with HEPES/RPMI media containing 1% human albumin. Cell derivatization was performed using cyanuric chloride activated mPEG, ≈ 5 kD (Sigma Chemical Co, St Louis, MO) with concentrations ranging from 0.2 to 4 mmol/l mPEG per 4 × 106 cells. Washed PBMC were incubated with activated mPEG for 60 minutes at room temperature in isotonic alkaline phosphate buffer (PBS; 50 mmol/L K2HPO4 and 105 mmol/L NaCl; pH 8.0).12 The derivatized cells were washed once in RPMI 1650 media containing 1x HEPES and 1% albumin. Depending on the study being performed, the modified cells were either washed once in AimV media if prepared for MLR or 2 times in PBS containing 1.5 mmol/L sodium azide for antibody binding studies.
MLR.
MLR were conducted using PBMC obtained from HLA class II disparate donors (Table 1).13,14 Donor MHC typing (Class I A/B and class II DR) was determined by the Albany Medical Center Transplantation Laboratory. Stimulator cells were rendered unresponsive to proliferation by gamma-irradiation (2 Gy).15 Time course experiments were performed and demonstrated that statistically significant responses were obtained after 4 days of total incubation time using populations of human PBMC. Unless stated otherwise, stimulator and responder PBMC (2.5 × 105 cells per well) were suspended in AimV media and cocultured, in triplicate, in 96-well plates at 37°C, 5% CO2, for 3 days. At day 3, all wells were pulsed with3H-thymidine and incubated 24 hours at 37°C, 5% CO2. Cellular DNA was collected onto filters using a cell culture harvester (Skatron; Suffolk, UK) and 3H-thymidine incorporation was determined by scintillation counting. For some studies exogenous human recombinant interleukin-2 (IL-2; Intergen; Purchase, NY) was added to each well of the MLR on day 1 at a concentration of 0.83 U/mL. The viability of the modified cells both before and after MLR culture was determined by a propidium iodide exclusion assay on the flow cytometer.
MHC Class I and Class II Phenotypes of PBMC Donors
| Name . | Gender . | Class I (A) . | Class I (B) . | Class II (DR) . | Class II (DQ) . |
|---|---|---|---|---|---|
| Donor 1 | Male | 32,- | 60,62 | 4,- | 3,8 |
| Donor 2 | Male | 1,2 | 35,- | 11,12 | 1,7 |
| Donor 3 | Female | 2,3 | 7,35 | 4,14 | 1,3 |
| Donor 4 | Female | 1,29 | 44,57 | 7,- | 2,9 |
| Donor 5 | Female | 2,24 | 60,- | 4,9 | 4,8 |
| Name . | Gender . | Class I (A) . | Class I (B) . | Class II (DR) . | Class II (DQ) . |
|---|---|---|---|---|---|
| Donor 1 | Male | 32,- | 60,62 | 4,- | 3,8 |
| Donor 2 | Male | 1,2 | 35,- | 11,12 | 1,7 |
| Donor 3 | Female | 2,3 | 7,35 | 4,14 | 1,3 |
| Donor 4 | Female | 1,29 | 44,57 | 7,- | 2,9 |
| Donor 5 | Female | 2,24 | 60,- | 4,9 | 4,8 |
(-) denotes homozygosity or the presence of a null allele.
Mitogen and antigen presentation studies.
Control and mPEG-derivatized cells were incubated, in triplicate, with phytohemagglutinin (PHA) (Sigma; 1 μg per 107 cells) or tetanus toxoid antigen16 (Sigma; 33.3 μg/mL) in 96-well plates at 37°C, 5% CO2 for 3 days. As in the MLR studies, all wells were pulsed the 3H-thymidine at day 3 and incubated an additional 24 hours (37°C, 5% CO2) before filter harvesting and determination of 3H-thymidine incorporation.
PBMC surface marker analysis.
To quantitate the ability of mPEG-derivatization to camouflage T-cell and APC adhesion and surface molecules, control and derivatized PBMC were examined by flow cytometry (FACScan, Becton Dickinson & Co, Mountain View, CA).17 18 For these studies, control and derivatized PBMC were resuspended into sample tubes at a concentration of 1.0 × 106 PBMC to which 20 μL of fluorescently-labeled mouse antihuman CD antibody (Becton Dickinson & Co) was added. The PBMC were incubated on ice for 30 minutes, washed 2 times in PBS containing azide and immediately analyzed for the fluorescence intensity of T-cell (CD2, CD3, CD4, CD8, CD28, CD11a, and CD62L) and APC (CD14, CD80, CD58, CD62L, and HLA class II) molecules. A minimum of 10,000 PBMC per sample were quantitated for the amount of bound fluorescein isothiocyanate (FITC), phycoerythrin (PE), and/or PerCp fluorescently-conjugated antibodies. All samples were analyzed using lymphocyte parameters previously established for FACScan analysis.
Cytokine assays.
To determine if mPEG-modification altered cytokine profiles of the PBMC, stimulator and responder PBMC were suspended in AimV media and cocultured in 96-well plates at 37°C, 5% CO2, for 4 days. On day 4, the supernatant was removed from each well and like wells were pooled together. IL-2, IL-4, IL-10, tumor necrosis factor (TNF)α and interferon (IFN)γ sandwich enzyme-linked immunosorbent assay (ELISA) assays (Immunotech; Marseilles, France) were performed according to the manufacturer’s specifications.
RESULTS
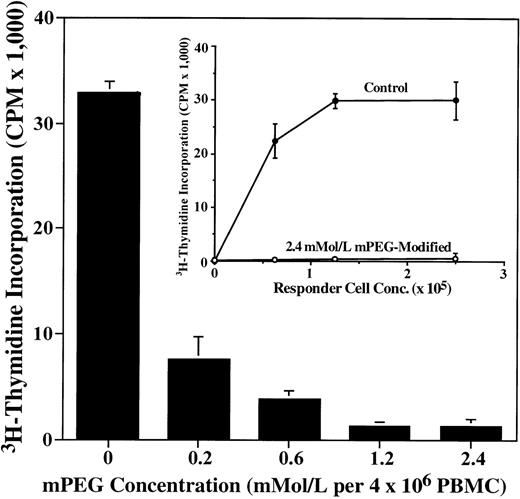
In a 1-way MLR, responder TH cells recognize disparate allogeneic class II MHC molecules on the stimulator cells (irradiated to prevent cell division) and proliferate. The CD4+TH responder cells are the initial proliferative cells and later stimulate proliferation of CD8+ cells.19As shown in Fig 1, the covalent modification of either the responder or stimulator (insert) PBMC with mPEG results in virtually complete inhibition of recognition of the antigenically foreign lymphocytes as denoted by the absence of3H-thymidine incorporation in the responder cells. The observed decrease in T-cell proliferation is dependent on the degree of mPEG-derivatization of the responder cells. However, even slight derivatization of the responder population (0.2 mmol/L mPEG/4 × 106 cells) results in a ≥75% decrease in3H-thymidine incorporation. Higher degrees of modification (0.6 to 2.4 mmol/L mPEG/4 × 106 cells) give rise to a ≥96% decrease in proliferation mimicking the background proliferation rates seen in cells exposed to no antigenic stimulus. Furthermore, the loss of proliferation arising from the pegylation of stimulator PBMC cannot be overcome by the addition of increasing numbers of control responder cells relative to the same stimulator cell population (Fig 1insert). Hence, covalent modification of either the stimulator or responder PBMC population effectively abrogates class II-mediated proliferation.
Cellular proliferation in MLR is effectively attenuated by mPEG-modification of either the responder (main graph) or stimulator (insert) PBMC population. As shown, pegylation of responder cells leads to a mPEG dose-dependent loss of cellular proliferation in response to a disparate MHC class II stimulator PBMC population. Insert: Increasing responder cell numbers does not overcome the antiproliferative effects of mPEG-modification. Shown is increasing numbers of unmodified responder cells exposed to 2.5 × 105 pegylated (2.4 mmol/L per 4 × 106 PBMC) stimulator PBMC. Cell proliferation was determined by 3H-thymidine incorporation into the DNA of the responder cells after 4 days exposure to stimulator cells (irradiated to prevent cell replication). Longer incubations (7 days) were also performed on human PBMC MLR yielding similar results, but higher control counts per minute (CPM). The results shown are the mean ± standard deviation (SD) of triplicate samples from a representative experiment from over 20 individual studies. The main graph uses donors 2 and 3 (responder), while the insert uses donors 2 and 4 (responder). All values for the mPEG-derivatized cells different from control PBMC at P < .0001.
Cellular proliferation in MLR is effectively attenuated by mPEG-modification of either the responder (main graph) or stimulator (insert) PBMC population. As shown, pegylation of responder cells leads to a mPEG dose-dependent loss of cellular proliferation in response to a disparate MHC class II stimulator PBMC population. Insert: Increasing responder cell numbers does not overcome the antiproliferative effects of mPEG-modification. Shown is increasing numbers of unmodified responder cells exposed to 2.5 × 105 pegylated (2.4 mmol/L per 4 × 106 PBMC) stimulator PBMC. Cell proliferation was determined by 3H-thymidine incorporation into the DNA of the responder cells after 4 days exposure to stimulator cells (irradiated to prevent cell replication). Longer incubations (7 days) were also performed on human PBMC MLR yielding similar results, but higher control counts per minute (CPM). The results shown are the mean ± standard deviation (SD) of triplicate samples from a representative experiment from over 20 individual studies. The main graph uses donors 2 and 3 (responder), while the insert uses donors 2 and 4 (responder). All values for the mPEG-derivatized cells different from control PBMC at P < .0001.
The loss of T-cell stimulation and activation is also evident in photomicrographs of the MLR. As shown in Fig 2, massive proliferation, cell spreading, and extensive foci of responder cells are seen in response to unmodified stimulator cells (Fig 2A). In contrast, the same population of responder cells do not recognize mPEG-modified stimulator cells (Fig 2B, 1.2 mmol/L mPEG/4 × 106 cells) as evidenced by both their rounded morphology and failure to proliferate (absence of 3H-thymidine incorporation; Fig 1).
Photomicrograph of lymphocyte proliferation in response to control (A) and mPEG-derivatized (B: 1.2 mmol/L mPEG/4 × 106 PBMC) stimulator PBMC. In (B), the PBMC remain small and rounded, a morphological feature characteristic of resting, nonproliferative lymphocytes, whereas in (A), the PBMC are larger and exhibit stellate protrusions typical of antigen-stimulated cells. Shown is the response of donor 4 to donor 1 (stimulator).
Photomicrograph of lymphocyte proliferation in response to control (A) and mPEG-derivatized (B: 1.2 mmol/L mPEG/4 × 106 PBMC) stimulator PBMC. In (B), the PBMC remain small and rounded, a morphological feature characteristic of resting, nonproliferative lymphocytes, whereas in (A), the PBMC are larger and exhibit stellate protrusions typical of antigen-stimulated cells. Shown is the response of donor 4 to donor 1 (stimulator).
Further supporting an abrogation in cellular response in the mPEG-treated MLR is the significantly decreased production of proinflammatory cytokines. For example, endogenous IL-2 production from MLR cocultures containing mPEG-derivatized PBMC (2.4 mmol/L mPEG/4 × 106 cells) exhibits an average decrease of 41.6% ± 12.3% (mean ± standard error of mean [SEM]; n = 4) as compared with the production of endogenous IL-2 generated by unmodified PBMC. Similar decreases (mean ± SEM) in the TNFα (69.8% ± 13.2%), IL-4 (89.6% ± 10.4%), and IFNγ (94.6 ± 3.7) cytokine levels are observed upon mPEG-modification of PBMC. Furthermore, even suppressor cytokines, such as IL-10, exhibit a significant decrease (81.7% ± 1.0%) in the pegylated PBMC indicating maintenance of a resting, naive, population.
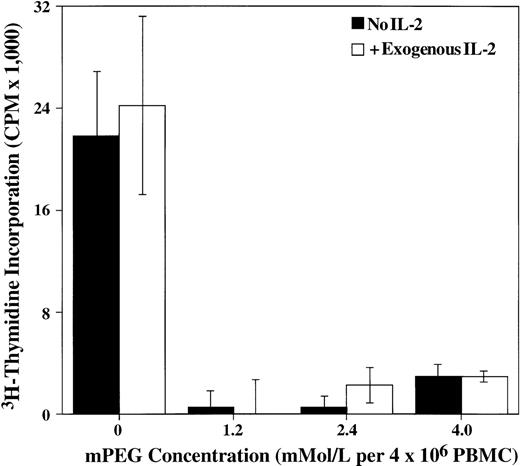
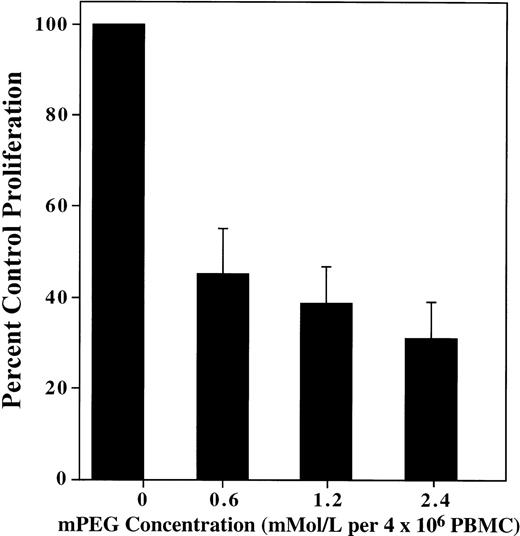
Moreover, the loss of proliferation is not solely due to decreased cytokine production. As shown in Fig 3, the addition of exogenous IL-2 to the MLR at concentrations normally used to enhance a T-cell response16 cannot reverse the attenuated immune response. This lack of IL-2–dependent proliferation suggests that the mPEG-modified responder T cells are not antigen primed (ie, are naive T cells) and therefore are unable to respond to the exogenous IL-2. Importantly, the loss of IL-2 enhancement is also not due to camouflaging of the IL-2 receptor. Using antibodies directed against the IL-2 receptor (CD25), it is observed that even at the highest rates of mPEG-derivatization, a < 35% decrease in receptor detection is noted immediately after modification (data not shown).
Proliferation of the mPEG-modified PBMC is not affected by the addition of exogenous IL-2, suggesting that these cells are not receiving the initial, antigen recognition signals necessary to evoke a proliferation response. Cell proliferation is measured by3H-thymidine incorporation into the DNA of responder cells (2.5 × 105 PBMC) in response to irradiated stimulator cells (2.5 × 105 PBMC) and 0.83 U/mL IL-2 present for the duration of the 4-day culture. The results shown are the mean ± SD of triplicate samples from a representative experiment of 4 independent studies using pegylated responder cells. All values for the mPEG-derivatized cells differ from control PBMC at P < .0001.
Proliferation of the mPEG-modified PBMC is not affected by the addition of exogenous IL-2, suggesting that these cells are not receiving the initial, antigen recognition signals necessary to evoke a proliferation response. Cell proliferation is measured by3H-thymidine incorporation into the DNA of responder cells (2.5 × 105 PBMC) in response to irradiated stimulator cells (2.5 × 105 PBMC) and 0.83 U/mL IL-2 present for the duration of the 4-day culture. The results shown are the mean ± SD of triplicate samples from a representative experiment of 4 independent studies using pegylated responder cells. All values for the mPEG-derivatized cells differ from control PBMC at P < .0001.
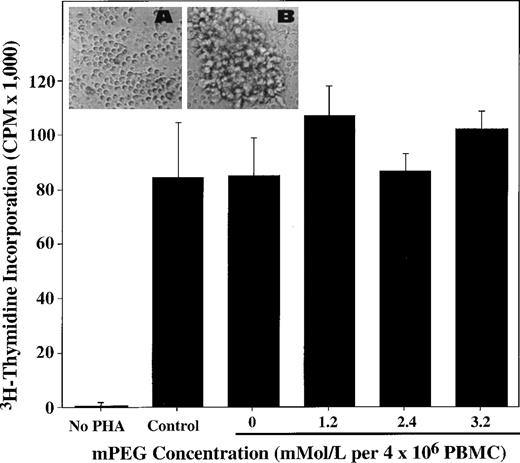
The loss of proliferative response is also not due to mPEG-mediated cytotoxicity. As shown in Table 2, virtually no difference in the viability of control and mPEG-modified PBMC is observed by propidium iodide analysis. Immediately after the preparation of the MLR, ≥92% of the control and derivatized responder cells are viable. Similarly, both the control and pegylated PBMC show virtually identical viability (≈ 60%) after 4 days in MLR culture. Further supporting the lack of mPEG-cytotoxicity is the finding that derivatization does not alter the proliferative potential of the PBMC. Stimulation of cellular proliferation of the mPEG-modified PBMC with the mitogen PHA (1 μg per 107 cells)20results in a normal proliferative response after 4 days of culture (Fig 4). Similar results are obtained with PHA stimulation before the pegylation procedure (data not shown). Hence, these data clearly indicate that loss of cellular viability or proliferation potential do not underlie the loss of MHC-mediated activation and proliferation.
Viability of mPEG-Modified PBMC Is Unaffected at Days 1 and 4 of MLR Culture
| Experimental Condition . | Day 1 Viability . | Day 4 Viability . |
|---|---|---|
| No treatment | 94.4% | 58.0% |
| Unmodified Controls (mPEG buffer only) | 98.2% | 59.2% |
| 1.2 mmol/L mPEG* | 92.7% | 63.5% |
| 2.4 mmol/L mPEG* | 96.2% | 63.2% |
| Experimental Condition . | Day 1 Viability . | Day 4 Viability . |
|---|---|---|
| No treatment | 94.4% | 58.0% |
| Unmodified Controls (mPEG buffer only) | 98.2% | 59.2% |
| 1.2 mmol/L mPEG* | 92.7% | 63.5% |
| 2.4 mmol/L mPEG* | 96.2% | 63.2% |
Shown are the results of a representative experiment of a minimum of 3 independent studies.
Per 4 × 106 PBMC.
No differences are observed in T-cell proliferation when control and mPEG-modified PBMC are exposed to the mitogen PHA. Cell proliferation is measured by 3H-thymidine incorporation into the DNA of PBMC (2.5 × 105 PBMC) in response to PHA stimulation for the duration of the 4-day culture (see Materials and Methods). The results shown are the mean ± SD of triplicate samples from a representative experiment of 4 independent studies. Insert: Photomicrographs of mPEG-derivatized lymphocytes (1.2 mmol/L mPEG per 4 × 106 PBMC) without PHA treatment (A) and with PHA treatment (B) after 4 days of culture.
No differences are observed in T-cell proliferation when control and mPEG-modified PBMC are exposed to the mitogen PHA. Cell proliferation is measured by 3H-thymidine incorporation into the DNA of PBMC (2.5 × 105 PBMC) in response to PHA stimulation for the duration of the 4-day culture (see Materials and Methods). The results shown are the mean ± SD of triplicate samples from a representative experiment of 4 independent studies. Insert: Photomicrographs of mPEG-derivatized lymphocytes (1.2 mmol/L mPEG per 4 × 106 PBMC) without PHA treatment (A) and with PHA treatment (B) after 4 days of culture.
To determine if the inhibition of MHC class II-dependent T-cell activation occurred as a consequence of altered cell-cell (T-cell APC) interaction, we investigated the antigenic recognition of adhesion and costimulatory molecules after cell surface derivatization with mPEG. It was our hypothesis that weakening of any of these interactions by mPEG-derivatization would impair both the initial cellular recognition and binding of the foreign MHC class II molecules to the T-cell receptor (TCR) complex, as well as the later costimulatory interactions, thus preventing T-cell activation and proliferation.21-23
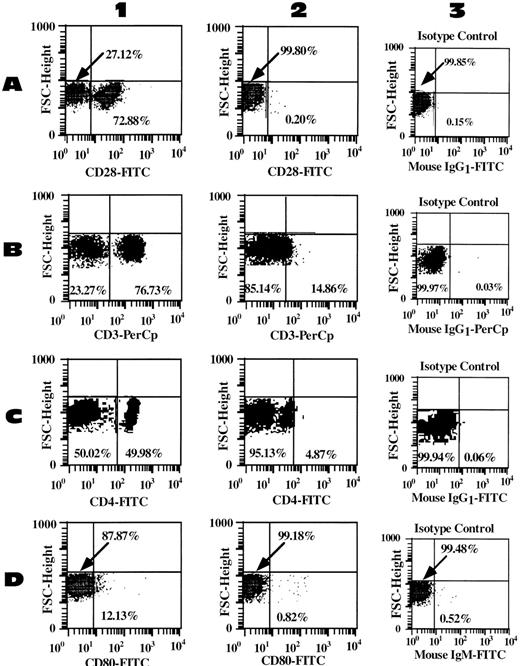
Indeed, flow cytometric analysis demonstrates that mPEG-modification results in a significant reduction in the detectable signal for a number of surface epitopes involved in cell activation and proliferation. As shown in Fig 5, mPEG modification effectively blocks antibody-mediated detection of CD28 (a costimulatory molecule present on T cells, which binds to CD80), CD3 (associated with the TCR and necessary for signal transduction), CD4 (coreceptor for MHC class II molecules and present on T cells), as well as CD80 (costimulatory molecule present on B cells and APC). Indeed, while 76.7% of the lymphocytes are initially CD3 positive, treatment with 0.6 and 2.4 mmol/L mPEG per 4 × 106 cells results in a dramatic decrease in antibody binding, such that only 25.9% and 14.9%, respectively, of the cells are seen as CD3+. Even more striking is the loss of detection of CD28+ cells. In the control population, 72.9% are CD28+, whereas in the 0.6 and 2.4 mmol/L mPEG-modified cells, only 33.3% and 0.20%, respectively, appeared as CD28+. Similarly, CD4 is effectively camouflaged by mPEG modification. While 50.0% of control PBMC are CD4+, only 4.9% of the mPEG-modified (2.4 mmol/L mPEG per 4 × 106) cell were positive. Of further interest was the change in CD80 (B7) present on B cells and APC. In control cells, 12.1% of the PBMC are CD80+, whereas after derivatization with 0.6 and 2.4 mmol/L mPEG per 4 × 106 cells, only 0.9% and 0.82% are positive, virtually identical to the isotype control (0.52%). Furthermore, as noted in Table 3, comparable findings of decreased antibody binding to surface determinants involved in antigen recognition and response are observed in both T cell (CD2, CD8, CD11a, and L-selectin) and APC (CD14, CD58, and L-selectin) populations. Interestingly, the very large HLA class II molecule on the APC is not significantly blocked by mPEG-derivatization.
Multiple cell determinants are effectively camouflaged by cell surface derivatization with mPEG. Shown are the scatter plot analyses for CD28 (A) costimulatory molecule present on T cells, binds to CD80; CD3 (B) associated with TCR on T cells and is necessary for signal transduction; CD4 (C) coreceptor for MHC class II molecules present on T cells); and CD80 (D) costimulatory molecule present on B cells and APC. Lane 1 represents the control unmodified PBMC; lane 2 represents the same PBMC population modified with 2.4 mmol/L mPEG (cell concentration of 4 × 106); while lane 3 represents the appropriate isotype control for the sample. In all cases, mPEG modification resulted in a significant decrease (P < .001) in antibody detection of the indicated cell marker. This decrease in antibody detection occurs in a dose-dependent manner upon increasing modification with mPEG (data not shown).
Multiple cell determinants are effectively camouflaged by cell surface derivatization with mPEG. Shown are the scatter plot analyses for CD28 (A) costimulatory molecule present on T cells, binds to CD80; CD3 (B) associated with TCR on T cells and is necessary for signal transduction; CD4 (C) coreceptor for MHC class II molecules present on T cells); and CD80 (D) costimulatory molecule present on B cells and APC. Lane 1 represents the control unmodified PBMC; lane 2 represents the same PBMC population modified with 2.4 mmol/L mPEG (cell concentration of 4 × 106); while lane 3 represents the appropriate isotype control for the sample. In all cases, mPEG modification resulted in a significant decrease (P < .001) in antibody detection of the indicated cell marker. This decrease in antibody detection occurs in a dose-dependent manner upon increasing modification with mPEG (data not shown).
Percent Binding of Monoclonal Antibodies to the Surface of Control and mPEG-Modified PBMC (dosage of mPEG per 4 × 106 PBMC)
| CD Molecule . | Function (cell type found on) . | Control PBMC . | mPEG-Modified PBMC . | |
|---|---|---|---|---|
| 0.6 mMol/L . | 2.4 mmol/L . | |||
| CD2 (LFA-2) | Adhesion molecule (T cell) | 82.3% | 77.3% | 31.6% |
| CD62L (L-selectin) | Adhesion molecule (APC and T cells) | 77.8% | 65.9% | 52.4% |
| CD11a (LFA-1) | Adhesion molecule (APC and T cells) | 94.0% | 82.3% | 43.9% |
| CD58 (LFA-3) | Adhesion molecule (APC and T cells) | 47.6% | 54.2% | 26.5% |
| CD8 | Binds MHC class I (TK cell) | 24.4% | ND | 0.06% |
| HLA class II | Present peptide (APC) | 8.9% | 11.8% | 10.1% |
| CD Molecule . | Function (cell type found on) . | Control PBMC . | mPEG-Modified PBMC . | |
|---|---|---|---|---|
| 0.6 mMol/L . | 2.4 mmol/L . | |||
| CD2 (LFA-2) | Adhesion molecule (T cell) | 82.3% | 77.3% | 31.6% |
| CD62L (L-selectin) | Adhesion molecule (APC and T cells) | 77.8% | 65.9% | 52.4% |
| CD11a (LFA-1) | Adhesion molecule (APC and T cells) | 94.0% | 82.3% | 43.9% |
| CD58 (LFA-3) | Adhesion molecule (APC and T cells) | 47.6% | 54.2% | 26.5% |
| CD8 | Binds MHC class I (TK cell) | 24.4% | ND | 0.06% |
| HLA class II | Present peptide (APC) | 8.9% | 11.8% | 10.1% |
Abbreviation: ND, not determined.
While the PBMC proliferative response to MHC class II disparate cells was shown to be effectively blunted, we were also interested in what effect mPEG-modification has on exogenous antigen presentation. Consequently, we examined the proliferative response of control and pegylated PBMC to tetanus toxoid. Interestingly, the proliferative response of human PBMC to tetanus toxoid is invariably a memory response. This is of importance because memory responses can be of significant consequence in transfusion/transplantation medicine. As shown in Fig 6, levels of mPEG modification (eg 2.4 mmol/L per 4 × 106 PBMC) that completely abrogated recognition of foreign PBMC also has a significant, but much lesser, effect on the proliferative response to tetanus toxoid (P < .001). These data indicate that mPEG-derivatization cannot only significantly attenuate antigen presentation/activation, but can also inhibit memory cell responses.
T-cell proliferation in response to tetanus toxoid challenge is decreased after mPEG-derivatization. However, the loss of proliferation is significantly less than that observed after exposure to disparate MHC-Class II antigens (see Fig 1; eg, ≈ 60% v>95% at 1.2 mmol/L mPEG per 4 × 106 PBMC). Shown is the mean ± SEM tetanus toxoid-dependent proliferation of pegylated PBMC relative to control cells of 4 independent experiments.
T-cell proliferation in response to tetanus toxoid challenge is decreased after mPEG-derivatization. However, the loss of proliferation is significantly less than that observed after exposure to disparate MHC-Class II antigens (see Fig 1; eg, ≈ 60% v>95% at 1.2 mmol/L mPEG per 4 × 106 PBMC). Shown is the mean ± SEM tetanus toxoid-dependent proliferation of pegylated PBMC relative to control cells of 4 independent experiments.
Thus, mPEG modification of either the responder or stimulator PBMC effectively attenuates/prevents MHC class II-mediated activation and proliferation of foreign lymphocytes. The loss of proliferation is likely mediated via altered cell:cell communication between the APC and T cell arising from the camouflage of crucial cellular determinants involved in cell:cell adhesion and in the costimulatory signals required for T-cell activation and proliferation. In addition, these data suggest that the covalent modification of PBMC can also decrease antigen-specific and recall antigen-dependent proliferation.
DISCUSSION
The MLR is a very sensitive measure of histocompatibility between the donor and recipient, as it measures the antigenic variance within the HLA class II complex (the primary antigens responsible for tissue compatibility in transplants). Indeed, before the use of immunosuppressive therapy (eg, cyclosporin), this assay, although time consuming, was perhaps the best indicator of the probability of both graft survival in an organ recipient and the onset and severity of GVHD. Consequently, the MLR assay is particularly well suited to examine whether mPEG modification could effectively attenuate the risk of GVHD due to lymphocyte contamination of blood products.
Our studies demonstrate that mPEG-derivatization of PBMC effectively abrogates allospecific, MHC class II-mediated T-cell activation. The initial T cell-APC communication is dependent on the interaction of adhesion molecules such as the T cell’s CD2 (lymphocyte function-associated antigen [LFA]-2) ligand binding to CD58 (LFA-3) on the APC.24 Subsequent to this event, cell:cell interaction is further stabilized by the binding of CD11a/CD18 (LFA-1) on the T cell to CD54 (intracellular adhesion molecule [ICAM]-1) on the APC.25 Initially, all of these interactions are of relatively low-affinity, but coupling of the TCR complex (CD3-TCR) and CD4 molecule with the MHC class II ligands on the APC leads to conformational changes in CD11a resulting in high-affinity binding to CD54.26-28 Once the TCR-MHC class II interaction is engaged, the T-cell proliferative response is fully dependent on secondary costimulatory events such as the interaction of CD28 (T cell) with CD80 (B7; APC). The CD28-CD80 interaction provides a sufficient secondary signal to induce T-cell proliferation and cytokine production.
As a consequence of the global camouflage imparted by cell surface pegylation, the signals necessary to initiate T-cell activation, cytokine production, and subsequent T-cell proliferation are not generated. Indeed, these pegylated cells morphologically resemble resting PBMC even after 4 days of culture in a MLR. The lack of antigen priming is further suggested by the failure of exogenous IL-2 to override the mPEG-dependent inhibition. Because IL-2 is largely responsible for the stimulation and proliferation of activated T cells, the failure of exogenous IL-2 to induce MLR proliferation in the mPEG-modified PBMC strongly suggests that the primary immune recognition/interactions (eg, adhesion, TCR-MHC) between the allogeneic APC and T cells have not occurred.
Interestingly, surface camouflage of the PBMC population does not entirely prevent T activation and proliferation in response to other antigens (tetanus toxoid) or mitogens (PHA). This clearly demonstrates that the pegylated PBMC are viable and have the identical proliferation potential (in the case of PHA) as the unmodified cells. The difference in the response between a singular antigen, such as tetanus toxoid, and a complex antigen (eg, HLA disparate cell) perhaps lies in the phenotype of T-cell response stimulated for each antigen condition. In a 1-way MLR, T-cell recognition to disparate HLA-class II cells occurs through direct recognition of foreign APC (foreign MHC and peptide) as well as some presentation of these cells by responder APC (self MHC and foreign peptide).29 The responder T-cell population recognizing the alloantigens are polyclonal naive T cells. In contrast, the T lymphocytes responding to tetanus toxoid antigen are primarily clonal memory cells. The differences between initiating a naive versus memory T-cell response may provide an explanation for the less effective attenuation of the tetanus toxoid response. For example, the binding of soluble anticlass II immunoglobulins (eg, lymphocyte activation gene-3 [LAG-3]-Ig) to PBMC results in blocked allospecific T-cell proliferation, but normal mitogen and recall antigen proliferation.30
However, the antiactivation/proliferation mechanism of mPEG-derivatization of cells is in contrast to other methods of preventing naive T-cell activation (eg, blocking antibodies [anti-CD2 and anti-CD3]31 or soluble ligands [LAG-3-Ig and cytotoxic T-lymphocyte antigen-4 (CTLA-4) Ig]32). As shown in Fig 5 and Table 3, the immunosuppressive action of PBMC pegylation arises from a global camouflage of the cell and the simultaneous inhibition of the numerous sites and pathways involved in T-cell activation and proliferation. This has multiple advantages over the use of a signal blocking antibody or ligand in that redundant activation pathways may be simultaneously blocked/inhibited. In addition, the pegylation of blood products is likely to be much more cost effective than the use of large quantities of blocking antibodies.
Based on these and our previous findings,9-12 the use of mPEG-modified blood or blood components could effectively decrease allosensitization rates in transfused patients and diminish the risk of GVHD in immunosuppressed patients. However, the immunomodulatory effects of mPEG-modification may not be limited to RBC or lymphocytes. Because immunoprotective levels of mPEG-modification do not affect cellular structure, function, or viability of a wide range of cell types (eg, RBC, lymphocyte, epithelial cells, endothelial cells, and monocytes),9-12 it may be possible to translate these findings to other instances of tissue transplantation. A particularly attractive application would be the infusion of an activated mPEG solution into the vasculature of organ graft to derivatize the endothelium with covalently bound mPEG. The modified endothelium might well become antigenically inert and prevent the initial binding of preformed antibodies (hence, complement activation), as well as decrease cell-cell interactions (eg, leukocyte rolling, adhesion, and migration) responsible for hyperacute rejection.10,12 This would be of potential therapeutic benefit in decreasing or preventing both hyperacute and acute tissue rejection with a consequent increase in the pool of available donor organs (both allogeneic and xenogeneic).12 33-35
In summary, these data demonstrate that mPEG-modification of lymphocytes can effectively block MHC class II-mediated, allospecific T-cell activation, as well as significantly attenuate antigen-specific and memory cell-dependent activation and proliferation. The loss of responsiveness is likely due to altered cell-cell interaction via reduced recognition and binding between the adhesion molecules and receptor/ligand requirements involved in the early stages of T cell-APC interaction and activation. These findings suggest that mPEG-modification of passenger leukocytes still present in blood products even after leukoreduction may prove to be an effective means of preventing activation and proliferation of the donor T cells in response to MHC disparate host tissue. Consequently, the use of pegylated blood products may prove beneficial in the treatment of immunosuppressed patients, as well as the chronically transfused.9-12
Supported by National Institutes of Health Grants No. HL53066 (to M.D.S.), HL58584 (to M.D.S.), and AI35327 (to E.J.G.) and by Cooley’s Anemia Foundation (K.L.M.).
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Mark D. Scott, PhD, Division of Experimental Pathology, Department of Pathology and Laboratory Medicine MC-81, Albany Medical College, 47 New Scotland Ave, Albany, NY 12208; e-mail: mscottpath@aol.com.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal