Abstract
We performed a prospective, randomized, multicenter trial to evaluate the effectiveness of prophylactic inhalations with aerosolized amphotericin B (aeroAmB) to reduce the incidence of invasive aspergillus (IA) infections in patients after chemotherapy or autologous bone marrow transplantation and an expected duration of neutropenia of at least 10 days. From March 1993 until April 1996, 382 patients with leukemias, relapsed high-grade non-Hodgkin lymphomas, or solid tumors were randomized with a 13:10 ratio to receive either prophylactic aeroAmB inhalations at a dose of 10 mg twice daily or no inhalation prophylaxis in an unblinded fashion. The incidence of proven, probable, or possible IA infections was 10 of 227 (4%) in patients who received prophylactic aeroAmB. This did not differ significantly from the 11 of 155 (7%) incidence in patients who received no inhalation prophylaxis (P = .37). Moreover, no differences in the overall mortality (13% v 10%; P= .37) or in the infection-related mortality (8% v 7%;P = .79) were found. In contrast to other nonrandomized trials, we observed no benefit from prophylactic aeroAmB inhalations, but the overall incidence of IA infections was low.
INVASIVE ASPERGILLUS (IA) infections have become an increasingly frequent and serious complication from prolonged neutropenia after chemotherapy or bone marrow transplantation (BMT).1-3 Yet, the incidence of IA infections in this setting is highly variable, ranging from as low as 0% to as high as 25% or more, depending on the epidemiologic exposure to aspergilli, the duration of neutropenia, and other individual risk factors.1,2,4,5 Difficulties in establishing an early clinical diagnosis, the poor response to antifungal treatment, and the resulting high morbidity and mortality from IA infections prompted widespread efforts to develop preventive strategies.6 7
Because IA infections are usually acquired by inhalation of aspergillus conidia and because the lungs are the primary site of infection in the majority of patients, we investigated aerosolized amphotericin B (aeroAmB) as prophylaxis of IA infections in a prospective randomized multicenter trial in patients with hematologic malignancies or solid tumors and an expected duration of neutropenia of at least 10 days.
PATIENTS AND METHODS
Study design.
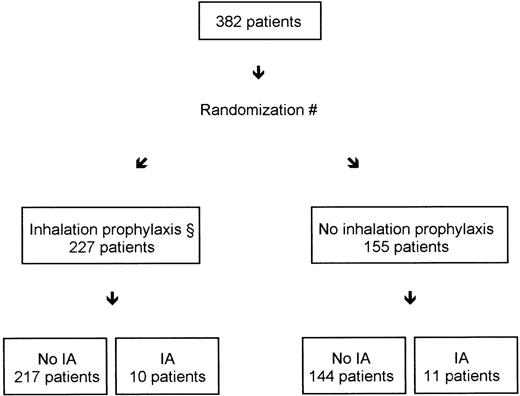
Between March 1993 and April 1996, 382 patients were entered in a prospective randomized multicenter trial at 11 participating centers throughout Germany. Patients were randomized into two arms of the trial to receive either prophylactic inhalations with aeroAmB (group A) or no inhalation prophylaxis (group B) in an unblinded fashion (Fig 1). Results from a preliminary interim analysis that would have allowed us to stop the trial early have already been reported.8 However, because none of the predefined stopping rules was fulfilled in the initial 115 patients, the trial continued to recruit to its full calculated sample size. The study was approved by local ethics committees at each participating center and conducted according to the guidelines established by the Declaration of Helsinki. Eligibility criteria were as follows: (1) patients scheduled to receive intensive chemotherapy with an expected duration of neutropenia less than 0.5/nL for at least 10 days because of either de novo or relapsed acute myeloid leukemia (AML), high-risk myelodysplasia (MDS), chronic myeloid leukemia (CML) in blast crisis, high-risk de novo or relapsed acute lymphocytic leukemia (ALL), or relapsed high-grade non-Hodgkin’s lymphoma (NHL), or patients with solid tumors undergoing high-dose chemotherapy with autologous BMT (auto-BMT); (2) age greater than 18 years; (3) a Karnofsky index greater than 50%; and (4) written informed consent. Patients were excluded from the trial if one or more of the following criteria was fulfilled: (1) patients with a history of a proven, probable, or possible invasive aspergillus infection during any preceding neutropenic episode; (2) treatment with intravenous amphotericin B (AmB) or oral itraconazol during the previous 3 months; (3) concurrent or planned prophylaxis with intravenous AmB or itraconazol; (4) pulmonary infiltrates at the time of randomization; or (5) prior participation in the trial. All patients were required to be nursed in rooms without high-particulate air filtration.
(#) Randomization was stratified according to treatment center and three disease categories. (§) Inhalation prophylaxis was scheduled to begin before the onset of neutropenia at a dose of 2 × 10 mg aerosol AmB daily until one of four observation endpoints was reached: (1) recovery of neutropenia to greater than 1.0/nL for more than 2 consecutive days; (2) day +50 after randomization in patients without recovery of the neutrophil count to greater than 1.0/nL; (3) stable neutrophil counts for at least 1 week in patients without neutropenia less than 0.5/nL; or (4) death during the trial period. IA = proven, probable, or possible IA.
(#) Randomization was stratified according to treatment center and three disease categories. (§) Inhalation prophylaxis was scheduled to begin before the onset of neutropenia at a dose of 2 × 10 mg aerosol AmB daily until one of four observation endpoints was reached: (1) recovery of neutropenia to greater than 1.0/nL for more than 2 consecutive days; (2) day +50 after randomization in patients without recovery of the neutrophil count to greater than 1.0/nL; (3) stable neutrophil counts for at least 1 week in patients without neutropenia less than 0.5/nL; or (4) death during the trial period. IA = proven, probable, or possible IA.
Randomization was performed by computer-generated random numbers in sealed envelopes and permuted blocks of 10 in a 13:10 ratio in favor of group A, because we anticipated approximately 30% premature discontinuations of the prophylactic inhalations.9Envelopes were opened for each consecutive patient either at the coordinating center or at one of the participating centers after checking all of the inclusion and exclusion criteria. Randomization was stratified according to treatment center and the following three groups: (1) AML, high-risk MDS, and CML blast crisis; (2) high-risk de novo or relapsed ALL and relapsed NHL; and (3) solid tumors undergoing auto-BMT. Randomization was scheduled to be performed immediately before the initiation of antineoplastic chemotherapy, ie, before the onset of neutropenia less than 0.5/nL. However, patients who were neutropenic at the time of initiation of chemotherapy could also be randomized. Each patient entered the trial only once for a single neutropenic episode.
The trial period started with the random assignment of patients into one of the two arms of the trial and ended with one of the four predefined trial endpoints, whichever occurred first: (1) recovery of the neutrophil count to greater than 1.0/nL for more than 2 consecutive days; (2) day +50 after randomization in patients without recovery of the neutrophil count to greater than 1.0/nL; (3) stable neutrophil counts for at least 1 week in patients without neutropenia less than 0.5/nL; or (4) death during the trial period. All surviving patients were observed for at least 2 more weeks after one of the trial endpoints was reached.
The primary outcome variable was the cumulative incidence of proven, probable, or possible invasive aspergillus infections in each trial arm. Secondary outcome variables were incidence of fever refractory to antibiotic treatment, frequency and cumulative doses of intravenous AmB, overall and infection-related mortality in each trial arm, side effects of the prophylactic inhalations with aeroAmB as well as frequency, and causes of premature discontinuation of the allocated treatments. Overall incidence, type, and localization of all fungal and bacterial infections were also documented. To assure the quality of the data collection, charts and radiologic films of all patients were reviewed by one of the three principal investigators (J.B., S.S., or G.B.). In reviewing the source data, defining the trial endpoints, and analyzing the trial results, identical criteria were applied for all patients. No particular attention was given as to the randomization status of an individual patient. However, no formal attempt was made to blind for this information.
Interventions and treatments.
Overall, 227 patients were randomly assigned to group A and scheduled to receive prophylactic inhalations with aeroAmB at a dose of 10 mg AmB twice daily, starting with the day of randomization until one of the study endpoints was reached. Further continuation with prophylactic aeroAmB was optional in patients of group A when intravenous AmB treatment was started. For each inhalation, 10 mg of AmB for intravenous use (Bristol Myers Squibb, Munich, Germany) was diluted with sterile water to a total volume of 5 mL. Only three devices were allowed for nebulizing AmB: RespirGard II (Marquest, Englewood, CO) and PariBoy or Pari IS II (both Pari Werke, Starnberg, Germany). All three devices had been previously shown to generate particles that would allow alveolar as well as tracheal and nasopharyngeal deposition of AmB.10 The RespirGard II nebulizer was driven either by a bedside compressor (Lifetec jetair 10; Salvia, Schwalbach, Germany) or by pressured oxygen from hospital supplies with a pressure of at least 2 × 105 Pa. PariBoy and Pari IS II nebulizers were driven by their corresponding compressors, which were provided by the manufacturer (Pari Werke). Each inhalation lasted for about 15 to 20 minutes and each nebulizer was only used twice to avoid bacterial contamination. The 155 patients of group B were scheduled to receive no inhalation prophylaxis.
Definitions.
Proven invasive aspergillosis was defined as histologic evidence of invasive aspergillus infection with or without cultural evidence of the invading pathogen. Probable invasive aspergillosis was defined as pneumonia or any other organ infection unresponsive to antibiotic treatment with no other microbiologically documented causative organism and at least one of the following criteria: (1) aspergillus cultured from normally sterile tissues, bronchoalveolar lavage, blood, sputum, or nose; (2) repeated positive serological testing; or (3) pulmonary lesion with a halo sign in computed tomography (CT) scans or an air crescent sign. Possible invasive aspergillosis was defined as fever unresponsive to antibiotic treatment with no other microbiologically documented causative organism and at least one of the following criteria: (1) aspergillus cultured of normally sterile tissues, bronchoalveolar lavage, blood, sputum, or nose; or (2) repeated positive serological testing. Serological testing was performed using the commercially available Pastorex latex agglutination test (Sanofi Diagnostics Pasteur, Marnes-La-Coquette, France) for detection of aspergillus galactomannan.11 Serological testing would have also been considered positive in patients with increasing antibody titers in at least two consecutive serum samples.
Infections were otherwise classified in either bacteremia/fungemia, other microbiologically documented infections, clinically documented infections, fever of unknown origin, and no evidence of infection.12 Pneumonia was diagnosed clinically in any febrile patient by typical auscultation findings or radiologic infiltrates on chest x-rays or CT scans. Infiltrates were classified as interstitial or focal, and only focal lesions with an air crescent sign or a halo sign were considered to be suggestive of IA infections.
Fever was defined as a single oral temperature of greater than 38.5°C or two consecutive oral temperatures of greater than 38°C. Fever refractory to antibiotic treatment was defined as persisting fever despite broad spectrum intravenous antibiotics for more than 5 days, which included a nonresponse to at least one modification of the initial antibacterial regimen.
Supportive care.
All patients were hospitalized and reverse isolation measures were instituted during periods of neutropenia less than 0.5/nL. Antibacterial prophylaxis was performed at the discretion of each participating center. If performed, antibacterial prophylaxis consisted of oral cotrimoxazole or a quinolone. Patients were allowed to receive prophylactic oral amphotericin B, fluconazole, or both as prophylaxis of candida infections, because no influence of these drugs on the incidence of IA infections was anticipated. However, with the intravenous administration of AmB, prophylactic fluconazole was stopped. Antiviral prophylaxis with acyclovir was allowed, but was not routinely administered.
Empiric antibiotic treatment was initiated in febrile patients according to published guidelines.13 A broad spectrum penicillin or a third-generation cephalosporin in combination with an aminoglycoside was used as initial treatment. Alternatively, a combination of two broad spectrum β-lactam drugs or single-agent carbapenem was also allowed. In patients who remained febrile after 3 days, a glycopeptide drug was added. The empiric antibiotic treatment was modified according to clinical or microbiological findings. After a minimum of 5 days with fever unresponsive to antibiotic treatment, empiric intravenous AmB was initiated at a minimum dose of 0.5 mg/kg and continued at least until neutrophil recovery. Because of an anticipated high incidence of fungal infections, empiric intravenous AmB was also started in patients with clinical or radiological evidence of pneumonia.14
Diagnostic procedures included daily clinical evaluations as well as conventional chest x-rays of the lungs, blood cultures, and serologic testing for fungal pathogens at the time when fever first developed. In patients with pulmonary infiltrates on conventional films, CT scans of the thorax were recommended, preferably using the high-resolution technique. In these patients, x-rays of the sinuses, microbiologic examination of sputum, and serologic testing for fungal pathogens were also indicated. Bronchoalveolar lavage was performed if it was considered safe for an individual patient by the local investigator. Other diagnostic procedures were performed as clinically indicated. Surveillance with weekly chest x-rays and microbiologic examination of sputum and swabs from the nose and pharynx were recommended.
Statistical methods.
The analysis of the trial was planned and performed on an intention-to-treat basis. Therefore, all patients were analyzed in the trial arm to which they were initially randomized, regardless of whether they received the allocated prophylaxis or discontinued the allocated prophylaxis prematurely and irrespective of the trial endpoint that was reached. The primary outcome variable on which the sample size calculation was based was the cumulative incidence of proven, probable, or possible IA infections in each arm of the trial. Based on the results of the pilot study for this trial, a cumulative incidence of 1% was anticipated in group A with prophylactic inhalations; in group B, without the prophylactic inhalations, a cumulative incidence of 10% was anticipated, for an overall difference of 9% between the two arms.9 With these figures and an α-error of 5% and a β-error of 10%, the minimal sample size was calculated to be at least 165 patients per arm. Because a rate of 30% premature discontinuations of prophylactic aeroAmB was expected from the pilot study, 50 additional patients were randomized to group A for an overall sample size of 380 patients and a ratio of 13:10 (215 patients in group A with prophylactic inhalations and 165 patients in group B without prophylactic inhalations).9 To detect unexpected side effects of the prophylactic inhalations and to stop the trial early in case of unequivocal efficacy of aeroAmB, one interim analysis was performed after one third of patients in each arm were recruited.
Data were analyzed using the Prism (GraphPad, San Diego, CA) statistical software. The χ2 test was used for differences in categorical variables with the Yates correction whenever applicable. For continuous variables, the Student’s t-test or the Mann-Whitney U-test was used. Time-dependent variables were compared using the log-rank test on Kaplan-Meier estimates. All differences between the trial arms were tested two-sided and considered significant if their probabilities were less than 1% in the interim analysis and less than 4% in the final analysis for an overall two-sided significance level of P < .05.
RESULTS
Patient characteristics and study endpoints.
Figure 1 summarizes the trial design. Details of the patient characteristics are shown in Table 1. With the stratified randomization, the disease entities and consequently the duration of neutropenia were well balanced between the two groups (Fig 2). More than 70% of the study population were patients with de novo or relapsed AML, because we stopped recruiting auto-BMT patients with the increasing use of peripheral blood stem cells and the resulting shorter periods of neutropenia. Other potential confounding factors for the development of IA infections, such as age, steroid comedication, and building reconstruction activity in vicinity to study patients, were also equally distributed. However, hematopoietic growth factors were used more frequently in group A with prophylactic aeroAmB inhalations as compared with group B.
Patient Characteristics, Distribution of Known Risk Factors, and Endpoints of the Study
| . | Group A With Inhalations (n = 227) . | Group B Without Inhalations (n = 155) . |
|---|---|---|
| Age in years | ||
| Mean (range) | 46 (16-80) | 48 (17-81) |
| Disease category | ||
| AML/MDS/CML | 165 (73%) | 118 (76%) |
| ALL/NHL | 23 (10%) | 12 (8%) |
| Auto-BMT | 39 (17%) | 25 (16%) |
| Inadequate inclusions | 8 (4%) | 6 (4%) |
| Risk factors for IA infections | ||
| Neutropenia <0.5/nL at study entry | 79 (35%) | 48 (31%) |
| Building reconstruction activity | 49 (22%) | 36 (23%) |
| Steroid comedication | 29 (13%) | 20 (13%) |
| Growth factor (G-CSF/GM-CSF)* | 108 (48%) | 54 (35%) |
| Neutropenia <0.5/nL | ||
| Median (range) | 19 (0-50) | 21 (0-50) |
| Days in study | ||
| Median (range) | 27 (2-50) | 28 (0-50) |
| Study endpoint reached | ||
| Neutrophil recovery >1.0/nL | 171 (75%) | 120 (77%) |
| No neutrophils until day +50 | 28 (12%) | 18 (12%) |
| No neutropenia | 4 (2%) | 5 (3%) |
| Death before neutrophil recovery | 24 (11%) | 12 (8%) |
| . | Group A With Inhalations (n = 227) . | Group B Without Inhalations (n = 155) . |
|---|---|---|
| Age in years | ||
| Mean (range) | 46 (16-80) | 48 (17-81) |
| Disease category | ||
| AML/MDS/CML | 165 (73%) | 118 (76%) |
| ALL/NHL | 23 (10%) | 12 (8%) |
| Auto-BMT | 39 (17%) | 25 (16%) |
| Inadequate inclusions | 8 (4%) | 6 (4%) |
| Risk factors for IA infections | ||
| Neutropenia <0.5/nL at study entry | 79 (35%) | 48 (31%) |
| Building reconstruction activity | 49 (22%) | 36 (23%) |
| Steroid comedication | 29 (13%) | 20 (13%) |
| Growth factor (G-CSF/GM-CSF)* | 108 (48%) | 54 (35%) |
| Neutropenia <0.5/nL | ||
| Median (range) | 19 (0-50) | 21 (0-50) |
| Days in study | ||
| Median (range) | 27 (2-50) | 28 (0-50) |
| Study endpoint reached | ||
| Neutrophil recovery >1.0/nL | 171 (75%) | 120 (77%) |
| No neutrophils until day +50 | 28 (12%) | 18 (12%) |
| No neutropenia | 4 (2%) | 5 (3%) |
| Death before neutrophil recovery | 24 (11%) | 12 (8%) |
Probability of P < .05 for the difference between the two groups; all other comparisons between the two groups had probabilities of P > .05.
Distribution of the duration of neutropenia in patients of group A with prophylactic inhalations (○) and group B without prophylactic inhalations (•). For patients with proven, probable, or possible IA, the number of neutropenic days until an IA infection was suspected or proven are marked with squares ([□] in group A and [▪] in group B).
Distribution of the duration of neutropenia in patients of group A with prophylactic inhalations (○) and group B without prophylactic inhalations (•). For patients with proven, probable, or possible IA, the number of neutropenic days until an IA infection was suspected or proven are marked with squares ([□] in group A and [▪] in group B).
No differences in the study endpoints were found between group A and group B. Although a minority of patients in each group did not become neutropenic, the majority of patients in both groups developed significant neutropenia at a median of 19 days in group A and 21 days in group B (P = .84; Fig 2). About 12% of the patients in each group did not even recover with their neutrophil count until the maximal study period of 50 days after randomization (Table 1). There were 4% inadequate inclusions in each group, ie, disease entities not covered by the inclusion criteria (n = 6), chemotherapy regimens used without an expected neutropenia less than 0.5/nL (n = 7), and a pulmonary infiltrate at randomization (n = 1). However, because all of these patients were randomized, they were included in the final analysis of the trial.
Primary and secondary outcome variables.
The overall incidence of proven, probable, or possible IA infections was 21 of 382 (5%). There was no statistical difference in the cumulative incidences of proven, probable, and possible IA infections between the two trial arms. The incidence of IA infections was 10 of 227 (4%) in group A in patients with prophylactic inhalations and 11 of 155 (7%) in group B in patients without prophylactic inhalations (P = .37; Table 2). Repeated positive aspergillus antigen testing contributed to the diagnosis of an IA in 2 patients (UPN 79 and UPN 305) who were classified as having possible infections. Among 71 patients of group A who discontinued the inhalation prophylaxis prematurely, 5 of 71 (7%) developed a proven (n = 3) or probable (n = 2) IA infection. Three patients of group B started aeroAmB inhalations in violation of their randomized assignment. Thus, when the analysis was limited to patients who continued with their allocated treatments throughout the trial, 5 of 156 (3%) patients of group A and 10 of 152 (7%) patients of group B developed a proven, probable, or possible IA infection (P = .27). Details of all 21 patients who developed a proven, probable, or possible IA infection are shown in Table 3.
Incidence of Proven, Probable, or Possible IA Infections
| . | Patients of Group A With Inhalations (n = 227) . | Patients of Group B Without Inhalations (n = 155) . | All Patients (n = 382) . |
|---|---|---|---|
| IA infections | |||
| Proven | 4 | 1 | 5 |
| Probable | 5 | 9 | 14 |
| Possible | 1 | 1 | 2 |
| All IA infections | 10 (4%) | 11 (7%) | 21 (5%) |
| . | Patients of Group A With Inhalations (n = 227) . | Patients of Group B Without Inhalations (n = 155) . | All Patients (n = 382) . |
|---|---|---|---|
| IA infections | |||
| Proven | 4 | 1 | 5 |
| Probable | 5 | 9 | 14 |
| Possible | 1 | 1 | 2 |
| All IA infections | 10 (4%) | 11 (7%) | 21 (5%) |
Values are the number of patients, with percentages in parentheses. Comparisons between the two groups were not statistically significant.
Clinical Details in Patients With Possible, Probable, or Proven IA Infections
| UPN . | Strat. . | Inhal. . | Stop (d) . | Diagn. (d) . | Neutr. (d) . | Locat. of IA . | CXR Results . | CT Scan Results . | Sero. Results . | Histo. Results . | Culture Results . | Diagnosis Based on . | Category of IA . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3 | ALL3-150 | No | — | 15 | 6 | Trachea/lung | Normal | ND | ND | Pos. | ND | p.m. finding | Proven |
| 7 | AML | No | — | 23 | 16 | Lung | IPA | IPA | ND | ND | Neg. | Radiology | Probable |
| 12 | AML | No | — | 43 | 22 | Lung | IPA | IPA | Neg. | ND | Neg. | Radiology | Probable |
| 50 | AML | No | — | 34 | 29 | Lung | IPA | IPA | ND | ND | Neg. | Radiology | Probable |
| 117 | AML | No | — | 28 | >28 | Palate | Sinusitis | Sinusitis | Neg. | Neg. | A. flavus | Nasal swab | Probable |
| 123 | AML | No | — | 15 | >15 | Lung | IPA | IPA | ND | ND | ND | Radiology | Probable |
| 216 | AML3-150 | No | 53-151 | 15 | 11 | Lung | IPA | ND | Pos. | ND | A. fumig. | Surg. swab | Probable |
| 266 | AML | No | — | 13 | >13 | Lung | IPA | IPA | Pos. | ND | A. fumig. | BAL | Probable |
| 308 | AML | No | — | 40 | 38 | Lung | IPA | ND | ND | ND | A. fumig. | Sputum | Probable |
| 378 | AML | No | — | 32 | 11 | Lung | IPA | IPA | Neg. | ND | ND | Radiology | Probable |
| 79 | BMT | No | — | 14 | 4 | Sinus | Sinusitis | ND | Pos. | ND | ND | Serology | Possible |
| 49 | AML3-150 | Yes | — | 37 | >37 | Dissemin. | IPA | IPA | Neg. | Pos. | A. flavus | p.m. finding | Proven |
| 170 | BMT3-152 | Yes | 8 | 16 | 9 | Lung | Normal | ND | Pos. | Pos. | ND | p.m. finding | Proven |
| 192 | ALL | Yes | 8 | 23 | 15 | Lung/brain | IPA | IPA | Neg. | Pos. | Neg. | BAL + biopsy | Proven |
| 258 | AML3-150 | Yes | 1 | 30 | 26 | Lung | IPA | IPA | Pos. | Pos. | A. fumig. | BAL + biopsy | Proven |
| 51 | AML | Yes | — | 42 | 39 | Lung | IPA | IPA | ND | ND | ND | Radiology | Probable |
| 102 | BMT | Yes | 6 | 17 | 11 | Lung | IPA | IPA | Pos. | ND | ND | Radiology | Probable |
| 128 | AML3-150 | Yes | — | 11 | 3 | Lung | IPA | ND | Pos. | ND | Neg. | Radiology | Probable |
| 241 | AML | Yes | 8 | 13 | >13 | Lung | IPA | IPA | Neg. | ND | Neg. | Radiology | Probable |
| 360 | AML | Yes | — | 46 | >46 | Lung | IPA | IPA | Neg. | Neg. | Neg. | Radiology | Probable |
| 305 | BMT | Yes | — | 10 | 5 | Undeterm. | Normal | Normal | Pos. | ND | ND | Serology | Possible |
| UPN . | Strat. . | Inhal. . | Stop (d) . | Diagn. (d) . | Neutr. (d) . | Locat. of IA . | CXR Results . | CT Scan Results . | Sero. Results . | Histo. Results . | Culture Results . | Diagnosis Based on . | Category of IA . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3 | ALL3-150 | No | — | 15 | 6 | Trachea/lung | Normal | ND | ND | Pos. | ND | p.m. finding | Proven |
| 7 | AML | No | — | 23 | 16 | Lung | IPA | IPA | ND | ND | Neg. | Radiology | Probable |
| 12 | AML | No | — | 43 | 22 | Lung | IPA | IPA | Neg. | ND | Neg. | Radiology | Probable |
| 50 | AML | No | — | 34 | 29 | Lung | IPA | IPA | ND | ND | Neg. | Radiology | Probable |
| 117 | AML | No | — | 28 | >28 | Palate | Sinusitis | Sinusitis | Neg. | Neg. | A. flavus | Nasal swab | Probable |
| 123 | AML | No | — | 15 | >15 | Lung | IPA | IPA | ND | ND | ND | Radiology | Probable |
| 216 | AML3-150 | No | 53-151 | 15 | 11 | Lung | IPA | ND | Pos. | ND | A. fumig. | Surg. swab | Probable |
| 266 | AML | No | — | 13 | >13 | Lung | IPA | IPA | Pos. | ND | A. fumig. | BAL | Probable |
| 308 | AML | No | — | 40 | 38 | Lung | IPA | ND | ND | ND | A. fumig. | Sputum | Probable |
| 378 | AML | No | — | 32 | 11 | Lung | IPA | IPA | Neg. | ND | ND | Radiology | Probable |
| 79 | BMT | No | — | 14 | 4 | Sinus | Sinusitis | ND | Pos. | ND | ND | Serology | Possible |
| 49 | AML3-150 | Yes | — | 37 | >37 | Dissemin. | IPA | IPA | Neg. | Pos. | A. flavus | p.m. finding | Proven |
| 170 | BMT3-152 | Yes | 8 | 16 | 9 | Lung | Normal | ND | Pos. | Pos. | ND | p.m. finding | Proven |
| 192 | ALL | Yes | 8 | 23 | 15 | Lung/brain | IPA | IPA | Neg. | Pos. | Neg. | BAL + biopsy | Proven |
| 258 | AML3-150 | Yes | 1 | 30 | 26 | Lung | IPA | IPA | Pos. | Pos. | A. fumig. | BAL + biopsy | Proven |
| 51 | AML | Yes | — | 42 | 39 | Lung | IPA | IPA | ND | ND | ND | Radiology | Probable |
| 102 | BMT | Yes | 6 | 17 | 11 | Lung | IPA | IPA | Pos. | ND | ND | Radiology | Probable |
| 128 | AML3-150 | Yes | — | 11 | 3 | Lung | IPA | ND | Pos. | ND | Neg. | Radiology | Probable |
| 241 | AML | Yes | 8 | 13 | >13 | Lung | IPA | IPA | Neg. | ND | Neg. | Radiology | Probable |
| 360 | AML | Yes | — | 46 | >46 | Lung | IPA | IPA | Neg. | Neg. | Neg. | Radiology | Probable |
| 305 | BMT | Yes | — | 10 | 5 | Undeterm. | Normal | Normal | Pos. | ND | ND | Serology | Possible |
All patients had fever refractory to broad spectrum antibiotics for greater than 5 days plus clinical evidence of an infection (except for patients UPN 3, 50, and 51, who had only clinical evidence of an infection, but responded to broad spectrum antibiotics).
Abbreviations: A. flavus, Aspergillus flavus; A. fumig., Aspergillus fumigatus; ALL, acute lymphatic leukemia; AML, acute myeloid leukemia; BMT, autologous bone marrow transplantation; CXR, chest x-ray; CT scan, computerized tomography scan; Diagn., time after randomization (in days) when an IA was diagnosed; dissem., disseminated organ infection; Histo., histology for invasive mold; IPA, invasive pulmonary aspergillosis (air crescent sign, halo sign, or other highly compatible nodular infiltrate); Locat., location of invasive aspergillus infection; ND, not done; neg., negative; Neutr., duration of neutropenia <0.5/nL (in days) at the time an IA was diagnosed; p.m., post mortem; pos., positive; Sero., serologic tests for aspergillus; surg., surgical; Stop, discontinuation of allocated study treatment (in days after randomization); Strat., stratum used for randomization; undeterm., undetermined; UPN, unique patient number.
Patient died from aspergillus infection during or shortly after study period.
Patient started inhalations when IA was suspected.
Patient died from noninfectious multiorgan failure during study period.
Among the secondary outcome variables, there were also no statistical differences between the two trial arms, despite a trend to less fever refractory to antibiotic treatment (25% v 32%; P = .16), fewer patients who required intravenous AmB (32% v 40%;P = .11), and a lower mean cumulative dose of AmB (860v 1,068 mg; P = .16) in favor of group A with prophylactic inhalations (Table 4). The overall mortality in the trial was 45 of 382 (12%); the infection-related mortality was 30 of 382 (8%) with no statistically significant differences between the two trial arms. Noninfectious causes, bacterial infections, and fungal infections each accounted for approximately one third of the deaths that occurred during or within 14 days of the trial period (Table 4). Only 5 of 382 (1%) patients died due to IA infections. Therefore, the early mortality was only 5 of 21 (24%) among patients who developed an IA infection.
Secondary Outcome Variables
| . | Patients of Group A With Inhalations (n = 227) . | Patients of Group B Without Inhalations (n = 155) . | Significance Level . |
|---|---|---|---|
| Fever refractory to antibiotics | 57 (25%) | 49 (32%) | P = .16 |
| Intravenous AmB | 73 (32%) | 62 (40%) | P = .11 |
| Cumulative dose of AmB (in mg) | |||
| Mean (range) | 860 (100-4,335) | 1,068 (110-4,290) | P = .16 |
| Causes of death | |||
| No death | 197 (87%) | 140 (90%) | P = .62 |
| Disease progression/noninfectious | 9 (4%) | 3 (2%) | |
| Bacterial infections | 10 (4%) | 6 (4%) | |
| Fungal infections | 9 (4%) | 5 (3%) | |
| Exact cause unknown | 2 (1%) | 1 (1%) |
| . | Patients of Group A With Inhalations (n = 227) . | Patients of Group B Without Inhalations (n = 155) . | Significance Level . |
|---|---|---|---|
| Fever refractory to antibiotics | 57 (25%) | 49 (32%) | P = .16 |
| Intravenous AmB | 73 (32%) | 62 (40%) | P = .11 |
| Cumulative dose of AmB (in mg) | |||
| Mean (range) | 860 (100-4,335) | 1,068 (110-4,290) | P = .16 |
| Causes of death | |||
| No death | 197 (87%) | 140 (90%) | P = .62 |
| Disease progression/noninfectious | 9 (4%) | 3 (2%) | |
| Bacterial infections | 10 (4%) | 6 (4%) | |
| Fungal infections | 9 (4%) | 5 (3%) | |
| Exact cause unknown | 2 (1%) | 1 (1%) |
Unless otherwise indicated, values are the number of patients, with percentages in parentheses.
The overall incidence of infections was as expected in patients with hematologic malignancies and prolonged neutropenia. The rates of fever of unknown origin (38% v 37%; P = .89), bacteremia or fungemia (14% v 11%; P = .54), other microbiologically documented infections (16% v 17%; P= .79), clinically documented infections (20% v 28%;P = .08), and no evidence of infection (13% v 7%,P = .10) were not significantly different between group A and group B.
Despite initial concerns about a possible increase of bacterial pneumonias or sepsis as a result of contaminated inhalation equipments in group A, the incidence of microbiologically documented pneumonias (8% v 10%; P = .56) and gram-negative bacteremias (6% v 9%; P = .60) did not differ between the two arms of the trial. The overall incidence of pneumonias with or without microbiologic confirmation was even lower in group A as compared with group B (19% v 30%; relative risk, .86; 95% confidence interval, 0.77 to 0.98; P < .02).
Risk factors of IA infections.
The duration of neutropenia before the diagnosis of an IA infection was not different in 10 patients of group A with prophylactic inhalations as compared with 11 patients of group B without prophylactic inhalations, with medians of 14 and 15 days, respectively (P = .51 by the log-rank test). Unexpectedly, the incidence rates of IA infections also did not differ significantly between the three major disease entities: 15 of 283 (5%) in AML/MDS/CML, 2 of 35 (6%) in ALL/NHL, and 4 of 64 (6%) in auto-BMT. However, there was a wide local variation in the incidence of IA infections. Despite comparable durations of neutropenia, three centers that included 43% of the patients reported 81% of all IA infections (relative risk, 1.10; 95% confidence interval, 1.04 to 1.16; P < .003 for the comparison of these 3 centers with all other centers), corresponding to incidence rates at the participating centers ranging from 0% to 19%. Patients with IA infections had longer durations of neutropenia less than 0.5/nL, with a mean of 27 days (range, 6 to 50 days) as compared with patients without IA infections, with a mean of 22 days (range, 0 to 50 days; P = .07). Other potential risk factors, such as pre-existing neutropenia at the time of randomization, concomitant use of corticosteroids, cytokine administration, and even building reconstruction activity reported by individual centers, had no obvious influence on the incidence of IA infections.
Side effects and premature discontinuation of prophylactic aeroAmB.
Although no serious side effects occurred, about two thirds of patients reported some form of unpleasant sensation. In patient questionnaires, cough was graded as absent, mild, moderate, or severe by 57%, 29%, 7%, and 7% of patients, respectively. Bad taste was graded as absent by 48%, mild by 28%, moderate by 18%, and severe by 6% of patients. Nausea was graded as absent by 62%, mild by 21%, moderate by 9%, and severe by 8% of patients. Other side effects, such as dizziness or tightness of the chest, were mentioned infrequently. No systemic side effects and no infections could be attributed to the prophylactic aeroAmB inhalations.
As anticipated from pilot studies, 71 of 227 (31%) patients of group A discontinued prophylactic aeroAmB inhalations prematurely after a median of 6 days (range, 0 to 27 days).9 The reasons for premature discontinuation were side effects of the inhalations in 55%, inability to further cooperate in 30%, violation of the study protocol in 11%, and noncompliance in 4% of patients, respectively.
DISCUSSION
Numerous strategies to prevent IA infections have been reported, including prophylactic intranasal application of AmB sprays, low or even therapeutic doses of prophylactic intravenous AmB desoxycholate or AmB in liposomal preparations, as well as prophylactic oral itraconazol.6,7,15-20 Many of these strategies have been reported as clinically effective.15,16,22,24 However, with the large variation in the incidence rates of IA infections even within the same institution, the level of evidence from these retrospective analyses in favor of the prophylaxis is low. The few trials that investigated prophylaxis of IA infections prospectively failed to demonstrate a benefit of any of these strategies.19-21 AmB aerosol inhalations may also prevent IA infections according to several retrospective analyses and uncontrolled trials and are generally considered safe for application in neutropenic patients.9,22-25 Reductions in the incidence rates of more than 10% have been reported in patients who received prophylactic AmB aerosols as compared with historical controls.22 AmB aerosol particles are of the same size and should ideally travel the same routes as aspergillus conidia that are readily inhaled and cause IA infections in susceptible individuals.9 10 Therefore, this form of prophylaxis seemed particularly attractive in patients with prolonged neutropenia.
Over a period of 3 years, we recruited and randomly assigned 382 patients to receive either prophylactic inhalations with 10 mg of aeroAmB twice daily or no inhalation prophylaxis. A neutropenic period of 10 days or more has been reported to be associated with a high incidence of IA infections and was chosen as the entry criteria for the trial.4,26 Patients with a history of a proven, probable, or possible IA infection as well as those with pulmonary infiltrates at the time of randomization were excluded from the trial, because aeroAmB was not expected to be effective as secondary prophylaxis or as treatment of established IA infections. At present, therapeutic doses of intravenous AmB are recommended in those patients.18 To define a homogenous study population, we also excluded patients scheduled for allogeneic BMT for whom many confounding risk factors apart from neutropenia would have been present.5,17 An interim analysis that would have allowed us to stop the trial early was performed and published previously.8 Because no unexpected toxicity was observed and no unequivocal efficacy could be demonstrated after recruitment of the initial 115 patients, the trial continued to its full calculated sample size. Characteristics of patients and conduct of the trial did not change after the results of the interim analysis became available.
The majority of patients developed significant neutropenia predisposing them for the development of IA infections. The duration of neutropenia as well as the distribution of other potential risk factors for IA infections did not differ between the two arms of the trial. Similarly, as a result of the stratification, approximately equal proportions of patients at each center were randomized to receive prophylactic inhalations or no inhalation prophylaxis. Hematopoietic growth factors were more frequently used in patients who received prophylaxis with aeroAmB, but because we did not stratify randomization according to this variable, this difference might have occurred by chance alone. Generally, these agents were used as part of the routine supportive care during the trial rather than as treatment of suspected or proven IA infections. Because the duration of neutropenia did not differ between the two arms of the trial, we do not expect this imbalance to be relevant to the incidence of IA infections. Yet, some of the secondary outcome variables in the trial, such as the use of intravenous AmB or the resolution of fever, might have been influenced by this fact.
The optimal strategy to diagnose IA infections remains controversial. Whereas histologic evidence of an invasive infection in combination with a positive aspergillus culture is required to prove an IA infection, such a high level of evidence can rarely be achieved clinically. Indirect evidence for an IA infection can be obtained using clinical, radiologic, histologic, cultural, and serologic information, but particularly the usefulness of serologic tests has been debated. The primary outcome measure in the trial was the overall incidence of proven, probable, or possible IA infections. These detailed and predefined categories were constructed to integrate all available information and at the same time reflected the level of evidence in favor of the diagnosis of an IA infection. This allowed us to measure the effect of prophylactic aeroAmB according to very strict or less stringent outcome criteria.
We observed no statistically significant differences in the incidence of proven, probable, or possible IA infections in patients with or without prophylactic aeroAmB inhalations irrespective of whether we analyzed all randomized patients or only those who were fully compliant with the inhalation prophylaxis. The 4% incidence of IA infections in patients with aeroAmB prophylaxis was greater than anticipated. Likewise, the 7% incidence of IA infections in patients without aeroAmB prophylaxis was less than anticipated and equal to the 7% incidence in patients who discontinued aeroAmB prophylaxis prematurely. One patient who was fully compliant with the aeroAmB prophylaxis developed a proven IA infection as well as 3 patients who discontinued the prophylaxis prematurely after 1 and 8 days, respectively. The differences in the incidence rates of IA infections that we observed in the present trial might represent a more accurate estimation of the incidence of IA infections in a population of neutropenic patients as compared with previous reports. Institutional and temporal clustering of IA infections, the lack of a prospective control group, and publication bias might have previously contributed to an overestimate of IA infections in patients without inhalation prophylaxis as well as to an underestimate of their incidence in patients with inhalation prophylaxis.
Although there was a trend to less fever refractory to antibiotic treatment and less use of intravenous AmB in patients who received prophylaxis with aeroAmB as compared with those who did not, none of these differences was either statistically significant or clinically relevant. The mortality rates from all causes combined, as well as those from bacterial or fungal infections, were equal in both arms of the trial. Fungal infections combined accounted for about one third of all deaths that occurred during or within 14 days of the study period. The early mortality from IA infections was 24%, which is substantially lower than reported in the literature.3,27 The exclusion of some high-risk groups (ie, patients after allogeneic BMT), the greater awareness for IA infections in the present trial, the fact that most patients with IA infections recovered with their neutrophil counts, as well as better and more aggressive treatments might have contributed to the low early mortality from IA infections in the present trial.27 28
Side effects from the inhalations were reported by about two thirds of patients. Although most of these side effects were mild and no serious side effects or an increased incidence of bacterial infections could be attributed to the prophylactic inhalations, 31% of patients discontinued aeroAmB inhalations prematurely. Moreover, 30% of patients who discontinued the prophylaxis prematurely did so because they were too ill to continue with the inhalations. In these patients, systemic rather than topical prophylaxis of IA would clearly be desirable.
Several conclusions can be drawn from this final analysis and extend the conclusions from the interim analysis of the trial. IA infections remain a significant cause of morbidity and mortality in patients with prolonged neutropenia. Apart from the early mortality, delays in the antileukemic treatment and reactivation of IA infections during repetitive periods of neutropenia or after allogeneic BMT may all lead to an inferior overall treatment outcome in patients with IA infections that was not studied in the present trial. The incidence rates of IA infections varied widely among participating centers. This fact must be considered in the design of future trials as well as in the decision of whether it is worthwhile to explore prophylaxis of IA infections at an individual center. Although we could demonstrate that prophylactic aeroAmB inhalations do not completely eliminate the risk of IA infections during prolonged neutropenia, we cannot exclude the possibility that they might reduce the frequency of such infections. Given the low incidence rates and size of the present trial, we only had a 20% power to detect even a 50% reduction of IA infections using aeroAmB inhalations; conversely, to prove with a power of 90% that the differences found in the present trial did not just occur by chance, a sample size of more than 1,000 patients per arm would have been required. Prophylactic aeroAmB inhalations should therefore be studied—and indeed might be effective—in patients at an even higher risk for the development of IA infections, ie, after allogeneic BMT or during local epidemiologic outbreaks. The results of the present trial are limited to patients with neutropenia as their single or at least predominant risk factor for the development of IA infections and cannot be generalized to other patient populations. Because of acute or chronic graft-versus-host disease, immunosuppressive treatment, and other factors, many patients after allogeneic BMT are at continued risk for the development of IA infections despite recovery from neutropenia and might profit from prolonged administration of aeroAmB. Also, aerosolized lipid formulations of AmB have been successfully used as prophylaxis of IA infections in animal models. Such preparations might be considered in future trials. However, it is most important that any trial involving topical as well as systemic prophylaxis of IA infections should be performed prospectively with well-defined clinical outcome variables, as proposed for the present trial, and should consider the highly variable incidence rates of IA infections.
ACKNOWLEDGMENT
Investigators of the Departments of Hematology and Oncology from the following institutions in Germany contributed to the trial: Klinikum Rudolf Virchow (Berlin, Germany): J. Beyer, O. Boenisch, M. Ruhnke, K. Lenz, W. Siegert, and D. Huhn; Universitätsklinikum Benjamin Franklin (Berlin, Germany): S. Schwartz and E. Thiel; Universitätsklinikum Göttingen (Göttingen, Germany): G. Behre, W. Treder, B. Wörmann, and W. Hiddemann; Klinikum Groβhadern der Universität München (München, Germany): S. Bercht, D. Bosse, V. Heinemann, U. Jehn, and W. Wilmanns; Klinikum der Stadt Nürnberg (Nürnberg, Germany): R. Roidl and H. Wandt; Städtisches Klinikum Neukölln (Berlin, Germany): A. Grüneisen, B. Krause, E. Schilling, and C.A. Mayr; Medizinische Hochschule Hannover (Hannover, Germany): U. Paaz and H. Link; Robert Rössle Klinik (Berlin, Germany): F. Weber and W.-D. Ludwig; Universitätsklinikum Charité (Berlin, Germany): A. Trittin, G. Massenkeil, and K. Possinger; Universitätsklinikum Ulm (Ulm, Germany): W. Kern; Universitätsklinikum Düsseldorf (Düsseldorf, Germany): B. Arning and M. Arning; and Universitätsklinikum Münster (Münster, Germany): G. Silling-Engelhard.
Supported in part by a grant from Bristol-Myers Squibb (Munich, Germany).
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to J. Beyer, MD, Department of Hematology and Oncology, Universitätsklinikum Charité, Campus Virchow, Augustenburger Platz 1, 13353 Berlin, Germany; e-mail:jbeyer@charite.de.

![Fig. 2. Distribution of the duration of neutropenia in patients of group A with prophylactic inhalations (○) and group B without prophylactic inhalations (•). For patients with proven, probable, or possible IA, the number of neutropenic days until an IA infection was suspected or proven are marked with squares ([□] in group A and [▪] in group B).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/93/11/10.1182_blood.v93.11.3654/4/m_blod41111002x.jpeg?Expires=1763673089&Signature=zGoxj20XXZD2NpNP9BmCCWg49F1YsDgpU6tv~p4jbwqaWiXsvhwJxXp1d53fmKGGaLU~v41JKsI52yY5cnx~AdOh95EIJSx1yQR8lk3deodZuHGRlk33q0Z1ydM7gCLjT8NsyXe9EeEEEB9P6Og~BQN4wh5H19M8x2neCzvLBgxoLsAPLCT03vTf3hBPVehzHLogi-rPRqRs6TnU2UXiqK0IEVhAXDvMWQfcNJ2qXSF5utioUywARQBQJudY2Ex28T-klUuIqtGednogMVkzpbY11hUHwAzAzprb7Rtb-08i-xpkRjVHP7gC7OnkL7o297ga7eXZpcZeNqr3A-WL2A__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal