Abstract
Serum from 386 myeloma patients were analyzed for serum hyaluronan (HYA) at diagnosis. Median age was 68 years (range, 32 to 87 years). The distribution of Ig classes was typical (58% IgG, 21% IgA, 1% IgD, and 20% light chain disease). The patients comprised 58% in stage III, 33% in stage II, and 9% in stage I. The majority (82%) had HYA values within an intermediate range (10 to 120 μg/L), 13% had high values (>120 μg/L), and 5% had abnormally low values (0 to 9 μg/L). For the first time, a patient group with abnormally low HYA serum values is reported. An inverse correlation between survival and HYA serum level was found (P = .015). When tested separately, patients with abnormally low or high HYA values had significantly shorter median survival (21.1 and 19.7 months, respectively) than those with an intermediate HYA concentration (32.6 months; P = .005). Patients with abnormally low or high HYA levels had more advanced disease as judged by staging and biochemical markers. Interestingly, there was an inverse correlation between the HYA value and the M-component concentration in serum. Fifty percent of patients with abnormally low HYA values had IgA myelomas. In conclusion, the serum concentration of HYA may be of prognostic value in selected cases of multiple myeloma. Further studies will be performed to elucidate possible explanations for our findings, especially those related to the HYA cell surface binding proteins.
HYALURONAN (HYA) IS A high molecular weight polysaccharide that is mainly located extracellularly in all tissues. The concentration varies with the localization and state of the tissue investigated. The highest quantities are found in loose connective tissues such as the umbilical cord (4,100 mg/kg) and the synovial fluid (1,400 to 3,600 mg/L). High concentrations are also found in the vitreous body (140 to 340 mg/kg) and dermis (200 mg/kg). The biosynthesis of this large, linear chain molecule occurs in the plasma membrane of cells, which are regulated by different factors such as inflammatory mediators, hormones, and growth factors (for review see Fraser et al1). HYA production increases in proliferating cells, especially during mitosis. For several decades, it has been known that mesenchymal cells form a hyaluronidase-sensitive pericellular layer.2 Discoveries of specific cell surface receptors that can attach HYA to cells make it probable that HYA is an important regulator of cellular activities.3 Various HYA-receptors have been identified on different cell types, such as CD44 present on lymphocytes,4 and more recently described on myeloma cells (for review, see Cook et al5). Expression of the HYA-binding CD44-receptor and its specific splice variants have also been reported in many other malignancies and, in various ways, have been linked to their metastatic behavior.6-14
Since a method for detecting nanogram amounts of HYA was developed15,16 that uses the ability of this molecule to bind to proteoglycans, HYA has been detected in body fluids, such as lymph, serum, urine, and pleural fluid. Rough calculations indicate that one-third of all HYA in tissues (15 g in an average adult) is catabolized every day. The major part is catabolized by local uptake in cells and in lymph nodes. The remaining, regarded as normal spill-over, is carried to the blood by lymph in an amount of 20 to 40 mg/d and is rapidly taken up mainly by the liver endothelial cells viz. specific receptors. The half-life of circulating HYA in healthy adults is 2.5 to 5.5 minutes (see Fraser et al1 and references therein).
The serum HYA value is the steady-state level arising from supply and removal. Normal healthy middle-aged persons have been found to have serum HYA levels in the order of 10 to 100 μg/L, with an age-dependent continued increase from the level at 16 years of 29 ± 17 μg/L (mean ± standard deviation [SD]) to 177 ± 133 μg/L in elderly healthy persons over 75 years of age.17 In the age group of 61 to 70 years, ie, close to the mean age of the patients in the present study, the level was 112 ± 88 μg/L. Very high serum levels of HYA have been found in patients with liver disease (>700 μg/L), and high concentrations are correlated with histopathological diagnosis of cirrhosis. This is because of an impaired clearance from blood, manifested as a longer half-life in serum, a lower splanchnic extraction, and a lower maximal clearance capacity of the liver endothelial cells (see Laurent et al18 and references therein). High HYA levels are also seen in joint disease such as rheumatoid arthritis (mean values up to 297 μg/L), because of a large increase in total HYA in the joint fluid that is driven out by lymph into the circulation by physical activity. Serum HYA is found to correlate to the total joint involvement.19,20 In septic patients, high serum HYA is correlated with a bad prognosis.21 Probably, HYA synthesis is enhanced by tumor necrosis factor-α (TNF-α), and increased capillary permeability may lead to a wash-out of HYA from the interstitium. Patients with certain tumors are also found to have high values of HYA, first described in children with nephroblastoma (see Laurent et al18 and references therein). Extreme values have been reported in patients with progressive malignant mesothelioma (median value, 250 μg/L; range, 41 to 37, 880 μg/L).22 In these cases, the increased amount of HYA is probably produced locally due to stimulation by various growth factors.23 No medical condition with serum HYA levels less than 10 μg/L has been reported so far.
Multiple myeloma (MM) is a B-cell malignancy of unknown etiology with expansion of clonal malignant plasma cells. Clinically, this can result in the presence of monoclonal Igs in serum and/or urine, pancytopenia, renal dysfunction, hypercalcemia, and/or bone destruction. The purpose of this study was to examine serum HYA in a large, unselected group of patients with newly diagnosed MM and see if HYA could serve as a disease marker in this condition. Information about HYA is of special interest as myeloma cells express receptors for this polysaccharide.5
MATERIALS AND METHODS
Patients
A total of 583 patients were entered in the Nordic Myeloma Study Group (NMSG) randomized trial from June 1990 to November 1992. Patients with newly diagnosed MM were randomized to receive Melphalan-Prednisone or Melphalan-Prednisone-Interferon α2b. The diagnostic and eligibility criteria and results of treatment were described by Hjorth et al.24 Our study group consisted of 386 unselected patients from whom serum samples were drawn before randomization and start of therapy. The median age of the patients in the study group was 68.0 years (range, 32 to 87 years; mean age, 66.7 ± 9.0 SD). There were 228 males and 158 females. The distribution of myeloma characteristics were typical, with M-component type IgG in 58.3%, IgA in 21.2%, and IgD in 3 patients (0.8%). One patient (0.3%) had a nonsecreting myeloma. Seventy-six patients (19.7%) had light chain disease. According to the clinical staging system by Durie and Salmon,25 8.5% of the patients were in stage I, 33.2% in stage II, and 58.3% in stage III. Additional parameters measured were the percentage of plasma cells in bone marrow, hemoglobin, calcium, creatinine, serum albumin, and serum β2-microglobulin. After completion of the study, all sera were analyzed for interleukin-6 (IL-6), IL-6 receptor (IL-6sR), and C-reactive protein (CRP).
Methods
Serum analyses.
The serum samples were analyzed by a radiometric assay16based on the use of specific HYA binding proteins isolated from bovine cartilage. The HYA in the serum sample reacts with125I-labeled HYA binding proteins in solution. The unbound label is then quantitated by incubating with HYA covalently bound to Sepharose particles of small size and low density. Separation is performed by centrifugation, followed by decanting, and the radioactivity bound to the particles is counted in a gamma counter. The radioactivity is inversely related to the HYA concentration in the serum sample.
Because the majority of the samples with abnormally low HYA levels appeared to have high levels of Ig, the sera were stepwise diluted up to 10 times with normal serum to ensure that the very low HYA concentrations were not due to an assay artifact.
Statistical analyses.
The survival time was measured from the date of randomization to death or last follow-up. To estimate the association to survival, the HYA serum values were transformed to rank order and analyzed univariately by the Cox proportional hazard model. The survival curves for different groups of HYA serum values were constructed by the Kaplan-Meier method and compared by the log-rank test. The nonparametric Mann-Whitney-U test was used to compare patient characteristics between patients with abnormally low (<10 μg/L), intermediate (10 to 120 μg/L), and high (>120 μg/L) HYA serum levels. P values less than .05 were considered statistically significant. The analyses were performed on a Macintosh computer with the use of the statistical program StatView 4.5 (Abacus Concepts, Inc; Berkeley, CA). The NMSG study found no survival differences between the two arms of treatment; thus, it was possible to pool data from both treatment arms in the evaluation of prognostic significance for the parameters studied.
RESULTS
The median HYA value was 47 μg/L (range, 0 to 19,650 μg/L). The HYA values of 315 (82%) myeloma patients were within the intermediate range, whereas 51 (13%) had elevated values and 20 (5%) had abnormally low values.
HYA serum levels were not associated with survival when used as absolute values. However, after transformation to rank order, a significant inverse correlation to survival was found in a univariate analysis (P = .015). HYA was not a significant independent prognostic factor when tested in a multivariate analysis. HYA serum levels transformed to rank order were correlated to M-component concentration (r = −.245), age (r = .215), serum creatinine (r = .201), and serum β2-microglobulin (r = .146).
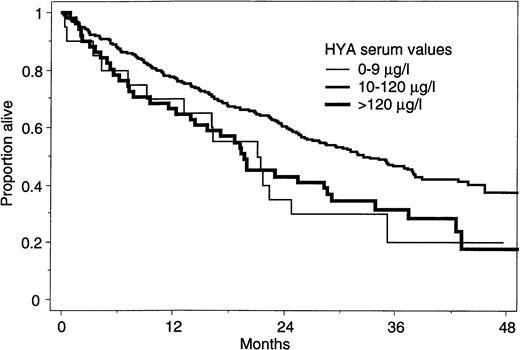
A more complex pattern was seen when the patients were grouped according to high, intermediate, or abnormally low HYA serum levels. Patients with either abnormally low or high serum HYA levels had significantly shorter survival (median survival, 21.1 and 19.7 months, respectively) than patients with serum HYA levels within the intermediate range (32.6 months; Fig 1). Table 1 displays the association between stages of disease, according to Durie and Salmon,25 and HYA levels. There were relatively more patients with advanced disease in the groups with abnormal low or high serum HYA levels. The Ig class of the M-component was also unevenly distributed, with a higher proportion of IgA myeloma cases in the group with abnormally low HYA levels and more Bence Jones myeloma cases among patients with high HYA levels.
Kaplan-Meier survival curves for 386 myeloma patients separated by low (0 to 9 μg/L, n = 20), intermediate (10 to 120 μg/L, n = 315), and high (>120 μg/L, n = 51) HYA value. The survival difference between the abnormally low or high and the intermediate HYA level group were significant (P = .005).
Kaplan-Meier survival curves for 386 myeloma patients separated by low (0 to 9 μg/L, n = 20), intermediate (10 to 120 μg/L, n = 315), and high (>120 μg/L, n = 51) HYA value. The survival difference between the abnormally low or high and the intermediate HYA level group were significant (P = .005).
Serum HYA Levels in Subgroups of Myeloma Patients
| . | N . | % . | Serum Hyaluronan Level . | Total % . | |||||
|---|---|---|---|---|---|---|---|---|---|
| 0-9 μg/L . | 10-120 μg/L . | >120 μg/L . | |||||||
| N . | % . | N . | % . | N . | % . | ||||
| Stage | |||||||||
| I | 34 | 9 | 0 | 0 | 32 | 94 | 2 | 6 | 100 |
| II | 130 | 34 | 6 | 5 | 106 | 82 | 18 | 14 | 100 |
| III | 222 | 57 | 14 | 6 | 177 | 80 | 31 | 14 | 100 |
| Total | 386 | 100 | |||||||
| M-comp Ig class* | |||||||||
| IgA | 82 | 21 | 10 | 12 | 67 | 82 | 5 | 6 | 100 |
| IgG | 224 | 59 | 9 | 4 | 186 | 83 | 29 | 13 | 100 |
| BJ† | 76 | 20 | 1 | 1 | 59 | 78 | 16 | 21 | 100 |
| Total | 382 | 100 | |||||||
| . | N . | % . | Serum Hyaluronan Level . | Total % . | |||||
|---|---|---|---|---|---|---|---|---|---|
| 0-9 μg/L . | 10-120 μg/L . | >120 μg/L . | |||||||
| N . | % . | N . | % . | N . | % . | ||||
| Stage | |||||||||
| I | 34 | 9 | 0 | 0 | 32 | 94 | 2 | 6 | 100 |
| II | 130 | 34 | 6 | 5 | 106 | 82 | 18 | 14 | 100 |
| III | 222 | 57 | 14 | 6 | 177 | 80 | 31 | 14 | 100 |
| Total | 386 | 100 | |||||||
| M-comp Ig class* | |||||||||
| IgA | 82 | 21 | 10 | 12 | 67 | 82 | 5 | 6 | 100 |
| IgG | 224 | 59 | 9 | 4 | 186 | 83 | 29 | 13 | 100 |
| BJ† | 76 | 20 | 1 | 1 | 59 | 78 | 16 | 21 | 100 |
| Total | 382 | 100 | |||||||
Number and percentage of myeloma patients in different disease stages (upper part) and with different M-component Ig classes (lower part) are given to the left. To the right individuals in the various stages (upper part) and with various M-component Ig classes (lower part) are separated according to abnormally low, intermediate, and high serum HYA levels.
Three cases with IgD and one nonsecretory case are excluded.
Bence Jones protein.
Patients in the group with abnormally low HYA levels had a higher percentage of bone marrow plasma cells, higher M-component concentration, and lower levels of hemoglobin and albumin when compared with patients with HYA levels in the intermediate range (Table 2). Patients in the group with high HYA levels had significantly lower hemoglobin levels and higher β2-microglobulin levels when compared with patients with HYA levels in the intermediate range. There was an inverse correlation between serum HYA level and M-component concentration most pronounced in the IgG myeloma (Fig 2). Serum levels of Ca, creatinine, IL-6, IL-6sR, and CRP did not differ significantly between the three HYA level groups. The age distribution was also similar (mean ± SD of 63.1 ± 12.7, 66.7 ± 8.7, and 67.7 ± 9.3 years in the abnormally low, intermediate, and high HYA level groups, respectively).
Laboratory Parameters and Serum HYA Levels in Myeloma Patients
| Parameters . | All Patients . | Serum Hyaluronan Level . | P* . | P† . | ||
|---|---|---|---|---|---|---|
| 0-9 μg/L . | 10-120 μg/L . | >120 μg/L . | ||||
| BM plasma cells (%) | 30.0 (0-100) | 48.5 (7-90) | 30.0 (0-100) | 30.0 (2-95) | .026 | .463 |
| Hemoglobin (g/L) | 106 (36-152) | 96 (71-144) | 108 (36-152) | 99 (68-138) | .002 | .004 |
| M-comp. conc. (g/L)‡ | 35 (0-121) | 56.5 (0-98) | 35.0 (0-121) | 26.5 (0-85) | .001 | .038 |
| IgG (g/L) (n = 224) | 64.0 (32-98) | 43.0 (1-121) | 38.0 (3-85) | .016 | .077 | |
| IgA (g/L) (n = 82) | 54.5 (16-68) | 34.0 (4-74) | 40.0 (9-55) | .009 | .499 | |
| β2-microglobulin (mg/L) | 4.8 (0.2-60.6) | 5.5 (2.3-39.3) | 4.4 (0.2-60.6) | 6.3 (1.7-48.0) | .503 | .005 |
| Albumin (g/L) | 34.0 (13-54) | 29.0 (23-45) | 35.0 (13-54) | 35.5 (16-46) | .025 | .710 |
| Parameters . | All Patients . | Serum Hyaluronan Level . | P* . | P† . | ||
|---|---|---|---|---|---|---|
| 0-9 μg/L . | 10-120 μg/L . | >120 μg/L . | ||||
| BM plasma cells (%) | 30.0 (0-100) | 48.5 (7-90) | 30.0 (0-100) | 30.0 (2-95) | .026 | .463 |
| Hemoglobin (g/L) | 106 (36-152) | 96 (71-144) | 108 (36-152) | 99 (68-138) | .002 | .004 |
| M-comp. conc. (g/L)‡ | 35 (0-121) | 56.5 (0-98) | 35.0 (0-121) | 26.5 (0-85) | .001 | .038 |
| IgG (g/L) (n = 224) | 64.0 (32-98) | 43.0 (1-121) | 38.0 (3-85) | .016 | .077 | |
| IgA (g/L) (n = 82) | 54.5 (16-68) | 34.0 (4-74) | 40.0 (9-55) | .009 | .499 | |
| β2-microglobulin (mg/L) | 4.8 (0.2-60.6) | 5.5 (2.3-39.3) | 4.4 (0.2-60.6) | 6.3 (1.7-48.0) | .503 | .005 |
| Albumin (g/L) | 34.0 (13-54) | 29.0 (23-45) | 35.0 (13-54) | 35.5 (16-46) | .025 | .710 |
Association between laboratory parameters and serum HYA levels in 386 patients with multiple myeloma. The HYA serum levels are grouped in abnormally low (0 to 9 μg/L; n = 20), intermediate (10 to 120 μg/L; n = 315), and high (>120 μg/L; n = 51) values.
Low versus intermediate HYA value group.
High versus intermediate HYA value group.
Seventy-two patients with light chain disease, 3 with IgD, and 1 nonsecretory patient are excluded.
Box plots of IgG (n = 224; upper panel) and IgA (n = 82; lower panel) concentrations in myeloma patients separated by low (0 to 9 μg/L; left), intermediate (10 to 120 μg/L; middle), and high (>120 μg/L; right) HYA serum values (number of patients in each group is given in Table 1). The horizontal lines in the plots represent the 10th, 25th, 50th, 75th, and 90th percentile, respectively. The differences between the abnormally low and intermediate HYA value groups were significant (P = .016 [IgG] and P = .009 [IgA], respectively).
Box plots of IgG (n = 224; upper panel) and IgA (n = 82; lower panel) concentrations in myeloma patients separated by low (0 to 9 μg/L; left), intermediate (10 to 120 μg/L; middle), and high (>120 μg/L; right) HYA serum values (number of patients in each group is given in Table 1). The horizontal lines in the plots represent the 10th, 25th, 50th, 75th, and 90th percentile, respectively. The differences between the abnormally low and intermediate HYA value groups were significant (P = .016 [IgG] and P = .009 [IgA], respectively).
DISCUSSION
Because our patient group has a median age of 68.0 years with a very wide range (32 to 87 years), it is not possible to give a normal HYA level range that includes all the patients. We find it therefore more correct to describe levels ranging from 10 to 120 μg/L as intermediate values. The main finding in this study is that, in a large well-defined population of myeloma patients, the HYA concentration in serum before start of treatment was within the intermediate range in the majority of patients. Only 13% of the patients had values above 120 μg/L, ie, a limit above which earlier studies have shown increased morbidity in middle aged patients.18,19 This is in accordance with our own observation in a small group of myeloma patients,26 but in contrast to the findings of Abildgaard et al,27 who found increased levels in serum of all 15 myeloma patients investigated. This emphasizes the importance of investigating large groups of patients when testing HYA as a suitable tumor marker.
An interesting observation in the present study is that a small group (n = 20 [5%]) of patients showed abnormally low serum HYA levels, which were previously not reported for any patient group. Experiments were performed to ensure that this was not due to an assay artifact, because Ig theoretically could interfere with the binding protein in the HYA assay.
When testing patients showing abnormally low, intermediate, and high serum HYA levels for clinical and laboratory parameters, it appeared that a majority with abnormally low or high HYA values were patients with advanced disease, as judged by staging (Table 1) or by measuring parameters such as hemoglobin, serum albumin, and Bence Jones protein (Table 2). It is emphasized that the patient age and CRP status were similar in the different HYA groups, because it is known that HYA levels increase with age17 and with infection.21 A connection between low HYA levels and disease activity has, to our knowledge, not been reported earlier. In addition, there turned out to be a strong inverse correlation between the levels of Ig and HYA in serum, in particular IgG. In correspondence with this finding, the patient group with abnormally low HYA had the highest number of abnormal plasma cells in the bone marrow. This negative correlation between Ig and HYA persisted when patients with IgG and IgA myeloma were investigated separately (Fig 2). Interestingly, we also found an increased number (50%) of IgA myeloma in the low HYA level group (Table 1).
Even if the majority of patients had HYA levels within the intermediate range, an inverse correlation between increasing serum HYA levels and survival was found. This is in accordance with several studies on patients with various diseases, malignant as well as nonmalignant.18,19 28 The finding of a connection between elevated serum HYA levels and β2-microglobulin, an accepted prognostic marker in MM, supports the significance of the finding of an inverse correlation between increasing serum HYA and survival. However, the association of HYA levels to survival is more complex, because it was observed that patients with abnormally low levels also have a poor prognosis (Fig 1). It may be argued that the finding of a bad prognosis in patients with abnormal levels is to be expected, because abnormal serum levels of any biologically important component of blood may be correlated to bad outcome by different mechanisms. However, we have no indication to believe that it is the abnormal HYA value that induces a shorter survival. We suggest that the abnormal HYA serum level is mirroring serious pathological mechanisms within the malignant myeloma clones.
It is known that the survival of cancer cells depends on their ability to adhere to the tissue matrix, to proliferate, to migrate, to invade the tissue, and to form metastases. It has also been proposed that HYA is involved in all these steps. The presence of HYA binding adhesion molecules, especially CD44 and receptor for hyaluronic acid-mediated motility (RHAMM), is under intensive investigation at present. The binding of HYA to these cell receptors is claimed to be of great importance for cell-cell and cell-matrix interaction and thereby for cell migration and metastatic expansion of malignant cells.3,12,14,29 Concerning MM, it is known that neoplastic myeloma cells differ from normal plasma cells and other B-cell malignancies by an almost exclusive homing to the bone marrow microenvironment. Cook et al5 claim that cellular adhesion molecules such as the HYA-binding CD44 receptor are involved in this homing and that some of these adhesion molecules potentiate proliferation rather than Ig production. This mechanism could be one among several possible reasons for this inverse association between serum values of Ig and HYA in our patients. One explanation for the abnormally low HYA values in the circulation in some myeloma patients is the occurrence of an excess of unoccupied HYA binding receptors on myeloma cells in the bone marrow that can bind circulating HYA produced in other tissues. This may result in an even shorter half-life of circulating HYA than otherwise found in normal subjects.1Furthermore, the occurrence of adhesion molecules has been more frequently found in the bone marrow of patients with active multiple myeloma compared with patients with inactive disease.30Recently Masellis-Smith et al31 32 have shown the importance of subsets of B cells or leukemic plasma cells in blood for the HYA-dependent spread of malignant myeloma cells in patients with MM.
Concerning patient survival and CD44 expression, an important observation was made by Kaufmann et al,33 who demonstrated an association between the expression of CD44 variant exon epitopes in primary breast cancer and length of survival. The presence of these CD44 epitopes absent in nonmalignant tissue controls was correlated with poor overall survival. Furthermore, patients with CD44 splice variant positive ovarian carcinomas had a significantly shorter disease-free survival than patients with CD44 splice variant negative tumors.34
To our knowledge, no work has been performed to elucidate the correlation between HYA serum level and expression of HYA binding cell receptors in vivo. However, by testing melanoma cell lines, those with high metastatic potential did show an increased migration rate on an HYA-rich matrix in addition to a significant increased number of the HYA binding CD44 epitopes.35 Production of HYA as well as the CD44 receptor was increased in those cell lines, indicating an autocrine mechanism that could eventually result in an elevated serum level of HYA. In line with these speculations, high HYA serum levels in some of the current myeloma patients may indicate an increased HYA production by the myeloma cells and increased growth of the cells in the marrow, resulting in spill-over of HYA to the circulation. High HYA serum level could alternatively originate from other adjacent cells under influence of growth factors, as in mesothelioma cell lines.23 Why abnormally low HYA levels are inversely associated to survival could be explained correspondingly. The low HYA levels in these patients may be due to absence of autocrine mechanisms for HYA production combined with a strong binding of circulating HYA to internalizing HYA receptors on the myeloma cells. This adds to the receptor-mediated clearance of circulating HYA by the liver endothelial cells, as previously discussed.
In conclusion, the measurement of serum HYA levels alone in myeloma patients is unlikely to give significant prognostic information, because the majority of our patients had values within an intermediate range. However, our findings may have impact regarding myeloma pathophysiology. At present, we are investigating, in addition to HYA serum level, HYA binding adhesion molecules on myeloma cells from patients with various forms of MM. By combining these different parameters, we hope to find new ways to characterize this complex disease and to elucidate its biological aspects.
Supported by the Norwegian Cancer Society, Oslo, Norway.
Members of the directory board of the Nordic Myeloma Study Group in alphabetical order: I.M.S. Dahl, P. Gimsing, E. Hippe, M. Hjorth, E. Holmberg, J. Lamvik, E. Löfvenberg, S. Magnusson, J.L. Nielsen, I. Palva, S. Rödjer, I. Talstad, I. Turesson, J. Westin, and F. Wisløff.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Inger Marie S. Dahl, Section of Hematology, University Hospital, 9038 Tromsø, Norway.

![Fig. 2. Box plots of IgG (n = 224; upper panel) and IgA (n = 82; lower panel) concentrations in myeloma patients separated by low (0 to 9 μg/L; left), intermediate (10 to 120 μg/L; middle), and high (>120 μg/L; right) HYA serum values (number of patients in each group is given in Table 1). The horizontal lines in the plots represent the 10th, 25th, 50th, 75th, and 90th percentile, respectively. The differences between the abnormally low and intermediate HYA value groups were significant (P = .016 [IgG] and P = .009 [IgA], respectively).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/93/12/10.1182_blood.v93.12.4144/4/m_blod412360021x.jpeg?Expires=1769174364&Signature=ouuYV6ZOqbz~Sz3CoFoxMNgYj9MIMoe5khKcYXt0kgJfD-h2BTvvquGaqLIsgL-S1yZ492OeKKH3PpeCT1qEKRVWl2O729ToEl1Lz4fWfvF4UwbrOaS2cf263Df44c6KGjIzW7Y~a06Zl0UYeDHaB6EQMrYvaFHEvQRAouLf90-CyQmFbB3VIohHupZGOmywnSEX2XLM5PVxl~ltPrMLKYgDp4DJIOjWSCgBZ5ihNX9VOD8mw~l0DXncVKBiLSP0Zkt6ycrsM7H63h7611oLqZW0Mj-oVeB~sSYmvDZEPl-~N3nXC4fddDduZbbV95LjaUgT~NsmikR1~UsNZuMFGw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 2. Box plots of IgG (n = 224; upper panel) and IgA (n = 82; lower panel) concentrations in myeloma patients separated by low (0 to 9 μg/L; left), intermediate (10 to 120 μg/L; middle), and high (>120 μg/L; right) HYA serum values (number of patients in each group is given in Table 1). The horizontal lines in the plots represent the 10th, 25th, 50th, 75th, and 90th percentile, respectively. The differences between the abnormally low and intermediate HYA value groups were significant (P = .016 [IgG] and P = .009 [IgA], respectively).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/93/12/10.1182_blood.v93.12.4144/4/m_blod412360022x.jpeg?Expires=1769174364&Signature=St-Bnr824arIXidPJmJClK2V4CC66fuSBd9t2Z4Nwv8bgKP4ZlN3cXFz4nr6ax5F5SWxZATmtnh4OwziSnXldQnAoFt6u8FP4MSJ6WCfWX-I4IS18WiWk8UFbc5K28KEQn5iILpMdynmKjXtdMPODB3x0zdjWZpzLf~mRGSWaTMngJpXUGI4Lg~zgdnOJsCoPWheP-paUax6CR0mRUcfEbik8rNr~Eih9nvLn-mXxEI29JQuzsjq1QFCQQgjz2x4vPA7HINYZFCqXNYv21u~Ba~ebnlT4RCVMQK-5imY05dhSwHvmpwCDW-jxtwOyUJMOvpSLbRy~JJEDJ6Jd968mw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal