Abstract
Hairy cell leukemia is a chronic B-cell disorder that follows an indolent, but progressive course. Cladribine (2-chlorodeoxyadenosine) induces complete remissions in the majority of patients after a single course. We report the long-term outcomes, including response rates and their duration; time-to-treatment failure (TTF) rates; retreatment results; toxicities; and survival rates of patients treated at Scripps Clinic (La Jolla, CA). A total of 358 patients with hairy cell leukemia were treated with cladribine at 0.087 or 0.1 mg/kg body weight per day by continuous intravenous infusion for 7 days. The expected number of second neoplasms was based on the National Cancer Institute’s Surveillance Epidemiology and End Results data. Of 349 evaluable patients, 319 (91%) achieved an initial complete response and 22 (7%) a partial response with an overall median duration of response follow-up of 52 months. Ninety patients (26%) had relapsed at a median of 29 months. The TTF rate for all 341 responders was 19% at 48 months, 16% for complete responders, and 54% for partial responders. Of 53 evaluable patients treated with second courses of cladribine at first relapse, 33 (62%) achieved complete responses and 14 (26%) partial responses. Twenty-seven patients (8%) developed second neoplasms (only 1 hematopoietic) with an observed-to-expected ratio of 1.88 (95% confidence interval, 1.24 to 2.74). The overall survival rate was 96% at 48 months. Single courses of cladribine induced long-lasting complete responses in the vast majority of patients. Relapse rates for complete responders were low. Patients who relapse can be successfully retreated with cladribine. Cladribine has high efficacy and a favorable acute and long-term toxicity profile when administered to patients with hairy cell leukemia.
© 1998 by The American Society of Hematology.
HAIRY CELL LEUKEMIA is an uncommon chronic B-cell lymphoproliferative disorder characterized by mononuclear cells displaying cytoplasmic projections.1Typically, the disease follows an indolent, but progressive course.2 Patients present with pancytopenia, splenomegaly, and recurrent infections. Interferon-α induces partial responses in most patients but complete responses in only the minority.3Two newer purine analogues, 2′-deoxycoformycin (pentostatin, Nipent, Supergen, San Ramon, CA) and 2-chlorodeoxyadenosine (cladribine; Leustatin, Ortho Biotech, Raritan, NJ) induce long-lasting complete remissions in the majority of patients with hairy cell leukemia.3-5
In 1990, Piro et al6 at Scripps Clinic reported on 12 hairy cell leukemia patients, each of whom received a single infusion of cladribine at 0.1 mg/kg body weight daily for 7 days; 11 had complete responses and the twelfth patient a partial response. Similar high response rates were subsequently reported by other institutions.7-9 Herein we report the long-term follow-up of 358 patients documenting response rates and their duration, retreatment results, time-to-treatment failure (TTF) rates, and the incidence of second malignancies.
MATERIALS AND METHODS
Eligibility criteria and treatment indications.
Patients required a diagnosis of hairy cell leukemia based on review of the peripheral blood, bone marrow, and/or splenic tissue (in splenectomized patients) as centrally reviewed by hematopathologists at Scripps Clinic. Neutropenia (absolute neutrophil count <1.0 × 109/L), anemia (hemoglobin <10 g/dL), thrombocytopenia (platelets <100 × 109/L), symptomatic splenomegaly, or repeated infections were required before administering cladribine. Patients were eligible for cladribine treatment regardless of the percent infiltration by hairy cell leukemia of the bone marrow only if these criteria were met. There were no age restrictions. Patients were excluded if they had received treatment within 4 weeks of cladribine therapy, if they had an active infection, or if they had abnormal renal or hepatic functions. The same criteria were used for retreatment with cladribine at the time of relapse. The study was approved by the Scripps Clinic institutional review board, and written informed consent was obtained.
Patient population.
Of 365 consecutive patients followed from April 1986 to January 1993, 357 patients had hairy cell leukemia and 1 patient had hairy cell leukemia-variant. Seven patients were excluded after they were reclassified as low-grade non-Hodgkin’s lymphoma (3 patients), marginal zone lymphoma (3 patients, 1 of which had splenic lymphoma with circulating villous lymphocytes), and B-cell prolymphocytic leukemia (1 patient). Follow-up was through April 1997. Of the 358 eligible patients, there were 290 men and 68 women with a median age of 53 years (range, 24 to 88; Table 1). Of 320 patients who underwent cytochemical examination of the peripheral blood smear and/or marrow for tartrate-resistant acid phosphatase (TRAP), 270 were TRAP positive and 50 were TRAP negative; 38 patients were not evaluated by TRAP stain. One hundred seventy-nine patients were untreated; 95 had undergone splenectomy and 135 had received prior systemic therapy (132 with interferon and 8 with 2′-deoxycoformycin). Sixty-seven patients treated with cladribine were randomized between placebo and pentoxifylline in an attempt to ameliorate cladribine-induced toxicities.10 11 Median duration from diagnosis of hairy cell leukemia to the first cladribine course was 16.2 months (range, 6 days to 233 months). For patients who received prior interferon, median duration of interferon therapy was 12 months (range, 1 day to 67 months).
Patient Demographics
| No. of patients | 358 |
| Prior therapy | |
| None | 179 |
| Splenectomy alone | 44 |
| Interferon alone | 78 |
| Splenectomy, interferon | 47 |
| Splenectomy, interferon, 2′-deoxycoformycin | 4 |
| Interferon, 2′-deoxycoformycin | 3 |
| 2′-Deoxycoformycin alone | 1 |
| Other regimens | 2 |
| Spleen size | |
| Splenectomized | 98 |
| No splenomegaly | 71 |
| Mild (1-2 fingerbreadths) | 50 |
| Moderate (3-4 fingerbreadths) | 58 |
| Massive (greater than 4 fingerbreadths) | 76 |
| Unknown | 5 |
| Lymphadenopathy | 109 |
| Peripheral blood hematologic parameters | |
| Absolute neutrophil count (×109/L) | |
| Median (range) | 0.9 (0.1-12.5) |
| Hemoglobin level (g/dL) | |
| Median (range) | 11.3 (4.6-16.6) |
| Platelets (×109/L) | |
| Median (range) | 81 (7-575) |
| Peripheral blood immunophenotypic profile | |
| Typical for hairy cell leukemia (CD11c, CD25, and CD103 all positive) | 174 |
| Atypical for hairy cell leukemia (one or more markers negative) | 35 |
| Not done | 149 |
| Bone marrow infiltration by hairy cells (percentage) | |
| Median | 80 |
| Range | 1-100 |
| No. of patients | 358 |
| Prior therapy | |
| None | 179 |
| Splenectomy alone | 44 |
| Interferon alone | 78 |
| Splenectomy, interferon | 47 |
| Splenectomy, interferon, 2′-deoxycoformycin | 4 |
| Interferon, 2′-deoxycoformycin | 3 |
| 2′-Deoxycoformycin alone | 1 |
| Other regimens | 2 |
| Spleen size | |
| Splenectomized | 98 |
| No splenomegaly | 71 |
| Mild (1-2 fingerbreadths) | 50 |
| Moderate (3-4 fingerbreadths) | 58 |
| Massive (greater than 4 fingerbreadths) | 76 |
| Unknown | 5 |
| Lymphadenopathy | 109 |
| Peripheral blood hematologic parameters | |
| Absolute neutrophil count (×109/L) | |
| Median (range) | 0.9 (0.1-12.5) |
| Hemoglobin level (g/dL) | |
| Median (range) | 11.3 (4.6-16.6) |
| Platelets (×109/L) | |
| Median (range) | 81 (7-575) |
| Peripheral blood immunophenotypic profile | |
| Typical for hairy cell leukemia (CD11c, CD25, and CD103 all positive) | 174 |
| Atypical for hairy cell leukemia (one or more markers negative) | 35 |
| Not done | 149 |
| Bone marrow infiltration by hairy cells (percentage) | |
| Median | 80 |
| Range | 1-100 |
Six patients had 5% or less marrow involvement by hairy cell leukemia pretreatment. All six patients had circulating hairy cells in their peripheral blood; four by light microscopic examination of the buffy coat preparation, all six by peripheral blood immunophenotypic analysis, and one by electron microscopy. Three of these six patients had prominent splenomegaly, one had no palpable enlargement of the spleen, and two were previously splenectomized with splenic tissue showing hairy cell leukemia.
A second neoplasm was defined as any invasive malignancy, with the exception that nonmelanoma localized skin (squamous or basal) cancer was excluded.
Drug therapy, supportive care, and toxicity monitoring.
Patients received single courses of cladribine as continuous intravenous infusions. Before cladribine became commercially available, it was synthesized at Scripps Clinic by Dr Ernest Beutler and given at a dose of 0.087 mg/kg body weight daily over 7 days (patients 1 to 224), and from June 1991, cladribine was provided by Ortho Biotech (patients 225 to 365) at a dose of 0.1 mg/kg daily over 7 days. The drug synthesized at Scripps Clinic was standardized by using the extinction coefficient of chloroadenine, which was slightly lower than cladribine. Accordingly, the actual dose administered was only 87% of the amount intended.12
Initially, patients were hospitalized to administer cladribine as a continuous infusion, but later they were treated as outpatients by using peripherally inserted central catheters and computerized ambulatory drug delivery portable infusion pumps (Pharmacia Deltec, St Paul, MN). Patients were first orally given 300 mg allopurinol daily to prevent hyperuricemia of tumor lysis, but given its absence this practice was later discontinued. Also, initially all neutropenic patients with fevers greater than 38.5°C were hospitalized for prophylactic broad spectrum intravenous antibiotics. Given the rarity of documented infections, fever was later attributed to cytokine release and treated empirically with acetaminophen. For fevers greater than 38.5°C, shaking chills or rigors, or an inability to maintain oral hydration despite the use of acetaminophen, patients were hospitalized. Granulocyte colony-stimulating factors were not administered.
Pretreatment, patients had a physical examination, complete blood count with differential, chemistry 24 panel (Boehringer-Mannheim Diagnostics, Indianapolis, IN), chest radiograph, computerized axial tomographic (CAT) scan of the abdomen and pelvis, bone marrow aspiration and biopsy, and TRAP staining of the peripheral blood smear and/or marrow. Peripheral blood immunophenotypic analysis was performed in 209 of the 358 patients. In 149 patients immunophenotyping was not performed on the peripheral blood or bone marrow. Monoclonal antibodies against the B-cell antigens CD19, CD20, and CD22 were applied, and coexpression of CD11c, CD25, and CD103 was evaluated. Typical immunophenotypic analysis required the presence of all three antigens, CD11c, CD25, and CD103, whereas atypical analysis indicated the absence of one or more of these markers.
During treatment, patients had a complete blood count performed every other day and the chemistry 24 panel was repeated on day 7; after the completion of therapy the complete blood count was repeated weekly for approximately 10 weeks, monthly for 4 months, and then every 3 to 6 months. Patients underwent repeat bone marrow examinations at 3 months, 6 months, 12 months, 24 months, and then every 12 to 24 months thereafter. Bone marrow examinations were repeated earlier for new onset cytopenias or splenomegaly to document marrow relapse (if present) and prior to the institution of any chemotherapeutic agent after the single course of cladribine. The resolution of hepatomegaly and splenomegaly for response determination was by physical examination only. Repeat chest radiographs and computed tomography (CAT) scans of the abdomen and pelvis were performed in those patients whose pretreatment imaging studies showed significant lymphadenopathy (lymph nodes ≥2 cm).13
Toxicity was evaluated using standard criteria.14Hematologic toxicity was graded according to nadir blood counts irrespective of pretreatment values or percent decrement. Acute toxicities occurred within 6 months of cladribine and delayed adverse events thereafter.
Response criteria and relapse definition.
Complete response was the disappearance of all evidence of disease. The complete blood count had ≥1.5 × 109 neutrophils/L, ≥12.0 g hemoglobin/dL, ≥100 × 109 platelets/L, and the absence of any hairy cells on peripheral blood smear. Absence of disease on marrow aspiration and biopsy specimens was required. Physical examination showed no palpable lymphadenopathy nor hepatosplenomegaly. In those patients with baseline lymphadenopathy on chest radiograph and/or CAT scans of the abdomen and pelvis, follow-up imaging studies showed all lymph nodes to be 2 cm or less in diameter. Peripheral blood immunophenotypic analysis and marrow immunohistochemical staining (L26 and DBA.44) were not included in the definition of complete response.
Partial response required greater than 50% reduction in the absolute hairy cell count in the peripheral blood and bone marrow, greater than 50% improvement of all cytopenias, and greater than 50% reduction in abnormal lymphadenopathy or hepatosplenomegaly. Patients not meeting response criteria were scored as nonresponders.
Relapse after complete response was defined as the reappearance of hairy cells in the peripheral blood smear and/or bone marrow (regardless of the degree of infiltration), development of peripheral blood cytopenias, and/or splenomegaly on physical examination. Relapse after partial response was a greater than 50% increase of residual hairy cells in the marrow, development of cytopenias, splenomegaly on physical examination insufficient to qualify as a partial response, or reappearance of hairy cells in the bone marrow of those patients classified as partial responders based on residual splenomegaly only.
Statistical analysis.
TTF was defined for patients achieving a complete or partial response and was measured from the date of cladribine treatment until first relapse or death from any cause, whichever came first. Observations of TTF were censored at date of last contact for patients with no report of relapse who were last known to be alive. Overall survival was determined from date of treatment until death from any cause. Observations were censored for patients last known to be alive. TTF and overall survival estimates were determined by the method of Kaplan and Meier.15 The prognostic significance of baseline covariates on TTF and overall survival was examined with two-sided log rank statistics. The following pretreatment parameters were considered, age (> or <50 years), sex, splenomegaly (presence or absence), splenectomy, disease duration (<12 months, 12 to 24 months, 24 to 36 months, or >36 months), bone marrow infiltration (> or <20%), absolute neutrophil count (> or <0.5 × 109/L), white blood cell count (> or <15 × 109/L), platelets (> or < 50 × 109/L), hemoglobin (> or <9 g/dL), TRAP staining (positive or negative), and immunophenotype (typical or atypical). Variables found to have a P value of .30 or less were then included as covariates in a stepwise Cox proportional hazards model, with a type I error of 0.05.16
Time at risk for second malignancy was computed from date of cladribine to date of diagnosis of second malignancy, date of last examination, last patient contact, or date of death, whichever came first. Excess of second malignancies was expressed by the ratio of observed-to-expected cases from the United States general population. Expected numbers were calculated by using cancer incidence rates specific for age (in 5-year categories) and sex, for 1987 to 1991, as prepared by the Surveillance Epidemiology and End Results (SEER) Program of the National Cancer Institute.17 Cancer incidence rates were multiplied by observed person-years at risk in each age category to estimate expected frequency of second malignancies. Confidence intervals of observed-to-expected ratios were obtained by assuming a Poisson distribution for the observed numbers.
RESULTS
Response.
Of 358 patients treated with cladribine, 349 were evaluable for response and all were evaluable for toxicity (9 patients were not assessable for long-term response evaluation; 5 patients improved or normalized their peripheral blood counts but failed to undergo a bone marrow examination posttreatment, 2 patients had complete normalization of their peripheral blood counts but only underwent a single bone marrow examination posttreatment at 3 months [partial response] and 5 months [no response], which precluded long-term response determination, and 2 patients lacked any long-term response information). After single courses of cladribine, 319 (91%) of 349 patients achieved complete responses and 22 (7%) achieved partial responses, for an overall response rate of 98%. Response rates to cladribine were independent of prior therapy. Median duration of response follow-up for complete responders was 53 months (range, 1 to 134 months), and median response duration for partial responders was 37 months (range, 6 to 74 months). Median duration of response follow-up for all responders was 52 months (range, 1 to 134 months). Among the responders, bone marrow compliance was 84% at 3 months, 66% at 6 months, 70% at 12 months, 56% at 24 months, 47% from 25 to 50 months, and 57% at 75 months.
Of the 22 patients who achieved a partial response, 14 had residual disease in the marrow in the absence of splenomegaly on physical examination or peripheral blood cytopenias. Three partial responders had persistent marrow disease associated with splenomegaly as well as cytopenias (2 with thrombocytopenia and 1 with anemia). Five patients were assessed as partial responders because of isolated cytopenias only; 3 with thrombocytopenia, 1 with anemia, and 1 with neutropenia. No patients were classified as having a partial response on the basis of mild residual lymphadenopathy on chest radiograph and/or CT scans or hepatomegaly on physical examination. Thirteen of the patients who scored as partial responders underwent a peripheral blood immunophenotypic analysis; 10 were typical (CD11c, CD25, and CD103 expression), and 3 were atypical (absence of one of these surface markers; 1 had hairy cell leukemia-variant by morphology).
Median follow-up duration for all 358 patients (responders and nonresponders) was 58 months (range, 1 to 134 months), for complete responders was 59 months (range, 1 to 134 months), and for partial responders was 60 months (range, 17 to 83 months). For the 349 patients who underwent a posttreatment bone marrow examination, the median interval between the most recent bone marrow examination and last patient contact was 23 months (range, 0 to 72 months), and the median number of posttreatment bone marrow examinations performed was 4 (range, 1 to 13).
Eight patients were nonresponders after their first cladribine course; three received no further therapy and five were further treated. Only one of three patients who received a second course of cladribine achieved a brief partial response, one patient who underwent a splenectomy had improved peripheral blood hematologic parameters, and one patient who received cyclophosphamide, adriamycin, vincristine, and prednisone (CHOP) chemotherapy did not respond.
Relapse and retreatment results.
Ninety of 341 patients (26%) who achieved a response relapsed; 76 of 319 complete responders (24%) relapsed at a median of 30 months (range, 7 to 85 months) and 14 of 22 partial responders (64%) relapsed at a median of 24 months (range, 6 to 40 months). The sites of relapse are indicated in Table 2. Median time to first relapse was 29 months (range, 6 to 85 months).
Patients at First Relapse Following Cladribine
| Number | 90 |
| Age | |
| Median (yr) | 52 |
| Range | 34-77 |
| Sex | |
| Male | 75 |
| Female | 15 |
| Disease duration before 2-CdA | |
| Median (mo) | 11 |
| Range | 0-233 |
| Treatment before 2-CdA | |
| None | 48 |
| Splenectomy alone | 10 |
| Interferon alone | 13 |
| Splenectomy, interferon | 12 |
| Splenectomy, interferon, 2′-deoxycoformycin | 2 |
| 2′-Deoxycoformycin alone | 1 |
| 2′-Deoxycoformycin, interferon | 1 |
| Other regimens | 3 |
| First response to 2-CdA | |
| Complete response | 76 |
| Partial response | 14 |
| Peripheral blood hematologic parameters at first relapse | |
| Absolute neutrophil count (×109/L) | |
| Median (range) | 2.1 (0.1-23.3) |
| Hemoglobin level (g/dL) | |
| Median (range) | 14.3 (4.8-17.5) |
| Platelet (×109/L) | |
| Median (range) | 163 (40-537) |
| Site of relapse | |
| Bone marrow | 78 |
| Peripheral blood | |
| Cytopenias alone | 3 |
| Circulating hairy cells alone | 7 |
| Cytopenias and circulating hairy cells | 1 |
| Splenomegaly and retroperitoneal lymphadenopathy | 1 |
| Duration to first relapse from 2-CdA therapy | |
| Median (months) | 29 |
| Range | 6-85 |
| Treatment at relapse | |
| None | 24 |
| 2-CdA | 63 |
| Splenectomy (later 2-CdA) | 2 |
| Interferon | 1 |
| Response to second course of 2-CdA (65 patients) | |
| Complete response | 33 |
| Partial response | 14 |
| No response | 6 |
| Unknown | 12 |
| Number | 90 |
| Age | |
| Median (yr) | 52 |
| Range | 34-77 |
| Sex | |
| Male | 75 |
| Female | 15 |
| Disease duration before 2-CdA | |
| Median (mo) | 11 |
| Range | 0-233 |
| Treatment before 2-CdA | |
| None | 48 |
| Splenectomy alone | 10 |
| Interferon alone | 13 |
| Splenectomy, interferon | 12 |
| Splenectomy, interferon, 2′-deoxycoformycin | 2 |
| 2′-Deoxycoformycin alone | 1 |
| 2′-Deoxycoformycin, interferon | 1 |
| Other regimens | 3 |
| First response to 2-CdA | |
| Complete response | 76 |
| Partial response | 14 |
| Peripheral blood hematologic parameters at first relapse | |
| Absolute neutrophil count (×109/L) | |
| Median (range) | 2.1 (0.1-23.3) |
| Hemoglobin level (g/dL) | |
| Median (range) | 14.3 (4.8-17.5) |
| Platelet (×109/L) | |
| Median (range) | 163 (40-537) |
| Site of relapse | |
| Bone marrow | 78 |
| Peripheral blood | |
| Cytopenias alone | 3 |
| Circulating hairy cells alone | 7 |
| Cytopenias and circulating hairy cells | 1 |
| Splenomegaly and retroperitoneal lymphadenopathy | 1 |
| Duration to first relapse from 2-CdA therapy | |
| Median (months) | 29 |
| Range | 6-85 |
| Treatment at relapse | |
| None | 24 |
| 2-CdA | 63 |
| Splenectomy (later 2-CdA) | 2 |
| Interferon | 1 |
| Response to second course of 2-CdA (65 patients) | |
| Complete response | 33 |
| Partial response | 14 |
| No response | 6 |
| Unknown | 12 |
Of 90 patients who relapsed, 24 received no further therapy, 63 were retreated with a second cladribine course, 2 underwent splenectomy (no response) and thereafter received cladribine, and 1 received interferon (Table 2). Response information after a second cladribine course is available for 53 of these 65 patients; 7 were only recently retreated and their second response status is unknown, 5 were lost to follow-up, and 1 died after CHOP chemotherapy for low-grade non-Hodgkin’s lymphoma. Of 53 patients who received second courses of cladribine at first relapse, 33 (62%) achieved complete responses and 14 (26%) partial responses.
Thus far, 19 patients experienced a second relapse after having received two prior courses of cladribine. Second relapse was first documented on bone marrow examination in 17 patients and by peripheral blood cytopenias in 2 patients. These 19 patients had a median second response duration of 23 months (range, 3 to 59 months). At second relapse, the median absolute neutrophil count was 1.7 × 109/L (range, 0.8 to 6.7 × 109/L), median hemoglobin 13.1 g/dL (range, 8.1 to 16.8), and median platelet count 132 × 109/L (range, 28 to 248 × 109/L). Of these 19 patients, 7 received no further therapy, 7 received a third course of 2-CdA (2 complete responses, 4 partial responses, and 1 no response), 3 received interferon (1 partial response and 2 nonresponders), single patients each received 2’-deoxycoformycin and B4 blocked ricin (no response), and the response status of 1 patient is unknown.
Treatment at relapse with splenectomy, interferon, and/or 2′-deoxycoformycin.
Five patients underwent splenectomy after cladribine; one with symptomatic splenic infarction, one had hypersplenism but on pathological review of the spleen no hairy cells were identified, and three had persistent massive splenomegaly.
Eleven patients who relapsed after receiving cladribine were treated with interferon and/or 2′-deoxycoformycin; 5 first received interferon and later 2′-deoxycoformycin, 4 received interferon only, and 2 received 2′-deoxycoformycin alone (Table 3). Of the 9 patients who received interferon, 3 achieved responses (2 partial responses and 1 complete response), and of the 7 patients who received 2′-deoxycoformycin, 6 achieved responses (3 complete and 3 partial responses). Of the 5 patients who first received interferon and later 2′-deoxycoformycin, 2 nonresponders achieved a partial and complete response, respectively, and 1 partial responder had a complete response.
Responses to Interferon and 2′-Deoxycoformycin Therapy After Cladribine
| Patient . | Cladribine . | Interferon . | 2′-Deoxycoformycin . | |
|---|---|---|---|---|
| No. of Courses . | Responses . | |||
| 1* | 4 | NR, NR, NR, NR | NR | PR |
| 2 | 2 | PR, PR | PR | PR |
| 3 | 2 | PR, CR | NR | CR |
| 4* | 1 | NR | NR | — |
| 5* | 3 | CR, CR, PR | NR | NR |
| 6 | 3 | CR, CR, NR | CR | — |
| 7 | 4 | CR, NR, NR, NR | — | CR |
| 8* | 2 | PR, NR | NR | — |
| 9 | 3 | CR, CR, PR | — | PR |
| 10 | 2 | CR, NR | PR | CR |
| 11 | 1 | CR | NR | — |
| Patient . | Cladribine . | Interferon . | 2′-Deoxycoformycin . | |
|---|---|---|---|---|
| No. of Courses . | Responses . | |||
| 1* | 4 | NR, NR, NR, NR | NR | PR |
| 2 | 2 | PR, PR | PR | PR |
| 3 | 2 | PR, CR | NR | CR |
| 4* | 1 | NR | NR | — |
| 5* | 3 | CR, CR, PR | NR | NR |
| 6 | 3 | CR, CR, NR | CR | — |
| 7 | 4 | CR, NR, NR, NR | — | CR |
| 8* | 2 | PR, NR | NR | — |
| 9 | 3 | CR, CR, PR | — | PR |
| 10 | 2 | CR, NR | PR | CR |
| 11 | 1 | CR | NR | — |
Abbreviations: CR, complete response; PR, partial response; NR, no response.
Deceased.
Acute toxicities.
Lethal acute and delayed toxicities are separately reported. Of the first 135 consecutive patients treated, 22 (16%) experienced grade-3 neutropenia (absolute neutrophil 0.5 to 1.0 × 109/L) and 96 (71%) had grade-4 neutropenia (absolute neutrophil count <0.5 × 109/L). Fourteen patients (10%) experienced grade-3 thrombocytopenia (platelets 25 to 50 × 109/L) and 14 (10%) had grade-4 thrombocytopenia (platelets <25 × 109/L). Grade-3 anemia (hemoglobin <8 g/dL) was documented in 27 patients (20%), and 3 (2%) had grade-4 anemia (hemoglobin <6.5 g/dL). Median recovery time to normalization of peripheral blood counts after the first cladribine course was 49 days (range, 9 to 378 days) and after the second cladribine course was 45 days (range, 9 to 98 days).
Of 358 patients treated, 149 (42%) developed neutropenic fever (temperature >38.5°C) and 45 (13%) had documented infections. Oral herpes simplex was cultured from 5 patients, 3 patients developed herpes zoster (2 dermatomal and 1 disseminated), and 1 patient had acute cytomegalovirus retinitis. The most common bacterial infection was staphylococcal; 10 patients were bacteremic, and 23 grewstaphylococcus from their catheter tip or from the skin of associated cellulitis. Single patients each developed β hemolytic streptococcus, streptococcus pneumoniae, enterobacter, Escherichia coli (associated with a perirectal abscess) and micrococcus bacteremia. Three patients had bacterial urinary tract infections;Escherichia coli, gram-positive cocci (not further identified), and coagulase-negative staphylococcus. One patient had Branhamella catarrhalis cultured from his sputum without a pulmonary infiltrate on chest radiograph, and 1 patient received intravenous antibiotics with response for culture-negative pneumonia. There were no acute fungal infections.
One patient underwent emergency splenectomy for splenic rupture midway through his first cladribine course, and one patient developed transient chylous ascites. Two patients experienced cardiac arrhythmias; one paroxysmal atrial tachycardia and one ventricular tachycardia.
Delayed adverse events and second malignancies.
Dermatomal herpes zoster was the most frequent late infection (Table 4). Both patients with positive hepatitis C serology had received prior transfusions. Two patients developed motor peripheral neuropathies, one being reversible, and one patient with severe vertebral spondylosis experienced transverse myelitis 4.5 years after cladribine.
Nonlethal Delayed Adverse Events
| Adverse Event (No. of Patients) . | Months From First Cladribine Therapy . |
|---|---|
| Infections | |
| Herpes zoster, dermatomal (7) | 10, 18, 20, 24, 41, 42, 69 |
| Hepatitis C (2) | 31, 51 |
| Mycobacterium tuberculosis (1) | 21 |
| Mycobacterium chelonei (1) | 38 |
| Cardiac or cerebrovascular | |
| Myocardial infarction (1) | 43 |
| Stroke (1) | 53 |
| Pulmonary | |
| Pneumonia, etiology undetermined (2) | 24, 52 |
| Interstitial lung disease (1) | 44 |
| Pulmonary embolism (1) | 66 |
| Neurological | |
| Peripheral neuropathy (2) | 9, 25 |
| Transverse myelitis (1) | 54 |
| Miscellaneous | |
| Thyrotoxicosis (2) | 17, 54 |
| Psoriatic arthropathy (1) | 34 |
| Polymyalgia rheumatica (1) | 36 |
| Adverse Event (No. of Patients) . | Months From First Cladribine Therapy . |
|---|---|
| Infections | |
| Herpes zoster, dermatomal (7) | 10, 18, 20, 24, 41, 42, 69 |
| Hepatitis C (2) | 31, 51 |
| Mycobacterium tuberculosis (1) | 21 |
| Mycobacterium chelonei (1) | 38 |
| Cardiac or cerebrovascular | |
| Myocardial infarction (1) | 43 |
| Stroke (1) | 53 |
| Pulmonary | |
| Pneumonia, etiology undetermined (2) | 24, 52 |
| Interstitial lung disease (1) | 44 |
| Pulmonary embolism (1) | 66 |
| Neurological | |
| Peripheral neuropathy (2) | 9, 25 |
| Transverse myelitis (1) | 54 |
| Miscellaneous | |
| Thyrotoxicosis (2) | 17, 54 |
| Psoriatic arthropathy (1) | 34 |
| Polymyalgia rheumatica (1) | 36 |
After cladribine, 27 (23 males) of 358 patients (8%) developed second malignancies: 5 melanomas, 11 adenocarcinoma of the prostate, 4 adenocarcinoma of the colon, 3 adenocarcinoma of the stomach, 1 transitional cell carcinoma of the bladder, 1 renal cell carcinoma, 1 neuroendocrine tumor of the bladder, 1 low-grade non-Hodgkin’s lymphoma (well-differentiated lymphocytic lymphoma), and 1 cerebellar hemangioblastoma (Table 5). Of these 27 patients, 16 were previously untreated, 5 had received interferon, 3 were splenectomized, and 3 had undergone splenectomy and prior interferon. Patient 7, with a remote history of colon cancer, developed both adenocarcinoma of the prostate and stomach. Three patients relapsed from prior malignancies: patient 3, from melanoma; patient 15, from adenocarcinoma of the prostate; and patient 23, from transitional cell carcinoma of the bladder.
Second Malignancies After Cladribine Treatment of Hairy Cell Leukemia
| Patient . | Second Cancer . | HCL Therapy Prior to Cladribine . | Age at Diagnosis of 2nd Cancer (yrs) . | Time (mo) From Diagnosis of HCL to 2nd Cancer . | Time (mo) From Cladribine to 2nd Cancer . | Survival (mo) From Diagnosis of HCL . | Survival (mo) After Diagnosis of 2nd Cancer . | Status . |
|---|---|---|---|---|---|---|---|---|
| 1 | Melanoma | None | 64 | 18 | 12 | 82 | 63 | Alive |
| 2 | Melanoma | None | 76 | 76 | 57 | 87 | 10 | Alive |
| 3 | Melanoma, metastatic | None | 48 | 16 | 9 | 70 | 54 | Dead |
| 4 | Melanoma | None | 70 | 68 | 42 | 86 | 20 | Alive |
| 5 | Melanoma | None | 74 | 4 | 3 | 40 | 36 | Alive |
| 6 | Adenocarcinoma, prostate | Interferon | 77 | 75 | 21 | 128 | 53 | Alive |
| 7 | Adenocarcinoma, prostate | None | 71 | 9 | 4 | 85 | 74 | Alive |
| Adenocarcinoma, stomach | None | 73 | 36 | 30 | 85 | 49 | ||
| 8 | Adenocarcinoma, prostate | Interferon | 62 | 56 | 37 | 92 | 35 | Alive |
| 9 | Adenocarcinoma, prostate | None | 51 | 81 | 51 | 103 | 22 | Alive |
| 10 | Adenocarcinoma, prostate | None | 52 | 110 | 20 | 120 | 10 | Alive |
| 11 | Adenocarcinoma, prostate | Interferon | 61 | 85 | 22 | 130 | 45 | Alive |
| 12 | Adenocarcinoma, prostate | Interferon | 67 | 62 | 13 | 101 | 38 | Alive |
| 13 | Adenocarcinoma, prostate | None | 80 | 58 | 21 | 84 | 26 | Alive |
| 14 | Adenocarcinoma, prostate | None | 72 | 30 | 29 | 62 | 32 | Alive |
| 15 | Metastatic adenocarcinoma, prostate | None | 78 | 1 | 1 | 47 | 46 | Alive |
| 16 | Metastatic adenocarcinoma, prostate | Interferon | 75 | 72 | 11 | 75 | 3 | Dead |
| 17 | Adenocarcinoma, colon (Duke’s B2) | Interferon, Splenectomy | 64 | 125 | 46 | 141 | 16 | Alive |
| 18 | Adenocarcinoma, colon (Duke’s B2) | None | 56 | 30 | 26 | 48 | 17 | Dead |
| 19 | Adenocarcinoma, colon (Duke’s B2) | Splenectomy | 53 | 188 | 1 | 241 | 52 | Alive |
| 20 | Adenocarcinoma, colon (Duke’s C1) | None | 45 | 7 | 5 | 56 | 49 | Alive |
| 21 | Adenocarcinoma, stomach | None | 66 | 62 | 58 | 83 | 21 | Alive |
| 22 | Metastatic adenocarcinoma, stomach | Interferon, splenectomy | 66 | 105 | 31 | 106 | 1 | Dead |
| 23 | Transitional cell carcinoma, bladder | Splenectomy | 65 | 24 | 11 | 75 | 50 | Alive |
| 24 | Renal cell carcinoma | None | 70 | 16 | 15 | 76 | 60 | Alive |
| 25 | Metastatic neuroendocrine tumor, bladder | Splenectomy | 73 | 123 | 41 | 132 | 9 | Dead |
| 26 | Low-grade non-Hodgkin’s lymphoma | None | 71 | 109 | 9 | 19 | 8 | Dead |
| 27 | Cerebellar hemangioblastoma | Splenectomy, interferon | 61 | 80 | 6 | 153 | 73 | Alive |
| Medians | 67 (yr) | 62 (yr) | 21 (mo) | 85 (mo) | 36 (mo) | |||
| (Range) | (45-80) | (1-188) | (1-58) | (19-241) | (1-74) |
| Patient . | Second Cancer . | HCL Therapy Prior to Cladribine . | Age at Diagnosis of 2nd Cancer (yrs) . | Time (mo) From Diagnosis of HCL to 2nd Cancer . | Time (mo) From Cladribine to 2nd Cancer . | Survival (mo) From Diagnosis of HCL . | Survival (mo) After Diagnosis of 2nd Cancer . | Status . |
|---|---|---|---|---|---|---|---|---|
| 1 | Melanoma | None | 64 | 18 | 12 | 82 | 63 | Alive |
| 2 | Melanoma | None | 76 | 76 | 57 | 87 | 10 | Alive |
| 3 | Melanoma, metastatic | None | 48 | 16 | 9 | 70 | 54 | Dead |
| 4 | Melanoma | None | 70 | 68 | 42 | 86 | 20 | Alive |
| 5 | Melanoma | None | 74 | 4 | 3 | 40 | 36 | Alive |
| 6 | Adenocarcinoma, prostate | Interferon | 77 | 75 | 21 | 128 | 53 | Alive |
| 7 | Adenocarcinoma, prostate | None | 71 | 9 | 4 | 85 | 74 | Alive |
| Adenocarcinoma, stomach | None | 73 | 36 | 30 | 85 | 49 | ||
| 8 | Adenocarcinoma, prostate | Interferon | 62 | 56 | 37 | 92 | 35 | Alive |
| 9 | Adenocarcinoma, prostate | None | 51 | 81 | 51 | 103 | 22 | Alive |
| 10 | Adenocarcinoma, prostate | None | 52 | 110 | 20 | 120 | 10 | Alive |
| 11 | Adenocarcinoma, prostate | Interferon | 61 | 85 | 22 | 130 | 45 | Alive |
| 12 | Adenocarcinoma, prostate | Interferon | 67 | 62 | 13 | 101 | 38 | Alive |
| 13 | Adenocarcinoma, prostate | None | 80 | 58 | 21 | 84 | 26 | Alive |
| 14 | Adenocarcinoma, prostate | None | 72 | 30 | 29 | 62 | 32 | Alive |
| 15 | Metastatic adenocarcinoma, prostate | None | 78 | 1 | 1 | 47 | 46 | Alive |
| 16 | Metastatic adenocarcinoma, prostate | Interferon | 75 | 72 | 11 | 75 | 3 | Dead |
| 17 | Adenocarcinoma, colon (Duke’s B2) | Interferon, Splenectomy | 64 | 125 | 46 | 141 | 16 | Alive |
| 18 | Adenocarcinoma, colon (Duke’s B2) | None | 56 | 30 | 26 | 48 | 17 | Dead |
| 19 | Adenocarcinoma, colon (Duke’s B2) | Splenectomy | 53 | 188 | 1 | 241 | 52 | Alive |
| 20 | Adenocarcinoma, colon (Duke’s C1) | None | 45 | 7 | 5 | 56 | 49 | Alive |
| 21 | Adenocarcinoma, stomach | None | 66 | 62 | 58 | 83 | 21 | Alive |
| 22 | Metastatic adenocarcinoma, stomach | Interferon, splenectomy | 66 | 105 | 31 | 106 | 1 | Dead |
| 23 | Transitional cell carcinoma, bladder | Splenectomy | 65 | 24 | 11 | 75 | 50 | Alive |
| 24 | Renal cell carcinoma | None | 70 | 16 | 15 | 76 | 60 | Alive |
| 25 | Metastatic neuroendocrine tumor, bladder | Splenectomy | 73 | 123 | 41 | 132 | 9 | Dead |
| 26 | Low-grade non-Hodgkin’s lymphoma | None | 71 | 109 | 9 | 19 | 8 | Dead |
| 27 | Cerebellar hemangioblastoma | Splenectomy, interferon | 61 | 80 | 6 | 153 | 73 | Alive |
| Medians | 67 (yr) | 62 (yr) | 21 (mo) | 85 (mo) | 36 (mo) | |||
| (Range) | (45-80) | (1-188) | (1-58) | (19-241) | (1-74) |
Abbreviation: HCL, hairy cell leukemia.
Median age at diagnosis of the second cancer was 67 years (range, 45 to 80 years), median time from diagnosis of hairy cell leukemia to the second cancer was 62 months (range, 1 to 188 months), median time from cladribine administration to the second cancer was 21 months (range, 1 to 58 months), median survival time from diagnosis of hairy cell leukemia was 85 months (range, 19 to 241 months), and median survival time from diagnosis of the second cancer was 36 months (range, 1 to 74 months).
The expected number of second primary tumors in this group of 358 patients is 14.35, based on calculations derived from the National Cancer Institute’s SEER data.17 Second cancers were observed in 27 patients, so the excess frequency (observed-to-expected ratio) was 1.88 (95% confidence interval, 1.24 to 2.74). This represents a small but statistically significant increase in the risk of second cancers.
Of note, 40 patients (median age 58 years; range, 24 to 86 years) had an antecedent diagnosis of malignancy before cladribine; 9 melanoma, 8 adenocarcinoma of the prostate, 5 adenocarcinoma of the colon, 1 adenocarcinoma of the stomach, 9 urogenitary cancers (2 bladder, 3 testes, 1 kidney, 2 cervical, and 1 vulvar neoplasms), 3 infiltrating carcinoma of the breast, 2 thyroid cancer, 1 metastatic basal cell carcinoma, 1 Hodgkin’s disease, and 1 low-grade non-Hodgkin’s lymphoma (small lymphocytic lymphoma). Median time from diagnosis of the second cancer to cladribine was 77 months (range, 1 to 440 months).
Deaths.
Of 358 patients treated, 21 (6%) expired at a median of 39 months (range, 1 to 73 months) after their first cladribine course (Table 6). Seven died of second malignancies or complications of treatment (1 died of pulmonary complications of adriamycin, bleomycin, vinblastine, and dacarbazine chemotherapy administered to treat an antecedent diagnosis of Hodgkin’s disease), 3 of events directly related to hairy cell leukemia, 7 of cardiovascular or cerebrovascular events, 3 of infectious complications, and in 1 the cause of death was unknown. Of these 21 patients, 11 had experienced a prior complete response, 3 a partial response, 5 were scored nonresponders, and 2 were not evaluable for response.
Causes of Death in Hairy Cell Leukemia Patients Following Cladribine
| Causes of Death (No. of Patients) . | Months From First Cladribine Therapy . |
|---|---|
| Second malignancies (7) | |
| Adenocarcinoma of stomach, metastatic | 32 |
| Adenocarcinoma of colon | 44 |
| Melanoma, metastatic | 63 |
| Hodgkin’s disease | 11 |
| Neuroendocrine tumor, bladder | 50 |
| Low-grade non-Hodgkin’s lymphoma | 17 |
| Adenocarcinoma of prostate, metastatic | 14 |
| Hairy cell leukemia (3) | 66, 58, 28 |
| Cardiac or cerebrovascular events (7) | |
| Arrhythmia | 7, 73 |
| Myocardial infarction | 1, 39, 48, 40 |
| Stroke | 63 |
| Infectious complications (3) | |
| Septicemia (Acinetobacter) | 3 |
| Adult respiratory distress syndrome | 12 |
| Septic shock | 1 |
| Unknown (1) | 50 |
| Causes of Death (No. of Patients) . | Months From First Cladribine Therapy . |
|---|---|
| Second malignancies (7) | |
| Adenocarcinoma of stomach, metastatic | 32 |
| Adenocarcinoma of colon | 44 |
| Melanoma, metastatic | 63 |
| Hodgkin’s disease | 11 |
| Neuroendocrine tumor, bladder | 50 |
| Low-grade non-Hodgkin’s lymphoma | 17 |
| Adenocarcinoma of prostate, metastatic | 14 |
| Hairy cell leukemia (3) | 66, 58, 28 |
| Cardiac or cerebrovascular events (7) | |
| Arrhythmia | 7, 73 |
| Myocardial infarction | 1, 39, 48, 40 |
| Stroke | 63 |
| Infectious complications (3) | |
| Septicemia (Acinetobacter) | 3 |
| Adult respiratory distress syndrome | 12 |
| Septic shock | 1 |
| Unknown (1) | 50 |
TTF and overall survival.
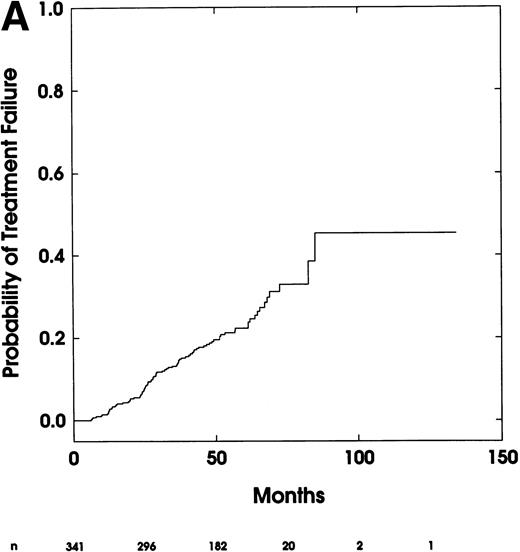
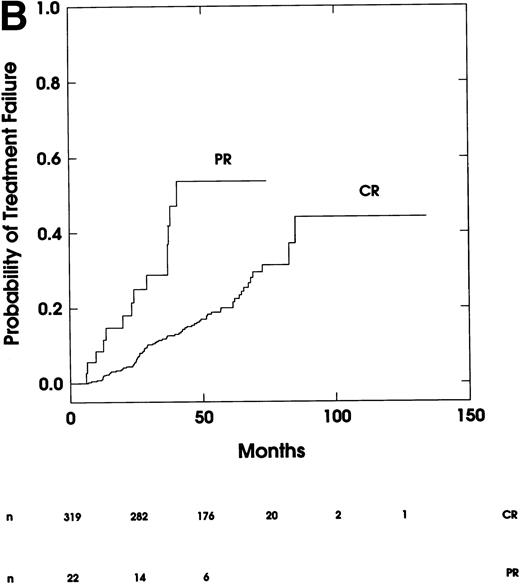
The estimated TTF rate for the 341 responder patients was 6.5% (95% confidence interval, 4.1% to 8.9%) at 24 months and 18.7% (95% confidence interval, 14.6% to 22.6%) at 48 months (Fig 1A). TTF rate for complete responders was 5.2% (95% confidence interval, 3.0% to 7.5%) at 24 months and 16.3% (95% confidence interval, 12.2% to 20.0%) at 48 months (Fig1B). TTF rate for partial responders was 21.5% (95% confidence interval, 5.9% to 34.4%) at 24 months and 53.7% (95% confidence interval, 26.4% to 69.7%) at 48 months (P < 1 × 10-6 by long-rank test; Fig 1B).
(A) Time-to-treatment failure for all 341 patients who achieved a response. (B) Time-to- treatment failure for patients achieving a complete response (CR) or partial response (PR).
(A) Time-to-treatment failure for all 341 patients who achieved a response. (B) Time-to- treatment failure for patients achieving a complete response (CR) or partial response (PR).
After univariate screening, four baseline covariates possibly predictive of TTF were entered into a proportional hazards regression model: white blood cell count, splenomegaly, disease duration, and platelets (in order of increasing significance). The first two factors (white blood cell count >15 × 109/L and presence of splenomegaly) were jointly significant predictors of TTF at the 0.05 level in this multivariate model. Insufficient data were available on all 358 patients to assess minimal residual disease detected by immunohistochemical stains as a risk factor for predicting relapse.18
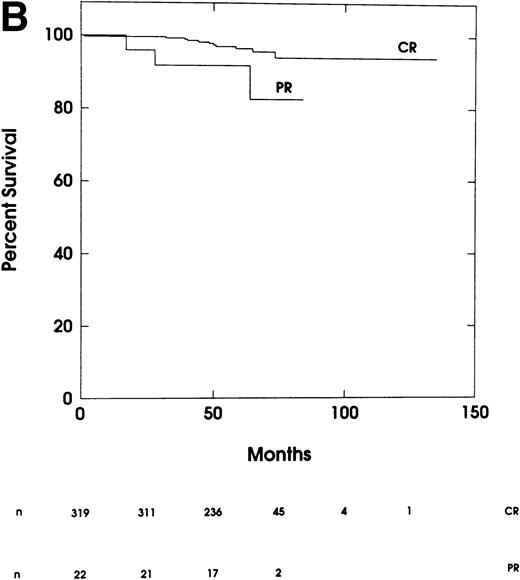
Overall survival rate for all 358 patients was 97.9% (95% confidence interval, 96.2% to 99.3%) at 24 months and 96.0% (95% confidence interval, 93.8% to 98.0%) at 48 months (Fig 2A). Survival for complete responders was 99.7% (95% confidence interval, 99.1% to 100%) at 24 months and 98.3% (95% confidence interval, 96.8% to 99.8%) at 48 months (Fig2B). Survival rate for partial responders was 96.0% (95% confidence interval, 87.1% to 100%) at 24 months and 91.8% (95% confidence interval, 79.7% to 100%) at 48 months (P = .0254 by log- rank test; Fig 2B).
(A) Overall survival for all 358 treated patients. (B) Overall survival for patients achieving a complete response (CR) or partial response (PR).
(A) Overall survival for all 358 treated patients. (B) Overall survival for patients achieving a complete response (CR) or partial response (PR).
In contrast to TTF, seven baseline covariates were somewhat related to survival from univariate screening: white blood cell count, splenectomy, age, TRAP stain, disease duration, immunophenotype, and splenomegaly. From multivariate stepwise Cox regression analysis, white blood cell count (>15 × 109/L) and age (>50 years) were jointly found to be significant predictors of reduced survival (P < .05).
DISCUSSION
This study describes the long-term follow-up of 358 hairy cell leukemia patients treated at Scripps Clinic. These results confirm in a larger group of patients the original report by investigators at Scripps Clinic6 that single courses of cladribine administered to patients with hairy cell leukemia induce a very high response rate, the vast majority of which are complete, durable, and unmaintained. The long-term follow-up now confirms that relapse rates for patients achieving a complete response are generally low, and when they are retreated with second courses of cladribine a second response is typically the result. In addition, these results are achieved with a favorable toxicity profile with culture-negative neutropenic fever being the principal acute toxicity and dermatomal herpes zoster being the most frequent late infection, likely related to the potent immunosuppressive properties of cladribine.19 20 A small, but statistically significant increased incidence of second neoplasms, predominantly solid tumor rather than hematopoietic, was observed. These results were similar to other smaller series reported for both cladribine and 2′-deoxycoformycin.
Tallman et al reported on 50 patients treated with cladribine.4 Overall response rate was 98% (80% complete responses and 18% partial responses), 7 patients (14%) relapsed at a median of 24 months, progression-free survival was 72% at 4 years for all patients and 83% for complete responders, and overall survival rate was 86% at 4 years. Hoffman et al reported on 49 patients treated with cladribine.21 All responded (76% complete and 24% partial responses), relapse-free survival was 80% at 55 months and overall survival was 95%. Comparable long-term results were also achieved with 2’-deoxycoformycin. Kraut et al reported on 24 patients who achieved complete responses after 2′-deoxycoformycin.22Twenty-three patients were alive at a median of 84 months, 11 relapsed at a median of 30 months (7 were retreated with 2′-deoxycoformycin or cladribine and all responded), and median survival from initiation of therapy was 93 months.
A limitation of this study was that the accuracy of the TTF estimates reported was obviously dependent on both the frequency and compliance of the posttreatment marrow samples performed. For example, patients with normal peripheral blood parameters may have had unrecognized marrow relapses. Decreased marrow compliance over time was in part caused by the reluctance of patients, often with the support of their primary oncologists, to undergo regular bone marrow biopsies when marrow relapse in the absence of significant cytopenias or splenomegaly would not have resulted in the need for retreatment. However, bone marrow examinations were repeated earlier for new onset cytopenias to document relapse and before the institution of any chemotherapeutic agent after the single course of cladribine.
Although in this study the TTF rate for complete responders was 16.3% at 4 years, there is no obvious plateau on the TTF curve. Thus, it is unclear what proportion of patients, if any, will be cured. Twenty-five percent to 50% of patients in morphological complete remission after cladribine have minimal residual disease detected by immunohistochemical stains of marrow biopsy specimens.18,23Using the polymerase chain reaction and clonogenic probes derived from the immunoglobulin heavy-chain genes, all seven patients in apparent complete remission after cladribine showed detectable minimal residual disease.24
Optimum therapy for patients who relapse after cladribine remains to be defined. In this study, of 53 patients who received a second course of cladribine at first relapse, 62% achieved complete response and 28% partial response, and of 6 patients who received a third course of cladribine at second relapse, 2 (33%) achieved complete responses and 4 (67%) partial response. For patients treated with interferon or 2′-deoxycoformycin at relapse, higher response rates were documented for 2′-deoxycoformycin-treated patients. Saven and Piro reported on 5 patients who were resistant or intolerant to 2′-deoxycoformycin, 4 of whom achieved complete responses after cladribine. This suggested a possible lack of cross-resistance between cladribine and 2′-deoxycoformycin despite structural and mechanistic similarities between the two agents.25 In small numbers of hairy cell leukemia patients, interferon induced responses after cladribine,26 and in selected patients with persistent splenomegaly and cytopenias after cladribine therapy, splenectomy may be beneficial.
In this report, 27 of the 358 patients (8%) developed second malignancies, which represented an excess frequency of 1.88 in the observed-to-expected ratio when compared with the National Cancer Institute’s SEER data. Because cladribine is powerfully immunosuppressive, reducing CD4 lymphocytes for up to 2 years, it was initially speculated that cladribine might be responsible for an increased incidence of second cancers.19,20,27 In addition, 2-chlorodeoxyadenosine-5′-triphosphate, the phosphorylated and putative active derivative of cladribine (or 2-chlorodeoxyadenosine), impairs DNA synthesis through its preferential use by DNA polymerase and by retardation of DNA chain elongation.28 Its incorporation into the DNA of vulnerable lymphocytes is potentially mutagenic.29 30 It is most intriguing that only 1 of the 27 patients with second malignancies had a hematopoietic cancer (a low-grade non-Hodgkin’s lymphoma), the rest being solid tumors, because prolonged immunosuppression is generally associated with an increased incidence of lymphoid cancers. The cause of the excess frequency of second malignancies is therefore undetermined but may, in part, be related to the age and sex of patients with hairy cell leukemia (for example, elderly males with adenocarcinoma of the prostate gland). Also, it should be noted that 40 patients had an antecedent diagnosis of malignancy before even receiving cladribine. Perhaps patients with hairy cell leukemia have an intrinsic susceptibility to developing second cancers, which is made clinically manifest by the improved survivals for patients with hairy cell leukemia induced by cladribine.
Other investigators have studied the possible causal relationship between the systemic treatments of hairy cell leukemia and the incidence of second malignancies. Kurzrock et al analyzed the incidence of second cancers in 350 hairy cell leukemia patients followed for a median of 6 years.31 Twenty-six patients developed second cancers and there was no excess of malignancy among patients treated with interferon, cladribine, or 2′- deoxycoformycin, but increased numbers of myeloma and lymphoma were observed. Of 979 hairy cell leukemia patients treated with cladribine on the National Cancer Institute group C protocols and followed for a median of 3.4 years, relative risk of cladribine-treated patients developing second cancers was 1.71 (95% confidence interval, 1.24 to 2.30), which represented an increased risk.32 A high incidence of second neoplasms was reported after interferon. Kampmeier et al reported on 69 patients followed for a median of 91 months,33 of whom 13 developed second cancers: 6 hematopoietic and 7 adenocarcinomas. The excess frequency of second cancers was 4.33, which was even greater for hematopoietic neoplasms.
In conclusion, cladribine has emerged as the treatment of choice for hairy cell leukemia given that the overwhelming majority of patients achieve long-lasting complete remissions after only a single 7-day infusion. Patients who relapse can be successfully retreated with cladribine. Longer follow-up of patients is necessary to determine if the slight increase in risk of second malignancies changes over time. The successful application of interferon, 2′-deoxycoformycin, and cladribine has greatly improved survivals of patients with this rare leukemia, which, before the availability of effective systemic therapy, had a median survival of only 53 months.2
Presented in part at the 39th Annual Meeting of the American Society of Hematology, San Diego, CA, December 5- 9, 1997.
Address reprint requests to Alan Saven, MD, Head, Division of Hematology/Oncology, Scripps Clinic, 10666 N Torrey Pines Rd, La Jolla, CA 92037.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" is accordance with 18 U.S.C. section 1734 solely to indicate this fact.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal