To the Editor:
Chronic leg ulcers in patients with inherited hemoglobin disorders are a cause of pain, repulsive appearance, disability, absence from or inability to work, and are a considerable cost. Conventional treatment is often disappointing. Their cause is complex. In most instances, they start as superficial abrasions resulting from minor trauma, scratches, local friction, or insect bites. Then, they expand rapidly because of the associated inadequate oxygen delivery, local edema resulting from venous insufficiency and possibly heart failure, local infections, and inappropriate medical procedures. Other factors that have been implicated include the decreased red blood cell deformability and the adherence of young reticulocytes to the vascular endothelium, which may cause obstruction of the blood flow and severe cutaneous ischemia. Fetal hemoglobin (HbF) may also interfere both by inhibiting the sickling process and through its high oxygen affinity. Chronic leg ulcers do not heal easily. Avoidance of trauma and venous congestion along with meticulous cleanness and good care of minor abrasions are a prerequisite for preventing further expansion. Other measures that have been proposed to this date include increasing the total hemoglobin with blood transfusions, improving the blood flow with pentoxifylline, preventing local thrombosis with antithrombin III, supporting the healing of the ulceration with peptide matrix, improving local oxygenation by flushing the area with oxygen, and preventing HbS polymerization through the increase of HbF with hydroxyurea, recombinant human erythropoietin (r-huEPO), or arginine butyrate (reviewed by Eckman1). In this letter, we report the beneficial effects obtained with local injections of granulocyte-macrophage colony-stimulating factor (GM-CSF; Mielogen-Molgramostin; Schering-Plough) in one patient with sickle cell disease and three patients with thalassemia whose chronic leg ulcers could not heal despite the large variety of treatments applied over the past years, including the topical impregnation with this factor, as suggested by Pieters et al2 a few years ago. Topical injections of GM-CSF have been successfully applied for the healing of chronic leg ulcers of other etiologies.3 4 Before starting, the procedure was explained to the patients and was fully accepted. The GM-CSF solution (300 μg) was injected in small portions (usually 4 to 8) through a 26-gauge needle within the margins of the ulcers, twice per week over 2 months. In some instances, a small quantity of the solution was gently applied over the open wound. Standard care was not neglected. On the occasion, the levels of interleukin-6 (IL-6), IL-1, tumor necrosis factor (TNF), IL-8, and transforming growth factor β (TGFβ), 24 hours before and 24 hours after the administration of GM-CSF, were also determined using an enzyme-linked immunosorbent assay (ELISA) technique.
Patient no. 1 was a 28-year-old man with compound Hb S/β-thalassemia (CD39) who had a chronic painful ulcer in the right ankle (3.5 × 2.5 cm) over the last 2 years. The patient had received hydroxyurea since 1995. His total Hb values varied between 8.0 and 9.0 g/dL; 33% of it was HbF. Patient no. 2 was a 49-year-old woman with thalassemia major (IVS1-nt110/CD39) and a deep ulcer in her left ankle (2.0 × 1.5 × 1.2 cm) over the last 25 years. She was on regular transfusions, maintaining a pretransfusion Hb level of 8.0 g/dL. Patient no. 3 was a 32-year-old woman with thalassemia major (IVS1-nt110/CD39). She had never complied with regular treatment and received sporadic blood transfusions, keeping a pretransfusion Hb level of approximately 6.0 g/dL. This woman had two large ulcers in her right leg (7.0 × 6.5 and 5.0 × 4.5 cm) and one ulcer in the ankle area of the left (3.0 × 3.0 cm). Patient no. 4 was a 38-year-old woman with thalassemia intermedia (IVS1-nt1/nt 1570) who had a painful ulcer in her right leg for the past 20 years (1.5 × 0.5 cm). Her usual total Hb varied around 8 g/dL; 8.0% of it was HbF.
Results and comments.
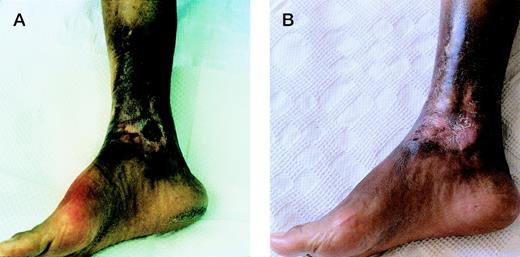
The injections were painful; a couple of hours later, there was swelling and reddening of the margins of the ulcers, frequently accompanied by fever up to 38°C. These symptoms lasted for a few hours and subsided spontaneously or with the help of minor analgesics. The patients tolerated this inconvenience, because they soon saw a favorable response. In fact, the latter was dramatic in three of them (patients no. 1, 2, and 4) in the sense that the rotten and unclean tissue was gradually replaced by healthy tissue and the ulcer healed completely in approximately 2 months (Fig1). The ulcers of patient no. 3 showed remarkable improvement but not complete healing. This may be attributed to their large size, their severe persistent contamination with staphylococcus aureus and other Gram-negative bacteria (despite the intensive local care and systematic administration of the appropriate antibiotics), and the premature termination of therapy because of an acute inflammatory reaction extending from one of the ulcers up to her groin, which appeared by the end of the second week. To this date, several months after this treatment, the ulcers have not recurred. The assay of various cytokines showed a clear increase of IL-1 and TNF along with a decrease of IL-8 (Table 1). These changes probably account for the high temperature observed in the patients after the injections of GM-CSF. The fact that the number of leukocytes in the peripheral blood did not change after each injection suggests that the action of GM-CSF was mainly local.
The deep chronic leg ulcer in patient no. 2 (A) before and (B) at the end of therapy.
The deep chronic leg ulcer in patient no. 2 (A) before and (B) at the end of therapy.
Changes of the Levels of Cytokines in the Blood of the Patients the Day Before (A) and 24 Hours After (B) the GM-CSF Injection
| . | IL-6 (pg/mL) . | IL-1β (pg/mL) . | TNFα (pg/mL) . | IL-8 (pg/mL) . | TGFβ (ng/mL) . |
|---|---|---|---|---|---|
| Patient no. 2 | |||||
| A | 3.9 | 1.7 | 0 | 4.0 | 17.4 |
| B | 5.8 | 3.5 | 5.3 | 0 | 19.3 |
| Patient no. 3 | |||||
| A | 5.5 | 12.0 | 0 | 98.7 | 24.8 |
| B | 4.2 | 17.7 | 10.3 | 3.7 | 25.4 |
| . | IL-6 (pg/mL) . | IL-1β (pg/mL) . | TNFα (pg/mL) . | IL-8 (pg/mL) . | TGFβ (ng/mL) . |
|---|---|---|---|---|---|
| Patient no. 2 | |||||
| A | 3.9 | 1.7 | 0 | 4.0 | 17.4 |
| B | 5.8 | 3.5 | 5.3 | 0 | 19.3 |
| Patient no. 3 | |||||
| A | 5.5 | 12.0 | 0 | 98.7 | 24.8 |
| B | 4.2 | 17.7 | 10.3 | 3.7 | 25.4 |
In conclusion, subcutaneous perilesional injections of GM-CSF may play an important role in the healing of chronic ulcers in patients with hemoglobinopathies, especially when these have persisted over several years despite intensive treatment, as in the case of the patients of this report. Treatment is relatively well-tolerated and the associated side effects (pain and fever) respond easily to mild analgesics. The activity of GM-CSF is pleiotropic. It includes local attraction of neutrophils, hence improving the clearance of bacteria and debris, promotion of neovascularization, enhancement of keratinization, and acceleration of the formation of new tissue.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal