Abstract
Paroxysmal nocturnal hemoglobinuria (PNH) is a clonal stem cell disorder caused by a somatic mutation of the PIGA gene. The product of this gene is required for the biosynthesis of glycosylphosphatidylinositol (GPI) anchors; therefore, the phenotypic hallmark of PNH cells is an absence or marked deficiency of all GPI-anchored proteins. Aerolysin is a toxin secreted by the bacterial pathogen Aeromonas hydrophila and is capable of killing target cells by forming channels in their membranes after binding to GPI-anchored receptors. We found that PNH blood cells (erythrocytes, lymphocytes, and granulocytes), but not blood cells from normals or other hematologic disorders, are resistant to the cytotoxic effects of aerolysin. The percentage of lysis of PNH cells after aerolysin exposure paralleled the percentage of CD59+ cells in the samples measured by flow cytometry. The kinetics of red blood cell lysis correlated with the type of PNH erythrocytes. PNH type III cells were completely resistant to aerolysin, whereas PNH type II cells displayed intermediate sensitivity. Importantly, the use of aerolysin allowed us to detect PNH populations that could not be detected by standard flow cytometry. Resistance of PNH cells to aerolysin allows for a simple, inexpensive assay for PNH that is sensitive and specific. Aerolysin should also be useful in studying PNH biology.
PAROXYSMAL NOCTURNAL hemoglobinuria (PNH) is an acquired hematopoietic stem cell disorder manifested by abnormal hematopoiesis, complement-mediated intravascular hemolysis, and a propensity toward thrombosis.1 The disease usually results from a somatic mutation in the X-linked gene, PIGA.2-5 The product of this gene is necessary for the first step in the biosynthesis of glycosylphosphatidylinositol (GPI) anchors; hence, cells harboring PIGA mutations are characterized by a deficiency, absolute or partial, of all proteins affixed to the cell membrane in this way. GPI-anchored proteins have been shown to be involved in a wide range of important cell functions, including signal transduction6,7 and trafficking of apically expressed epithelial proteins.8,9 They may also play a role in regulating apoptosis.10 Two GPI-anchored proteins, CD55 (decay accelerating factor) and CD59 (membrane inhibitor of reactive lysis), normally protect cells from the action of homologous complement, and it is their absence that leads to the hemolytic anemia associated with PNH.11 12
Aerolysin is a toxin secreted by the human bacterial pathogenAeromonas hydrophila and is perhaps the best characterized member of a large group of water-soluble proteins that are capable of killing target cells by forming channels in their membranes (see Parker et al13 for a recent review). Members of the group include a wide variety of virulence factors, such as Staphylococcus aureus α toxin and aerolysin itself, as well as the T-cell defense protein perforin. All of these proteins are able to undergo a transformation from a water-soluble to an insertion-competent state by oligomerizing to form amphipathic barrels.
Aerolysin is secreted as a completely inactive protoxin that is converted to the active form by proteolytic removal of a C-terminal peptide.14 A number of mammalian proteases can activate proaerolysin, including trypsin, chymotrypsin, and furin.15Cells that are sensitive to aerolysin, such as T lymphocytes (which are killed by 1 hour of exposure to as little as 10−11mol/L toxin), contain specific high-affinity receptors that serve to concentrate the toxin on the cell surface, promoting insertion.16 Proaerolysin can also bind to the receptors, but it is unable to oligomerize and therefore cannot form channels.17
We have recently identified a number of proteins that can act as aerolysin receptors.18-20 Among them are Thy-1 from brain and T lymphocytes, contactin from brain, the variant surface glycoprotein (VSG) of trypanosomes, and a novel erythrocyte glycoprotein (EAR). These proteins share one remarkable property: they are all attached to the plasma membrane with GPI anchors. Importantly, we demonstrated that the anchor itself is a primary determinant of aerolysin binding.20 In addition, we showed that mutant mouse T-cell lines that are unable to synthesize GPI-anchors are far less sensitive to aerolysin than normal cells.19 In this report, we show that human PNH cells are also resistant to the cytotoxic effects of aerolysin. This provides a sensitive and specific assay for PNH that is rapid and inexpensive.
MATERIALS AND METHODS
Cell lines.
The GPI-anchor deficient lymphoblastoid cell lines, LD− and JY5, harbor previously characterized PIGA mutations.10,21 An expression vector containing the full-length PIGA cDNA was stably transfected into the LD− and JY5 cell lines to establish the GPI-anchor replete cell lines, LD−(PIGA+) and JY5(PIGA+), as previously described.10 All cell lines were maintained in RPMI 1640 medium (GIBCO, Gaithersburg, MD) with 10% heat-inactivated fetal calf serum. To measure CD59 expression, cells were washed in RPMI with 0.2% fetal calf serum, stained for CD59 with a fluorescein isothiocyanate-conjugated monoclonal antibody (MoAb; Research Diagnostics, Flanders, NJ), and analyzed by flow cytometry (FACscan; Becton Dickinson, San Jose, CA).
Preparation of cells for aerolysin assay.
Venous peripheral blood from patients with PNH, normal controls, or disease controls was drawn into EDTA-containing tubes after informed consent as approved by the Joint Committee on Clinical Investigation of the Johns Hopkins Hospital. The blood was centrifuged at 400gfor 10 minutes and then the buffy coat was removed and the remaining erythrocytes were washed two times in phosphate-buffered saline (PBS) and resuspended in PBS to a concentration of 0.8%. Peripheral blood granulocytes were isolated using Ficoll/Hypaque (density, 1.119 g/mL) as previously described.22
Titer assay of aerolysin-induced hemolysis.
Aerolysin (1.5 × 10−6 mol/L), produced by trypsin activation of proaerolysin as described,15 was diluted 1:16 in PBS to a final volume of 100 μL and added to the first well of a 96-well plate. An equal volume of PBS was then added to the first well (1:32 aerolysin) and 1:2 serial dilutions were made across the plate. One hundred microliters of 0.8% red blood cells was added to all wells, and the plate was incubated at 37°C. Absorbance at 620 nm was measured using a plate reader (Biotek Instruments, Inc, Winooski, VT) at times 0, 5, 10, 15, and 20 minutes. Aerolysin and proaerolysin are available from Protox Biotech (Victoria, British Columbia, Canada).
Spectrophotometric assay of aerolysin-induced hemolysis.
Activated aerolysin was added to stirred cuvettes containing 1.5 mL of 0.8% vol/vol washed erythrocytes in PBS (10 mmol/L NaH2PO4, 150 mmol/L NaCl, pH 7.4) to a final concentration of 8 nmol/L. The rate of hemolysis was determined by measuring the change in optical density of the erythrocytes (which is due to a decrease in light scattering as the cells lyse) at 600 nm and 37°C as a function of time. The instrument used was a Varian Cary 1 (Varian Instruments, Houston, TX) recording spectrophotometer.
Propidium iodide staining for viability.
Cells were suspended to 1 × 106/mL in 0.5 mL PBS. Fifty microliters of propidium iodide (10 μg/mL in PBS) was added to each tube and the mixture was incubated for 5 minutes at 37°C. Approximately 10,000 data events per sample were collected for analysis on a FACSCAN flow-cytometer (BDIS, Mansfield, MA). Subcellular debris and remaining erythrocytes were excluded with a forward-scatter (FS)/90°-scatter (SS) gate. Viable cells were those exhibiting no fluorescence (propidium iodide excluding).
Detection of aerolysin-binding proteins by Western blotting.
Samples of cells dissolved in sample buffer were separated by sodium dodecyl sulfate-polyacrylamide electrophoresis (SDS-PAGE) using the method of Neville.23 Proteins were blotted onto nitrocellulose and the blots were developed by sandwich Western blotting as described by Nelson et al.19 This involved incubation with 2 × 10−8 mol/L proaerolysin, followed by polyclonal antiaerolysin and antirabbit horseradish peroxidase. Blots were then developed by enhanced chemiluminescence (ECL; Amersham Corp, Arlington Heights, IL).
RESULTS
Aerolysin-induced hemolysis of PNH erythrocytes.
In PNH, all hematopoietic lineages have a proportion of GPI-anchor deficient cells, because the PIGA mutation initially occurs in a pluripotent hematopoietic stem cell.1 The proportion for individual cell types can be estimated by measuring the fraction of cells that lack CD59 by flow cytometry, although this is an expensive procedure requiring complex instrumentation that is not widely available.24 25
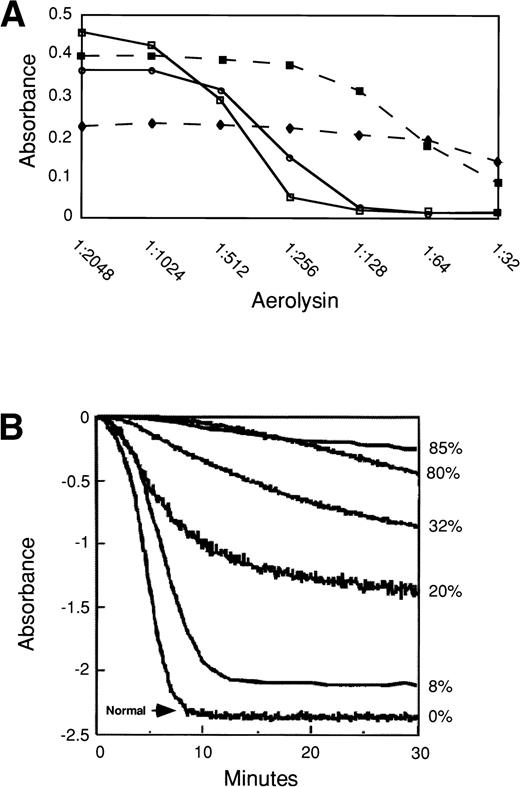
Based on our previous work, we expected the population of GPI-anchor deficient cells in a PNH blood sample to be relatively resistant to aerolysin compared with the normal, GPI-anchor replete cells.19 We initially performed a dose-response curve to compare the sensitivity of normal erythrocytes and PNH erythrocytes to various concentrations of aerolysin. Normal erythrocytes, but not PNH erythrocytes, were completely lysed after exposure to a 1:128 dilution of aerolysin (1.5 × 10-6 mol/L stock solution) for 10 minutes at 37°C (Fig 1A). The sensitivity of red blood cell lysis at a given dose of aerolysin varied depending on whether the PNH patient had predominantly type II cells (▪) or type III cells (⧫).
Aerolysin assays for detection of PNH. (A) Dose-response curve showing aerolysin sensitivity of two normal (solid lines, open symbols) versus two PNH (dashed lines, solid symbols) erythrocytes. (▪) Cells that are primarily type II erythrocytes; (⧫) type III cells. Serial dilutions of activated aerolysin (1.5 × 10−6 stock) were performed in a 96-well plate and mixed with an equal volume of 0.8% erythrocytes. Absorbance at 620 nm was measured after 10 minutes at 37°C using a plate reader. (B) Kinetic analysis of aerolysin-induced hemolysis of normal erythrocytes (bottom line) and erythrocytes from 5 different PNH patients. The rate of hemolysis was determined by measuring the change in optical density of erythrocytes at 600 nm and 37°C as a measure of time using a spectrophotometer. The percentage of CD59− erythrocytes determined by flow cytometry for each patient is shown to the right of the figure. (C) Flow cytometric analysis for CD59 expression of PNH red blood cells from the patient with 8% type III PNH erythrocytes (solid line) and a normal control (dotted line). (D) Flow cytometric analysis for CD59 expression of PNH red blood cells from the patient with 80% PNH erythrocytes (solid line) and a normal control (dotted line). The majority of cells represent type II PNH erythrocytes.
Aerolysin assays for detection of PNH. (A) Dose-response curve showing aerolysin sensitivity of two normal (solid lines, open symbols) versus two PNH (dashed lines, solid symbols) erythrocytes. (▪) Cells that are primarily type II erythrocytes; (⧫) type III cells. Serial dilutions of activated aerolysin (1.5 × 10−6 stock) were performed in a 96-well plate and mixed with an equal volume of 0.8% erythrocytes. Absorbance at 620 nm was measured after 10 minutes at 37°C using a plate reader. (B) Kinetic analysis of aerolysin-induced hemolysis of normal erythrocytes (bottom line) and erythrocytes from 5 different PNH patients. The rate of hemolysis was determined by measuring the change in optical density of erythrocytes at 600 nm and 37°C as a measure of time using a spectrophotometer. The percentage of CD59− erythrocytes determined by flow cytometry for each patient is shown to the right of the figure. (C) Flow cytometric analysis for CD59 expression of PNH red blood cells from the patient with 8% type III PNH erythrocytes (solid line) and a normal control (dotted line). (D) Flow cytometric analysis for CD59 expression of PNH red blood cells from the patient with 80% PNH erythrocytes (solid line) and a normal control (dotted line). The majority of cells represent type II PNH erythrocytes.
We also performed a kinetic analysis of normal and PNH erythrocytes after exposure to aerolysin. The spectrophotometric assay we used depends on the decrease in light scattering that accompanies erythrocyte lysis. Aerolysin (8 nmol/L) resulted in the complete hemolysis of erythrocytes from normals within approximately 10 minutes (Fig 1B). The time course was highly reproducible from one normal sample to another. The proportion of unlysed cells, which should correspond to those cells that did not display GPI-anchored proteins, could easily be calculated. For every patient, the value that was obtained corresponded very closely with the proportion of cells that lacked CD59, as determined by flow cytometry (Fig 1B). Furthermore, flow cytometric analysis showed that the cells remaining after exposure to aerolysin were CD59− (data not shown).
Although all PNH samples showed patterns that were easily distinguished from the controls, the kinetics of erythrocyte lysis was dependent on the type of PNH erythrocytes tested. Patients with predominantly type III PNH cells that completely lack GPI-anchors (eg, the patients with 85%, 20%, and 8% PNH cells; Fig 1C) exhibited a plateau of resistant cells after 10 minutes in aerolysin that matched the frequency of PNH cells in the patient (Fig 1B). In contrast, patients with a predominance of PNH type II cells (eg, the patients with 80% and 32% PNH cells; Fig 1D) showed slow ongoing lysis over time (Fig 1B).
To determine if the assay was specific for PNH, aerolysin sensitivity of erythrocytes from patients with various hematologic disorders was measured. In every disease state we tested, including myelodysplastic syndromes, aplastic anemia, hemolytic anemias, myeloproliferative disorders, and leukemias, we found that the cells were as sensitive as normal erythrocytes to the lytic effects of aerolysin (Fig 2). Absorbance greater than 0.1 10 minutes after exposure to a 1:128 dilution of aerolysin (1.5 × 10-6 mol/L stock) distinguished PNH from normals and from other hematologic disorders (Fig 2).
Aerolysin assay is specific for PNH. Mean absorbance of erythrocytes from 7 normal controls (dots), 3 PNH patients (shaded), and 20 disease controls (slanted lines) after 10 minutes of exposure to a 1:128 dilution of aerolysin (1 × 10−8 mol/L). Disease controls consisted of myelodysplastic syndromes (7), aplastic anemia (5), polycythemia vera (2), myelofibrosis (2), sickle cell anemia (1), autoimmune hemolytic anemia (1), iron deficiency anemia (1), and acute myelogenous leukemia (1). Error bars represent the standard deviation.
Aerolysin assay is specific for PNH. Mean absorbance of erythrocytes from 7 normal controls (dots), 3 PNH patients (shaded), and 20 disease controls (slanted lines) after 10 minutes of exposure to a 1:128 dilution of aerolysin (1 × 10−8 mol/L). Disease controls consisted of myelodysplastic syndromes (7), aplastic anemia (5), polycythemia vera (2), myelofibrosis (2), sickle cell anemia (1), autoimmune hemolytic anemia (1), iron deficiency anemia (1), and acute myelogenous leukemia (1). Error bars represent the standard deviation.
Sensitivity of PNH leukocytes to aerolysin.
A major advantage of using flow cytometry over tests based on complement sensitivity of erythrocytes (ie, sucrose hemolysis and Ham test) is that immunophenotyping can detect abnormalities in multiple hematopoietic lineages. To determine whether the aerolysin assay could detect a GPI-anchor deficiency in nucleated cells as well as in erythrocytes, the toxin was incubated with two PNH cell lines, LD− and JY5, that harbor a previously characterized PIGA mutation and, hence, fail to express GPI-anchored proteins. The absence of GPI anchors was confirmed using an aerolysin sandwich Western blotting procedure (Fig 3) and flow cytometric analysis for CD59 expression (Fig 4A and C). The LD−and JY5 cell lines were essentially unaffected by 6 nmol/L aerolysin (Fig 4B and D). In contrast, the same dose of aerolysin produced rapid death of the same cell lines stably transfected with the full-length cDNA for PIGA (Fig 4B and D).
PNH cells lack proaerolysin binding proteins. Proaerolysin binding to proteins from LD− cells (lane 1), LD−(PIGA+) cells (lane 2), and CEM cells (lane 3). Equal numbers of cells (6 × 104/lane) were applied to each lane. Lane 1 ( LD− cells) is blank, whereas lane 2 [LD−(PIGA+)] has multiple bands. For the sake of comparison, an immature human T-cell line (CEM) was also run in this experiment. A band corresponding to Thy-1, which we have detected previously in mouse T cells, is easily visible in the figure.
PNH cells lack proaerolysin binding proteins. Proaerolysin binding to proteins from LD− cells (lane 1), LD−(PIGA+) cells (lane 2), and CEM cells (lane 3). Equal numbers of cells (6 × 104/lane) were applied to each lane. Lane 1 ( LD− cells) is blank, whereas lane 2 [LD−(PIGA+)] has multiple bands. For the sake of comparison, an immature human T-cell line (CEM) was also run in this experiment. A band corresponding to Thy-1, which we have detected previously in mouse T cells, is easily visible in the figure.
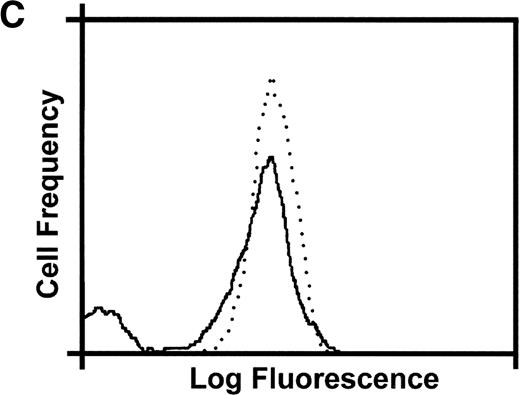
Restoration of GPI-anchor expression in PNH cell lines overcomes resistance to aerolysin. Flow cytometric analysis for CD59 expression of LD− and JY5 cells before (solid line) and after (dotted line) stable transfection of the PIGA cDNA (A and C). (B) Viability of LD− (solid line) and LD−PIGA+ (dotted line) cells after exposure to 1 nmol/L aerolysin at 37°C. (D) Viability of JY5 (solid line) and JY5PIGA+ (dotted line) cells after exposure to 1 nmol/L aerolysin at 37°C. Cell viability was determined in triplicate at 5-minute intervals. Error bars represent the standard deviations.
Restoration of GPI-anchor expression in PNH cell lines overcomes resistance to aerolysin. Flow cytometric analysis for CD59 expression of LD− and JY5 cells before (solid line) and after (dotted line) stable transfection of the PIGA cDNA (A and C). (B) Viability of LD− (solid line) and LD−PIGA+ (dotted line) cells after exposure to 1 nmol/L aerolysin at 37°C. (D) Viability of JY5 (solid line) and JY5PIGA+ (dotted line) cells after exposure to 1 nmol/L aerolysin at 37°C. Cell viability was determined in triplicate at 5-minute intervals. Error bars represent the standard deviations.
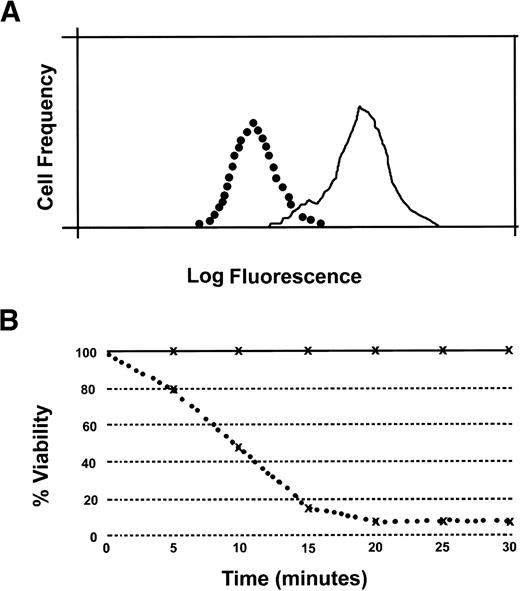
The percentage of PNH granulocytes in the circulation most accurately reflects the size of the PNH clone, because the survival of PNH granulocytes is normal or even increased,10,26,27 whereas erythrocyte survival is decreased.28 Therefore, we sought to determine the sensitivity of PNH granulocytes to aerolysin. Granulocytes from patients with PNH and from normal controls were separated, treated with aerolysin, and analyzed using flow cytometry to assess their ability to exclude propidium iodide. Forty minutes after exposure to 2.5 × 10−8 mol/L aerolysin, less than 10% of normal granulocytes excluded propidium iodide (Fig 5B). In contrast, more than 90% of PNH granulocytes retained their ability to exclude propidium iodide under identical conditions (Fig 5D). Granulocytes from disease controls were as sensitive to the toxin as cells from normal controls (data not shown), demonstrating that the ability to exclude propidium iodide after exposure to aerolysin was specific for PNH cells. The percentage of PNH granulocytes that was resistant to aerolysin correlated with the percentage of cells lacking CD59 expression (data not shown).
PNH granulocytes are resistant to aerolysin. Representative example of normal and PNH granulocytes stained with propidium iodide before (A and C) and 40 minutes after (B and D) incubation with 1 nmol/L activated aerolysin. Propidium iodide uptake was assayed using flow cytometry.
PNH granulocytes are resistant to aerolysin. Representative example of normal and PNH granulocytes stained with propidium iodide before (A and C) and 40 minutes after (B and D) incubation with 1 nmol/L activated aerolysin. Propidium iodide uptake was assayed using flow cytometry.
Sensitivity of aerolysin assay for PNH.
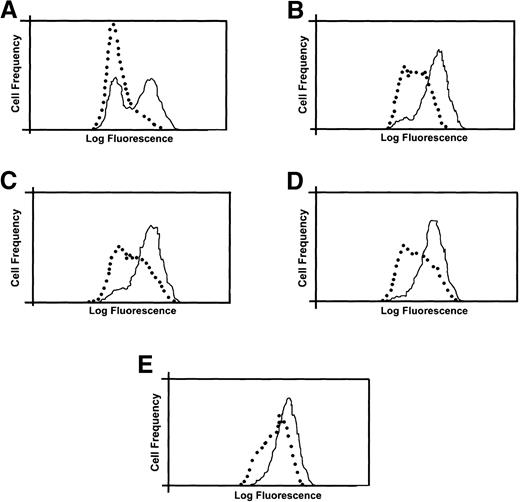
We next tested a known mixture of LD− and LD−(PIGA+) to determine how accurately the new assay could determine the percentage of GPI-anchor deficient cells in a mixed population (10% PNH cells). Similar to the above-mentioned experiments in erythrocytes, the assay accurately determined the percentage of PNH cells in the population (Fig 6). The lower limit of detection of a PNH population using flow cytometry is 1% to 5%.24 25 To determine whether aerolysin could be used to detect smaller PNH populations than this, we mixed PNH cells (LD−) with increasing numbers of GPI anchor protein replete cells (CEM) and assayed CD59 expression before and after exposure to aerolysin (Fig 7). Before the addition of aerolysin, PNH cells were undetectable when they comprised less than 1% of the population; however, 30 minutes after exposure to aerolysin, PNH populations as small as 0.1% were detected.
Aerolysin sensitivity correlates CD59 expression in PNH cell lines. Representative example showing correlation between aerolysin sensitivity and flow cytometric detection of CD59 in PNH cell lines. (A) Flow cytometric analysis for CD59 expression in a population of cells consisting of 90% LD−PIGA+ cells and 10% LD− cells (solid line). LD− cells are depicted by the dotted line. (B) The percentage of viability of the LD− (solid line) and mixed cell (dotted line) populations after exposure to 1 nmol/L aerolysin at 37°C. Cell viability was determined by trypan blue exclusion at 5-minute intervals.
Aerolysin sensitivity correlates CD59 expression in PNH cell lines. Representative example showing correlation between aerolysin sensitivity and flow cytometric detection of CD59 in PNH cell lines. (A) Flow cytometric analysis for CD59 expression in a population of cells consisting of 90% LD−PIGA+ cells and 10% LD− cells (solid line). LD− cells are depicted by the dotted line. (B) The percentage of viability of the LD− (solid line) and mixed cell (dotted line) populations after exposure to 1 nmol/L aerolysin at 37°C. Cell viability was determined by trypan blue exclusion at 5-minute intervals.
Use of aerolysin to detect small PNH populations. LD− cells (10,000) were mixed with CD59-expressing CEM cells 1:1 (A), 1:10 (B), 1:100 (C), 1:500 (D), and 1:1,000 (E) and analyzed for expression of CD59 before (solid line) and after (dotted line) 30 minutes of exposure to 1 nmol/L aerolysin.
Use of aerolysin to detect small PNH populations. LD− cells (10,000) were mixed with CD59-expressing CEM cells 1:1 (A), 1:10 (B), 1:100 (C), 1:500 (D), and 1:1,000 (E) and analyzed for expression of CD59 before (solid line) and after (dotted line) 30 minutes of exposure to 1 nmol/L aerolysin.
PNH can arise de novo or evolve from aplastic anemia, suggesting a pathophysiologic link between the two diseases.29 30 To test whether the use of aerolysin in conjunction with flow cytometry could detect small PNH populations, we used this assay to study the peripheral blood from an aplastic anemia patient who did not respond to immunosuppressive therapy. Before adding aerolysin, we were unable to detect PNH erythrocytes using standard flow cytometry; however, 15 minutes after exposure to 5 × 10-9 mol/L aerolysin, a small population of PNH cells was detected (Fig 8). Because aerolysin depleted the erythrocyte population by 2.5 to 3 logs (determined by counting on a hemacytometer), we calculated that this represents a PNH population of less than 0.075%. A similar result was obtained in a patient with a 1-year history of moderate aplastic anemia; no PNH cells could be detected in the peripheral blood of three normal control subjects treated in an identical manner (data not shown).
Use of aerolysin to detect a minor population of PNH cells in patient with aplastic anemia. Two-color histogram of peripheral blood cells stained with MoAb directed against CD59 antigen (FITC) and MoAb directed against glycophorin-A (PE) before (A) and after (B) exposure to aerolysin (5 × 10−9 mol/L for 15 minutes). Axis represent log red (PE) or log green (FITC) fluorescence intensity.
Use of aerolysin to detect a minor population of PNH cells in patient with aplastic anemia. Two-color histogram of peripheral blood cells stained with MoAb directed against CD59 antigen (FITC) and MoAb directed against glycophorin-A (PE) before (A) and after (B) exposure to aerolysin (5 × 10−9 mol/L for 15 minutes). Axis represent log red (PE) or log green (FITC) fluorescence intensity.
DISCUSSION
We found that a simple, inexpensive assay that measures the absorbance of cells after exposure to 1 × 10−8 mol/L aerolysin for 10 minutes can reliably distinguish PNH cells from normals and other disease states (Figs 1 and 2). The presence of GPI-anchored proteins on cells sensitizes them to aerolysin because these proteins act as toxin receptors and binding promotes oligomerization and channel formation. PNH cells are less sensitive to the toxin because they have reduced (type II) or absent (type III) expression of GPI-anchored proteins. Type II PNH cells show slow, ongoing lysis to aerolysin over time because of their reduced but not absent GPI-anchors; nevertheless, even type II PNH cells can be unequivocally distinguished from normals and other disease states using the above-mentioned conditions (1 × 10−8 mol/L aerolysin for 10 minutes).
The sensitivity and specificity of the assay are not surprising given that no other clinical syndrome is characterized by cells with deficient GPI anchors. The assay represents an improvement over traditional screening tests for PNH that measure the sensitivity of erythrocytes to homologous complement, such as the sucrose hemolysis and Ham tests. The Ham test is relatively specific for PNH, but lacks sensitivity, whereas the sucrose hemolysis test is relatively sensitive, but is not specific.25 Another advantage of the aerolysin assay over these tests is that it accurately predicts the size of the PNH clone and the type of PNH erythrocytes (Figs 1 and 4) and can detect PNH populations in cells other than erythrocytes (Figs 3and 7).
Flow cytometry is currently the gold standard for diagnosing PNH but requires expensive equipment and significant technical expertise that are not available in many laboratories. The simple aerolysin assay offers most of the advantages of flow cytometry for the detection of PNH and can be performed in any laboratory with access to a plate reader or spectrophotometer. Moreover, it is currently not possible to detect small (<1% to 2%) PNH populations.24 25 However, by enriching for PNH cells, aerolysin can be used in conjunction with flow cytometry to detect PNH populations that represent 0.075% or less of the total cells (Figs 6 and 8). At this time it is unclear whether these small PNH populations are clinically relevent; nevertheless, this technology may be particularly helpful in studying the pathophysiology of PNH and detecting small PNH populations in patients with aplastic anemia (Fig 8).
Approximately one third of newly diagnosed PNH manifest as a secondary clonal complication in patients with aplastic anemia.31This is especially common after immunosuppressive therapy but is rare after regimens that use immunoablative doses of cyclophosphamide,32 with or without bone marrow transplantation.33 The close relationship between aplastic anemia and PNH suggests a pathophysiologic link between the two disorders, but the precise mechanism remains unclear.29,30,34,35 The fact that marrow failure in most cases of aplastic anemia results from an autoimmune attack has led some investigators to postulate that the immune attack in aplastic anemia is directed toward a GPI-anchored protein.36 37 Thus, PNH cells (with deficient GPI-anchored proteins) would be immune to attack and could preferentially expand. Nevertheless, direct evidence for such a mechanism in aplastic anemia or PNH is lacking and, with the exception of CD59 and CD55, GPI-anchored proteins are not ubiquitously expressed on both mature cells and progenitors. Our observations demonstrate that aerolysin is the first natural toxin that selectively kills normal cells while sparing PNH cells. This property may be particularly useful not only in diagnosis, but also in studying the biology of PNH by allowing the selection of PNH clones from the bone marrow in patients with aplastic anemia or other disease states.
ACKNOWLEDGMENT
The authors thank Dr Jerry Spivak for patient samples and critical reading of this manuscript and Marie C. Moineau for assistance in manuscript preparation. Drs Dana Devine and Brian Berry supplied samples from PNH patients that were used in preliminary experiments.
Supported in part by National Institutes of Health Grant No. CA74990 to R.A.B. and a grant from the Natural Sciences and Engineering Research Council of Canada (J.T.B.). R.A.B. is an American Society of Hematology Scholar.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Robert A. Brodsky, MD, Johns Hopkins Oncology Center, Room 2-127, 600 N Wolfe St, Baltimore, MD 21287-8967.



![Fig. 3. PNH cells lack proaerolysin binding proteins. Proaerolysin binding to proteins from LD− cells (lane 1), LD−(PIGA+) cells (lane 2), and CEM cells (lane 3). Equal numbers of cells (6 × 104/lane) were applied to each lane. Lane 1 ( LD− cells) is blank, whereas lane 2 [LD−(PIGA+)] has multiple bands. For the sake of comparison, an immature human T-cell line (CEM) was also run in this experiment. A band corresponding to Thy-1, which we have detected previously in mouse T cells, is easily visible in the figure.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/93/5/10.1182_blood.v93.5.1749/4/m_blod40509003w.jpeg?Expires=1765952002&Signature=uLtJMqfkkSPKrraE953dhB6erJ40XO-iYDFp45~jBSoeZLf3kBXfoNQ1RvBNKs9xT-Ev4qKDJ9AWqYduwaWIVa2Tj7tThKGGBY-7yNribsYAg0TDFKjmd09SXNYHnz2FSFN4IBLl4W7bC6ueNnpd-ewXM0k-4-H-qGrTVLULjMzhQLefRLK9KexVNEgdB910nftmi4AP~s4~595C1VVI2GxJWxXC3VMnFgaYaovhjQnzvtD6NTCeRKE2W7JhkmlvCFKkT13~d8hTDnfixv7PmpU3alaTlD9a3LpzcinW7x3AgNsPSDrEA-0QocLuhuAcNBykxONXZ-0qc2UJ2gQwVw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal